Introduction
Monocytes are white blood cells that derive from the bone marrow. A monocyte is part of the innate immune response and functions to regulate cellular homeostasis, especially in the setting of infection and inflammation.[1] They account for approximately 5% of circulating nucleated cells in normal adult blood.[2] The half-life of circulating monocytes is approximately one to three days.[3] Monocytopenia, a decrease in circulating monocytes, is a common finding in myelodysplastic syndromes.[4] While monocytosis, an increase in circulating monocytes, is a common finding in the peripheral blood, especially in association with infection, trauma, medications, autoimmune disease, and some malignancies.[1] When monocytosis is persistent and unexplained, the diagnosis of chronic myelomonocytic leukemia merits investigation.[5]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
When there is a suspected myeloid neoplasm with monocytic differentiation, it is challenging and essential to accurately classify monocytes as mature or immature. There is no definitive test to identify immature monocytes. Flow cytometry identifies molecules on the surface of such cells, known as cluster of differentiation (CD) markers. Such markers can provide information to help in estimating the approximate populations of mature and immature monocytes.[6] Along with flow cytometry, the cell’s morphology requires assessment due to the atypical expression of CD markers during neoplastic growth.[5] In chronic myelomonocytic leukemia, there is persistent peripheral blood monocytosis with approximately double the amount of normally circulating monocytes.[5] The bone marrow must have less than 20% blasts (immature cells) present for the clinician to render a diagnosis of chronic myelomonocytic leukemia.[7]
Structure
Monocytes are the largest white blood cell, measuring between 12 to 20 µm in diameter, approximately twice the size of red blood cells.[2] Monocytes are typically easy to identify in the peripheral blood by their relatively large size and convoluted bilobed nuclei, often described as kidney-shaped.[8]
Function
Monocytes are a crucial component of the innate immune system.[9] A monocyte is a type of white blood cell that differentiates into populations of macrophages and dendritic cells to regulate cellular homeostasis, especially in the setting of infection and inflammation.[1] Monocytes have two distinct roles; they regularly patrol the body for microbial cells and orchestrate an immune response in times of infection and inflammation.[1] Monocytes have toll-like receptors on their surfaces that interact with PAMPS (pathogen-associated molecular patterns) found on invading microbial cells.[10] In response to such stimuli, monocytes migrate from the bone marrow into the blood circulation and infiltrate tissues within 12 to 24 hours.[11]
