Introduction
Trichilemmomas are benign adnexal tumors originating from the hair follicles and were first described by Headington and French in 1962.[1] Trichilemmomas are classified within the spectrum of benign follicular tumors, which encompass a diverse group of uncommon neoplasms originating from various locations within the hair follicle.[2] Trichilemmomas originate from the outer root sheath of the hair follicular unit.[3] Other similar growths originating from this locus include dilated pore of Winer, pilar sheath acanthoma, and pilar cyst, each delineating a unique facet of follicular pathogenesis.[2]
Trichilemmomas often present as asymptomatic, solitary, or multiple verrucous papules, primarily surfacing on the face or neck.[4] When solitary, these lesions can often be clinically misdiagnosed due to their resemblance to other skin conditions, such as verruca vulgaris, verrucous papilloma, basal cell carcinoma, or squamous cell carcinoma, thereby posing diagnostic challenges. However, when a patient presents with numerous trichilemmomas, clinicians should evaluate potential associations with genetic syndromes, notably Cowden syndrome.[5] Trichilemmomas may also be associated with other benign neoplasms such as nevus sebaceous and syringocystadenoma papilliferum.[6][5]
Histopathologically, trichilemmomas exhibit a lobular proliferation extending from the epidermis, characterized by pale-to-clear cells exhibiting peripheral palisading, enveloped by a thickened eosinophilic basement membrane. This is often accompanied by overlying hyperkeratosis and variable papillomatosis.[4] In addition, a desmoplastic variant of trichilemmoma may be present, characterized by infiltrating basaloid cells amidst a thick, sclerotic stroma.[7]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact cause of trichilemmoma remains unknown. Studies have been conducted to investigate a possible association with a viral etiology, such as human papillomavirus (HPV), due to trichilemmoma's clinical and histopathological similarity to a verruca. Although several studies failed to detect HPV within trichilemmoma lesions,[8][9] 1 study successfully identified HPV DNA by polymerase chain reaction in trichilemmomas observed in patients with Cowden syndrome.[10] However, given the conflicting results, the definitive association with a viral cause remains uncertain, underscoring the need for further research to to determine causality.
Epidemiology
The prevalence and incidence of trichilemmomas in the general population are unknown, although cases are considered rare. The true incidence might be higher due to lesions being frequently misdiagnosed. Trichilemmomas are predominantly observed in adults aged between 30 and 80, with a median age of 59, and are uncommon in children.[5][11] They occur across all racial groups, with a slightly higher incidence in males.[11] Approximately 10% to 35% of patients with Cowden syndrome present with multiple trichilemmomas.[5][12]
Histopathology
The histopathological characteristics of trichilemmomas include the following features:
- The epidermis typically displays varying degrees of hyperkeratosis, mild acanthosis, and, in rare occasions, a cutaneous horn. Lesions may exhibit papillomatosis.
- A lobular growth or proliferation extends from the epidermis and projects down into the dermis. Pale-to-clear cells are visible within this proliferation, showing periodic acid-Schiff (PAS)–positive staining due to their glycogen content.
- Cells exhibit peripheral palisading, particularly along the tumor's edges.[4]
- An eosinophilic basement membrane containing hyaline surrounds the tumor. Squamous eddies and areas of keratinization may be seen.
- A desmoplastic variant can be seen, which is characterized by dense, sclerotic collagen throughout the tumor, forming small islands of cells. Due to the dense sclerotic stroma with infiltrating islands of cells, trichilemmomas may mimic infiltrating squamous cell carcinoma or a morphea-like basal cell carcinoma yet typically lack atypia or mitotic activity.[1]
From a histopathological standpoint, various differential diagnoses should be considered. These include verruca vulgaris, basal cell carcinoma, clear cell acanthoma, and squamous cell carcinoma, as well as other benign follicular neoplasms such as tumors of the follicular infundibulum, inverted follicular keratosis, trichoblastoma or trichoepithelioma, and poroma—all of which may resemble a trichilemmoma.