To infiltrate the affected sites, the monocytes must first secure themselves to the endothelium and then loosely roll along the vascular surface. The monocyte then firmly adheres to the endothelium and finally passes through the endothelial cells through a process known as diapedesis. Monocytes are then able to penetrate the endothelial basement membrane and migrate to the area of inflammation.[12] This process occurs through the interaction of molecules on both the monocyte and the endothelial cell surfaces.[13] Growth factors and cytokines determine the monocyte subtype.[14] Monocytes function as phagocytes and antigen-presenting cells in the peripheral blood to ingest and remove microorganisms, foreign material, and dead or damaged cells.[1] Antigen-presenting cells include macrophages, dendritic cells, B lymphocytes, and activated endothelial cells.[15]
Macrophages can further differentiate into specialized macrophages based on their location.[16] These include histiocytes in the connective tissue, microglia cells in the brain, osteoclast in the bone, mesangial cells in the kidney, and alveolar macrophages in the lungs.[17] Monocytes can produce cytokines that recruit additional cells and proteins to the affected area mounting a substantial immune response.[1] The types of cytokines released will vary depending on the function.[18] To restore homeostasis, monocytes can contribute to remodeling and healing via anti-inflammatory cytokines.[18]
Tissue Preparation
The histological characterizing of monocytes occurs in three main steps. These steps include obtaining and preparing a sample of whole blood, flow cytometry, and monocyte gating. The process of preparing the whole blood is a multistep chemical procedure that involves lysing the cells, marking the cells, and ultimately obtaining a concentrated sample for use in the study. Flow cytometry of the sample then allows for the characterizing of the monocytes depending on the markers they process. Monocyte gating is a visual means by which to organize the collected data to show the percentage of each monocyte subset.[19]
Histochemistry and Cytochemistry
The cluster of differentiation (CD) markers are specific molecules found on the surface of a cell that differentiates cells from one another, as well as from surrounding tissue. The CD markers are specific to the subtype of monocyte and the type of response mounted by the immune system.[6] Common CD markers include CD4, CD11b, CD14, CD16, and CD33.[20]
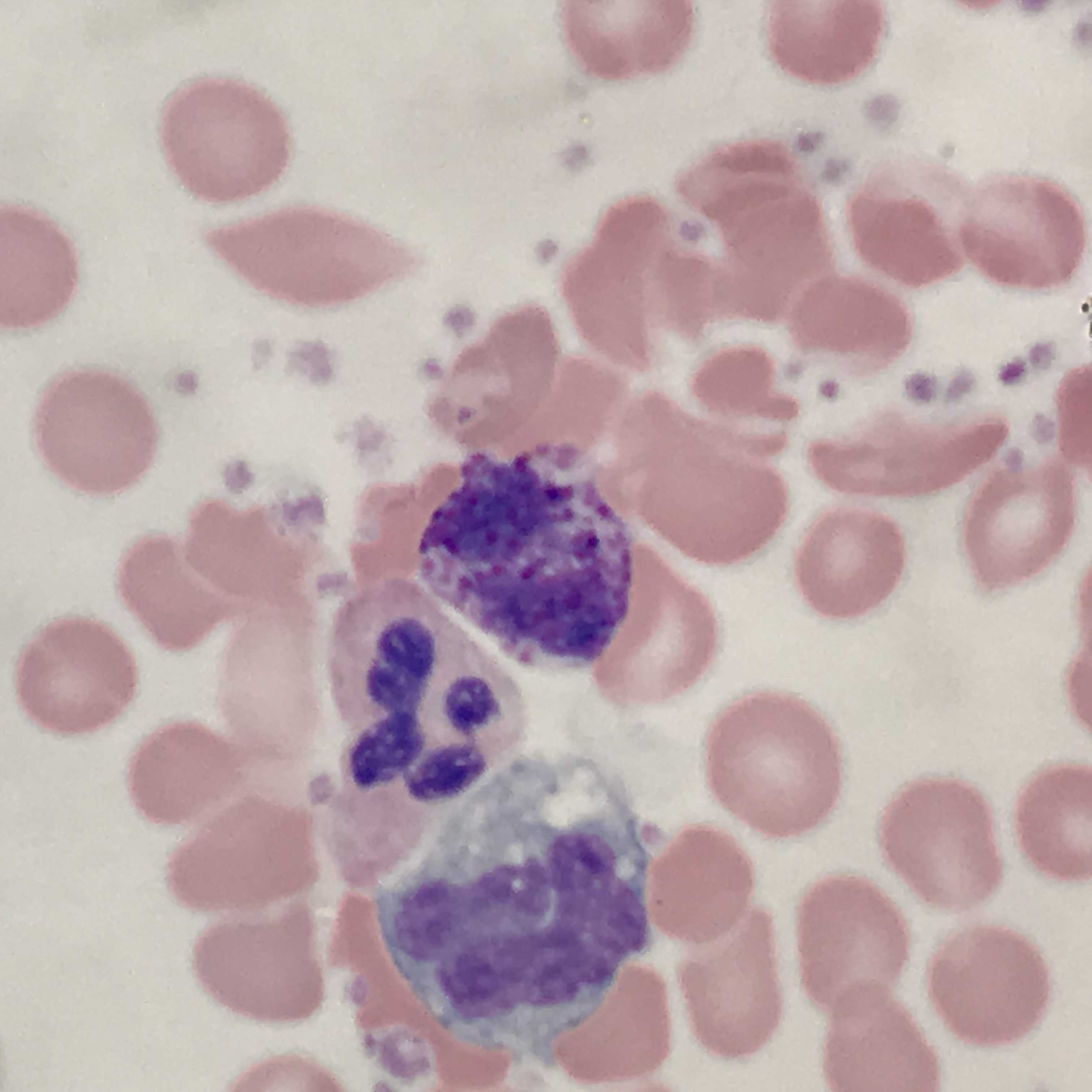
Microscopy, Light
The single bi-lobed nucleus has mature chromatin, and the cytoplasm is moderate to abundant and frequently shows irregular basophilic edges. Upon staining with non-specific esterases, the nucleus is pale violet, while the abundant cytoplasm stains pale grey to blue with numerous reddish-blue cytoplasmic granules.[2]
Microscopy, Electron
On electron microscopy, monocytes appear to have a single nucleus and abundant cytoplasm with scattered granules as well as organelles. Such organelles include numerous mitochondria, a Golgi apparatus, microvesicles, microtubules, and microfilaments.[21]
Pathophysiology
The role of monocytes is versatile and related to various types of disorders and infectious processes, and inflammation. Monocytosis and monocytopenia have been identifying factors in multiple hematologic disorders, such as leukemias and myelodysplastic syndromes.[22] Monocytosis is present in numerous inflammatory and immune disorders, such as connective tissue diseases, such as rheumatoid arthritis, systemic lupus erythematosus, and sarcoidosis.[23][24][25] Monocytes play a crucial role in the immune response to acute infectious and inflammatory processes, such as mycobacterial infections and varicella-zoster virus.[26][27] Monocytosis also occurs in myocardial infarction and is often related to the serum creatinine kinase and extent of infarction.[28] Monocytes can remove the debris and help with remodeling following myocardial infarctions.[29]
Clinical Significance
Monocytes are a critical component of the innate immune system. They are the source of many other vital elements of the immune system, such as macrophages and dendritic cells. Monocytes play a role in both the inflammatory and anti-inflammatory processes that take place during an immune response. Monocytes, and their abundance or lack thereof, can provide significant identifying clues for the diagnosis of several hematologic disorders and inflammatory and immune disorders.
Media
(Click Image to Enlarge)
References
Yáñez A, Coetzee SG, Olsson A, Muench DE, Berman BP, Hazelett DJ, Salomonis N, Grimes HL, Goodridge HS. Granulocyte-Monocyte Progenitors and Monocyte-Dendritic Cell Progenitors Independently Produce Functionally Distinct Monocytes. Immunity. 2017 Nov 21:47(5):890-902.e4. doi: 10.1016/j.immuni.2017.10.021. Epub [PubMed PMID: 29166589]
Prinyakupt J, Pluempitiwiriyawej C. Segmentation of white blood cells and comparison of cell morphology by linear and naïve Bayes classifiers. Biomedical engineering online. 2015 Jun 30:14():63. doi: 10.1186/s12938-015-0037-1. Epub 2015 Jun 30 [PubMed PMID: 26123131]
Patel AA, Zhang Y, Fullerton JN, Boelen L, Rongvaux A, Maini AA, Bigley V, Flavell RA, Gilroy DW, Asquith B, Macallan D, Yona S. The fate and lifespan of human monocyte subsets in steady state and systemic inflammation. The Journal of experimental medicine. 2017 Jul 3:214(7):1913-1923. doi: 10.1084/jem.20170355. Epub 2017 Jun 12 [PubMed PMID: 28606987]
Saeed L, Patnaik MM, Begna KH, Al-Kali A, Litzow MR, Hanson CA, Ketterling RP, Porrata LF, Pardanani A, Gangat N, Tefferi A. Prognostic relevance of lymphocytopenia, monocytopenia and lymphocyte-to-monocyte ratio in primary myelodysplastic syndromes: a single center experience in 889 patients. Blood cancer journal. 2017 Mar 31:7(3):e550. doi: 10.1038/bcj.2017.30. Epub 2017 Mar 31 [PubMed PMID: 28362440]
Itzykson R, Fenaux P, Bowen D, Cross NCP, Cortes J, De Witte T, Germing U, Onida F, Padron E, Platzbecker U, Santini V, Sanz GF, Solary E, Van de Loosdrecht A, Malcovati L. Diagnosis and Treatment of Chronic Myelomonocytic Leukemias in Adults: Recommendations From the European Hematology Association and the European LeukemiaNet. HemaSphere. 2018 Dec:2(6):e150. doi: 10.1097/HS9.0000000000000150. Epub 2018 Nov 29 [PubMed PMID: 31723789]
Hamers AAJ, Dinh HQ, Thomas GD, Marcovecchio P, Blatchley A, Nakao CS, Kim C, McSkimming C, Taylor AM, Nguyen AT, McNamara CA, Hedrick CC. Human Monocyte Heterogeneity as Revealed by High-Dimensional Mass Cytometry. Arteriosclerosis, thrombosis, and vascular biology. 2019 Jan:39(1):25-36. doi: 10.1161/ATVBAHA.118.311022. Epub [PubMed PMID: 30580568]