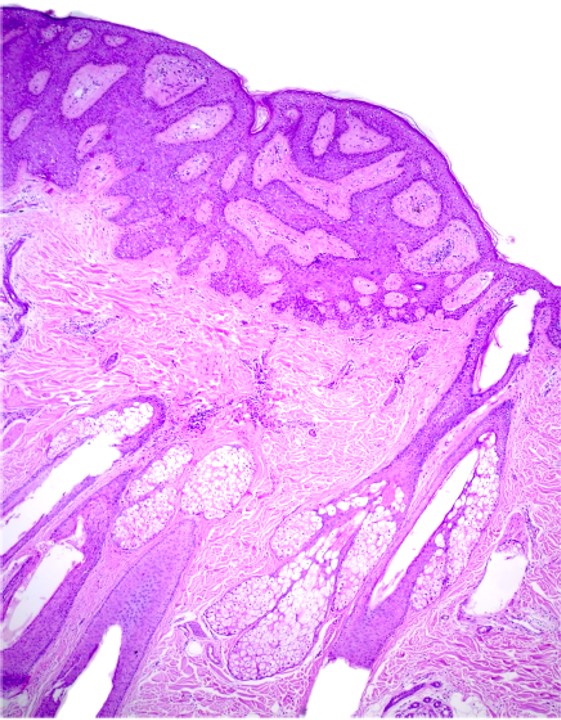
Stains can be useful in the diagnosis of trichilemmomas (see Image. Trichilemmoma Comparison View). A PAS stain is typically positive in trichilemmomas due to the presence of glycogen-filled clear cells, which may also be positive in clear cell acanthoma. However, trichilemmomas can be differentiated by the presence of peripheral palisading and a thick, eosinophilic basement membrane surrounding the tumor. Furthermore, CD34 staining is positive in trichilemmomas and other benign adnexal neoplasms and can aid in distinguishing from basal cell carcinoma or squamous cell carcinoma, particularly in the desmoplastic variant (see Image. Trichilemmoma Histopathological Analysis).[13]
History and Physical
Trichilemmomas typically present as a solitary, pink-to-tan, verrucous papule ranging from 1 to 5 mm in size.[5] A pigmented variant mimicking a pigmented basal cell carcinoma has been reported.[14] Although trichilemmomas are most commonly located on the head and neck, they can also occur at the extrafacial sites, with reports indicating their presence on the eyelid.[1][11] The main clinical differential diagnoses include verruca vulgaris, basal cell carcinoma, squamous cell carcinoma, and benign papillomas. Furthermore, trichilemmomas can be associated with other benign tumors, including nevus sebaceous and syringocystadenoma papilliferum.[6][5] These 2 entities often occur on the scalp but can be located elsewhere.[15]
Desmoplastic trichilemmoma, a rare variant of trichilemmoma, was first described in 1985.[1] Typically, this variant presents as a solitary, asymptomatic papule or nodule, which can be smooth or verrucous in texture. In rare instances, they may be ulcerated, resembling basal cell carcinoma. These papules usually measure between 5 and 7 mm and seldom exceed 10 mm in size. While commonly found on the lip and nose, they can occur elsewhere in the body. Desmoplastic trichilemmomas are slow-growing lesions that have likely been present for many years and are most frequently observed in males aged 50 or older. Concomitant growth with basal cell carcinoma has also been reported.[16]
Evaluation
Trichilemmomas may present clinical similarities to other benign follicular tumors and malignant neoplasms, necessitating a biopsy for accurate diagnosis. The patient may not need further workup or treatment if only one lesion is identified. However, in cases with multiple lesions, the patient should be evaluated for Cowden syndrome.