Tcyganov E, Mastio J, Chen E, Gabrilovich DI. Plasticity of myeloid-derived suppressor cells in cancer. Current opinion in immunology. 2018 Apr:51():76-82. doi: 10.1016/j.coi.2018.03.009. Epub 2018 Mar 14 [PubMed PMID: 29547768]
Level 3 (low-level) evidenceSkinner BM, Johnson EE. Nuclear morphologies: their diversity and functional relevance. Chromosoma. 2017 Mar:126(2):195-212. doi: 10.1007/s00412-016-0614-5. Epub 2016 Sep 8 [PubMed PMID: 27631793]
Auffray C, Sieweke MH, Geissmann F. Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annual review of immunology. 2009:27():669-92. doi: 10.1146/annurev.immunol.021908.132557. Epub [PubMed PMID: 19132917]
Level 3 (low-level) evidenceSantoni G, Cardinali C, Morelli MB, Santoni M, Nabissi M, Amantini C. Danger- and pathogen-associated molecular patterns recognition by pattern-recognition receptors and ion channels of the transient receptor potential family triggers the inflammasome activation in immune cells and sensory neurons. Journal of neuroinflammation. 2015 Feb 3:12():21. doi: 10.1186/s12974-015-0239-2. Epub 2015 Feb 3 [PubMed PMID: 25644504]
Level 3 (low-level) evidenceIssekutz AC, Issekutz TB. Quantitation and kinetics of blood monocyte migration to acute inflammatory reactions, and IL-1 alpha, tumor necrosis factor-alpha, and IFN-gamma. Journal of immunology (Baltimore, Md. : 1950). 1993 Aug 15:151(4):2105-15 [PubMed PMID: 8345197]
Level 3 (low-level) evidenceMaslin CL, Kedzierska K, Webster NL, Muller WA, Crowe SM. Transendothelial migration of monocytes: the underlying molecular mechanisms and consequences of HIV-1 infection. Current HIV research. 2005 Oct:3(4):303-17 [PubMed PMID: 16250878]
Level 3 (low-level) evidenceHenderson RB, Hobbs JA, Mathies M, Hogg N. Rapid recruitment of inflammatory monocytes is independent of neutrophil migration. Blood. 2003 Jul 1:102(1):328-35 [PubMed PMID: 12623845]
Level 3 (low-level) evidenceBoyette LB, Macedo C, Hadi K, Elinoff BD, Walters JT, Ramaswami B, Chalasani G, Taboas JM, Lakkis FG, Metes DM. Phenotype, function, and differentiation potential of human monocyte subsets. PloS one. 2017:12(4):e0176460. doi: 10.1371/journal.pone.0176460. Epub 2017 Apr 26 [PubMed PMID: 28445506]
Jakubzick CV, Randolph GJ, Henson PM. Monocyte differentiation and antigen-presenting functions. Nature reviews. Immunology. 2017 Jun:17(6):349-362. doi: 10.1038/nri.2017.28. Epub 2017 Apr 24 [PubMed PMID: 28436425]
Varol C, Yona S, Jung S. Origins and tissue-context-dependent fates of blood monocytes. Immunology and cell biology. 2009 Jan:87(1):30-8. doi: 10.1038/icb.2008.90. Epub 2008 Dec 2 [PubMed PMID: 19048016]
Level 3 (low-level) evidenceSchultze JL. Chromatin Remodeling in Monocyte and Macrophage Activation. Advances in protein chemistry and structural biology. 2017:106():1-15. doi: 10.1016/bs.apcsb.2016.09.001. Epub 2016 Oct 18 [PubMed PMID: 28057208]