Cowden syndrome is an autosomal dominant disease caused by a mutation in the phosphatase and tensin homolog (PTEN) gene, which is a tumor suppressor gene. This syndrome is part of a group of associated disorders caused by germline mutations in the PTEN gene, which includes Bannayan-Riley-Ruvalcaba syndrome, Proteus, and Proteus-like syndrome.[12] Cowden syndrome is a rare condition and has an estimated prevalence of 1 in 200,000 live births. This syndrome is characterized by numerous hamartomas and an increased risk of several malignancies, including breast, thyroid, endometrial, renal, colorectal carcinoma, and melanoma.[17] Additionally, individuals with Cowden syndrome may exhibit other associated features such as intestinal polyposis, macrocephaly, scoliosis, and intellectual disability.[12]
By the third decade of life, approximately 99% of patients with Cowden syndrome develop mucocutaneous manifestations of the disease.[17] Trichilemmomas represent the most characteristic lesion of Cowden syndrome, with up to 35% of patients exhibiting numerous trichilemmomas during examination. Other mucocutaneous features associated with this disorder include sclerotic fibromas, acral keratoses, mucocutaneous papillomas, palmoplantar pits, penile hyperpigmentation, neuromas, and lipomas.[12]
If Cowden syndrome is suspected, a referral to a medical geneticist should be promptly initiated for further evaluation. Diagnosis confirmation typically involves identifying a heterozygous germline pathogenic variant in the PTEN gene. If the syndrome is confirmed, management and cancer surveillance should adhere to the National Comprehensive Cancer Network (NCCN) guidelines. This includes performing all age-appropriate cancer screenings and conducting yearly full-body skin examinations.[12]
A recent study has demonstrated promising results in patients with Cowden syndrome by administering daily oral sirolimus—an mTOR inhibitor. This treatment has shown improvement in skin and gastrointestinal lesions, as well as neurological function. The overactivation of the PI3K-Akt-mTOR pathway results from loss of function in the PTEN gene.[18]
Treatment / Management
Trichilemmomas are benign lesions that do not require treatment. However, if lesions are aesthetically displeasing or causing discomfort, surgical excision or carbon dioxide laser therapy can be effective options. Additionally, electrocautery, cryosurgery, or dermabrasion may also be utilized.[5] Similarly, oral and mucocutaneous papillomas associated with Cowden syndrome can be managed with excision or laser treatment. Topical retinoids and salicylic acid have demonstrated some benefits for treating papillomas and acral keratoses.[12]
Mohs micrographic surgery is an effective and satisfactory treatment option for desmoplastic trichilemmomas located on the face, especially considering their potential association with basal cell carcinoma.[19]
Differential Diagnosis
The primary differential diagnosis for trichilemmoma is basal cell carcinoma. Basal cell carcinoma can also present as a smooth to pearly papule on the face, which can sometimes be ulcerated. Histologically, both lesions share similarities, characterized by the presence of basaloid cells and peripheral palisading around the tumor's edge. However, trichilemmomas do not exhibit clefting and lack the fibromyxoid stroma seen in basal cell carcinoma. Staining can be useful in distinguishing these 2 entities. Epithelial cells in trichilemmoma stain positive for CD34, while basal cell carcinoma stains negative. Conversely, BerEP4 staining is positive in basal cell carcinoma and negative in trichilemmomas. Additionally, PAS staining can also help distinguish between these conditions and will be positive only in trichilemmomas.[19]
Squamous cell carcinoma can bear clinical and histological resemblance to trichilemmoma. However, squamous cell carcinoma typically exhibits more diffuse atypia and increased mitotic activity compared to trichilemmoma. Verruca vulgaris also presents a common differential diagnosis. Clinically, verruca vulgaris may be indistinguishable from trichilemmomas. Histopathologically, verruca vulgaris displays acanthosis, papillomatosis, digitated epidermal hyperplasia, and dilated tortuous vessels.