Level 3 (low-level) evidenceYang J, Zhang L, Yu C, Yang XF, Wang H. Monocyte and macrophage differentiation: circulation inflammatory monocyte as biomarker for inflammatory diseases. Biomarker research. 2014 Jan 7:2(1):1. doi: 10.1186/2050-7771-2-1. Epub 2014 Jan 7 [PubMed PMID: 24398220]
Marimuthu R, Francis H, Dervish S, Li SCH, Medbury H, Williams H. Characterization of Human Monocyte Subsets by Whole Blood Flow Cytometry Analysis. Journal of visualized experiments : JoVE. 2018 Oct 17:(140):. doi: 10.3791/57941. Epub 2018 Oct 17 [PubMed PMID: 30394370]
Stansfield BK, Ingram DA. Clinical significance of monocyte heterogeneity. Clinical and translational medicine. 2015:4():5. doi: 10.1186/s40169-014-0040-3. Epub 2015 Feb 14 [PubMed PMID: 25852821]
Puhm F, Afonyushkin T, Resch U, Obermayer G, Rohde M, Penz T, Schuster M, Wagner G, Rendeiro AF, Melki I, Kaun C, Wojta J, Bock C, Jilma B, Mackman N, Boilard E, Binder CJ. Mitochondria Are a Subset of Extracellular Vesicles Released by Activated Monocytes and Induce Type I IFN and TNF Responses in Endothelial Cells. Circulation research. 2019 Jun 21:125(1):43-52. doi: 10.1161/CIRCRESAHA.118.314601. Epub 2019 May 8 [PubMed PMID: 31219742]
Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer. Journal of leukocyte biology. 2019 Aug:106(2):309-322. doi: 10.1002/JLB.4RI0818-311R. Epub 2019 Feb 18 [PubMed PMID: 30776148]
Roberts CA, Dickinson AK, Taams LS. The Interplay Between Monocytes/Macrophages and CD4(+) T Cell Subsets in Rheumatoid Arthritis. Frontiers in immunology. 2015:6():571. doi: 10.3389/fimmu.2015.00571. Epub 2015 Nov 19 [PubMed PMID: 26635790]
Burbano C, Villar-Vesga J, Orejuela J, Muñoz C, Vanegas A, Vásquez G, Rojas M, Castaño D. Potential Involvement of Platelet-Derived Microparticles and Microparticles Forming Immune Complexes during Monocyte Activation in Patients with Systemic Lupus Erythematosus. Frontiers in immunology. 2018:9():322. doi: 10.3389/fimmu.2018.00322. Epub 2018 Mar 1 [PubMed PMID: 29545790]
Fraser SD, Sadofsky LR, Kaye PM, Hart SP. Reduced expression of monocyte CD200R is associated with enhanced proinflammatory cytokine production in sarcoidosis. Scientific reports. 2016 Dec 8:6():38689. doi: 10.1038/srep38689. Epub 2016 Dec 8 [PubMed PMID: 27929051]
Delcroix M, Heydari K, Dodge R, Riley LW. Flow-cytometric analysis of human monocyte subsets targeted by Mycobacterium bovis BCG before granuloma formation. Pathogens and disease. 2018 Nov 1:76(8):. doi: 10.1093/femspd/fty080. Epub 2018 Nov 1 [PubMed PMID: 30445573]
Kennedy JJ, Steain M, Slobedman B, Abendroth A. Infection and Functional Modulation of Human Monocytes and Macrophages by Varicella-Zoster Virus. Journal of virology. 2019 Feb 1:93(3):. doi: 10.1128/JVI.01887-18. Epub 2019 Jan 17 [PubMed PMID: 30404793]
Nahrendorf M, Pittet MJ, Swirski FK. Monocytes: protagonists of infarct inflammation and repair after myocardial infarction. Circulation. 2010 Jun 8:121(22):2437-45. doi: 10.1161/CIRCULATIONAHA.109.916346. Epub [PubMed PMID: 20530020]
Level 3 (low-level) evidenceDutta P, Nahrendorf M. Monocytes in myocardial infarction. Arteriosclerosis, thrombosis, and vascular biology. 2015 May:35(5):1066-70. doi: 10.1161/ATVBAHA.114.304652. Epub 2015 Mar 19 [PubMed PMID: 25792449]