Inverted follicular keratosis also presents as a solitary papule on the face and can display a verrucous or smooth appearance resembling a trichilemmoma. However, histologically, differentiation can be achieved through the presence of squamous eddies, which are diagnostically characteristic of inverted follicular keratosis. Although inverted follicular keratosis may exhibit clear cell change and basaloid cells, they lack the thickened eosinophilic basement membrane observed in trichilemmomas.[4]
Further differential diagnoses include other benign follicular tumors such as trichoblastoma, trichoepithelioma, dilated pore of Winer, pilar sheath acanthoma, poroma, fibrofolliculoma, and trichodiscoma.[12] In addition to Cowden syndrome, multiple facial papules are associated with other inherited genetic syndromes, which may be indistinguishable clinically. Additional syndromes that can result in multiple facial papules are Brooke-Spiegler syndrome, Birt-Hogg-Dubé syndrome, familial multiple trichoepithelioma, tuberous sclerosis, and Muir-Torre syndrome.[12]
Prognosis
Trichilemmomas are typically benign neoplasms, and if they occur as singular lesions, the prognosis is excellent. Surgical excision usually results in a cure. However, in cases of Cowden syndrome, the prognosis depends on the presence and extent of associated malignancies. Fortunately, many of the cancers associated with Cowden syndrome are curable if detected early.
Complications
Solitary trichilemmomas typically do not present complications. However, complications may arise from the treatment modalities, such as surgical excision, laser therapy, or oral treatments, including risks of scarring, infection, or dyspigmentation.
Complications associated with Cowden syndrome primarily stem from the heightened risk of malignancies. Thus, it is crucial to conduct appropriate screenings in accordance with the NCCN guidelines to detect and manage these risks effectively.[12]
Deterrence and Patient Education
In cases of solitary lesions, educational efforts and treatment options tend to be relatively ineffective due to the benign nature of trichilemmoma. Typically, these lesions have minimal impact on quality of life, except for cosmetic concerns. However, if patients present with numerous lesions, healthcare providers should emphasize the possible association with a genetic syndrome and promptly refer them to the appropriate team of specialists for further evaluation. Early referral to genetics is crucial, as the underlying etiology of the disease may significantly impact their quality of life. Thus, educating patients about the benign nature of these lesions and distinguishing them from non-melanoma skin cancers, such as basal cell carcinoma, is crucial.
Enhancing Healthcare Team Outcomes
Histopathological evaluation of cutaneous adnexal neoplasms, such as trichilemmomas, is critical in establishing an accurate diagnosis and guiding subsequent management and treatment strategies. Given the similarities in clinical and histological presentation with both benign and malignant neoplasms, a biopsy is frequently necessary to clarify the diagnosis. A biopsy helps distinguish between benign and malignant lesions, such as basal or squamous cell carcinoma, which may require more extensive treatment regimens, including surgical excision or Mohs micrographic surgery. Avoiding misdiagnosis is essential in preventing further morbidity.
Providers should routinely examine patients for any new or enlarging lesions. If a lesion on the neck or face persists for more than 6 weeks without spontaneous resolution, a biopsy should be conducted. In cases where histopathology confirms a diagnosis of trichilemmoma, and there is suspicion of Cowden syndrome, patients should be promptly referred for additional genetic workup.[5]
Media
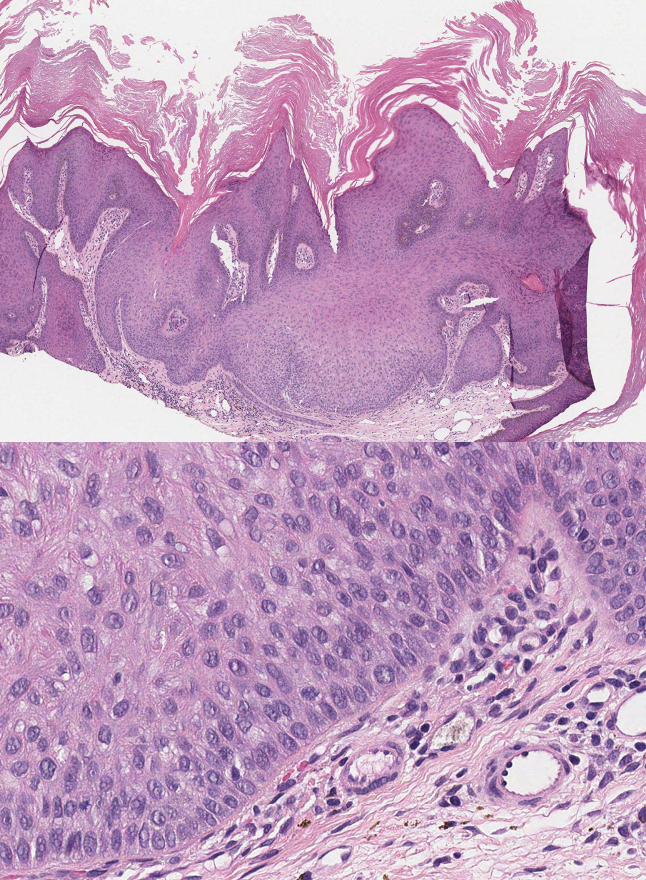
(Click Image to Enlarge)
Trichilemmoma Histopathological Analysis. Sections examined reveal a folliculocentric tumor with a connection to the epidermis. The tumor consists of pale eosinophilic cytoplasm cells, some exhibiting clear cell differentiation. Prominent peripheral palisading and reverse polarity of nuclei within the peripheral cells are observed, resting on a thickened basement membrane. Foci of keratinization are evident within the tumor. Stromal clefting is also observed in the dermis. Dysplasia could not be identified. (Hematoxylin and eosin staining, original magnification x40.)
Contributed by M Abdel-Halim Ibrahim, MD
References
Pihlblad M, Chelnis J, Schaefer D. Eyelid desmoplastic trichilemmoma: 2 case reports and review. Ophthalmic plastic and reconstructive surgery. 2014 Sep-Oct:30(5):e136-8. doi: 10.1097/IOP.0b013e3182a65067. Epub [PubMed PMID: 24777258]
Level 3 (low-level) evidenceTellechea O, Cardoso JC, Reis JP, Ramos L, Gameiro AR, Coutinho I, Baptista AP. Benign follicular tumors. Anais brasileiros de dermatologia. 2015 Nov-Dec:90(6):780-96; quiz 797-8. doi: 10.1590/abd1806-4841.20154114. Epub [PubMed PMID: 26734858]
Chan P, White SW, Pierson DL, Rodman OG. Trichilemmoma. The Journal of dermatologic surgery and oncology. 1979 Jan:5(1):58-9 [PubMed PMID: 759462]
Maher EE, Vidal CI. Trichilemmoma. Cutis. 2015 Aug:96(2):81, 104-6 [PubMed PMID: 26367753]
Ng DW. Trichilemmoma in Childhood. Journal of pediatric health care : official publication of National Association of Pediatric Nurse Associates & Practitioners. 2016 Sep-Oct:30(5):491-4. doi: 10.1016/j.pedhc.2016.06.001. Epub 2016 Jun 29 [PubMed PMID: 27372178]
Alqahtani J, Al-Natour SH. Trichilemmoma Arising in a Sebaceous Nevus Successfully Treated with Cryotherapy. Clinical, cosmetic and investigational dermatology. 2022:15():185-188. doi: 10.2147/CCID.S351033. Epub 2022 Feb 7 [PubMed PMID: 35173451]
Tellechea O, Reis JP, Baptista AP. Desmoplastic trichilemmoma. The American Journal of dermatopathology. 1992 Apr:14(2):107-4 [PubMed PMID: 1373583]
Brownstein MH. Trichilemmoma. Benign follicular tumor or viral wart? The American Journal of dermatopathology. 1980 Fall:2(3):229-31 [PubMed PMID: 7258555]
Stierman S, Chen S, Nuovo G, Thomas J. Detection of human papillomavirus infection in trichilemmomas and verrucae using in situ hybridization. Journal of cutaneous pathology. 2010 Jan:37(1):75-80. doi: 10.1111/j.1600-0560.2009.01348.x. Epub 2009 Jul 13 [PubMed PMID: 19615037]
Schaller J, Rohwedder A, Burgdorf WH, Itin PH, Lautenschlager S. Identification of human papillomavirus DNA in cutaneous lesions of Cowden syndrome. Dermatology (Basel, Switzerland). 2003:207(2):134-40 [PubMed PMID: 12920361]
Jakobiec FA, Stagner AM, Sassoon J, Goldstein S, Mihm MC. A Hyalinized Trichilemmoma of the Eyelid in a Teenager. Ophthalmic plastic and reconstructive surgery. 2016 Jan-Feb:32(1):e9-e12. doi: 10.1097/IOP.0000000000000389. Epub [PubMed PMID: 26020717]
Lim A, Ngeow J. The Skin in Cowden Syndrome. Frontiers in medicine. 2021:8():658842. doi: 10.3389/fmed.2021.658842. Epub 2021 Jun 10 [PubMed PMID: 34179044]
Rao AG, Reddy VS, Tejal M, Divya M. Trichilemmoma Coexisting with Sebaceous Nevus. Indian dermatology online journal. 2020 Mar-Apr:11(2):253-255. doi: 10.4103/idoj.IDOJ_91_19. Epub 2020 Mar 9 [PubMed PMID: 32477993]
Behera B, Srinivas BH, Kumari R, Thappa DM, Ayyanar P. Pigmented trichilemmoma: A potential mimicker. The Australasian journal of dermatology. 2021 Aug:62(3):e462-e464. doi: 10.1111/ajd.13622. Epub 2021 May 10 [PubMed PMID: 33970491]
Castilla EA, Bergfeld WF, Ormsby A. Trichilemmoma and syringocystadenoma papilliferum arising in naevus sebaceous. Pathology. 2002 Apr:34(2):196-7 [PubMed PMID: 12009106]
Zhong S, Wang L, Mei XL. Desmoplastic trichilemmoma of the scalp: case report and literature review of immunohistochemical staining features. The Journal of international medical research. 2019 Aug:47(8):3918-3925. doi: 10.1177/0300060519859739. Epub 2019 Jul 15 [PubMed PMID: 31304849]
Level 3 (low-level) evidenceMasmoudi A, Chermi ZM, Marrekchi S, Raida BS, Boudaya S, Mseddi M, Jalel MT, Turki H. Cowden syndrome. Journal of dermatological case reports. 2011 Mar 26:5(1):8-13. doi: 10.3315/jdcr.2011.1063. Epub [PubMed PMID: 21886759]
Level 3 (low-level) evidenceKomiya T, Blumenthal GM, DeChowdhury R, Fioravanti S, Ballas MS, Morris J, Hornyak TJ, Wank S, Hewitt SM, Morrow B, Memmott RM, Rajan A, Dennis PA. A Pilot Study of Sirolimus in Subjects with Cowden Syndrome or Other Syndromes Characterized by Germline Mutations in PTEN. The oncologist. 2019 Dec:24(12):1510-e1265. doi: 10.1634/theoncologist.2019-0514. Epub 2019 Jul 26 [PubMed PMID: 31350329]
Level 3 (low-level) evidenceAfshar M, Lee RA, Jiang SI. Desmoplastic trichilemmoma--a report of successful treatment with Mohs micrographic surgery and a review and update of the literature. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2012 Nov:38(11):1867-71. doi: 10.1111/j.1524-4725.2012.02514.x. Epub 2012 Jul 17 [PubMed PMID: 22805188]