Anatomy, Bony Pelvis and Lower Limb: Superficial Peroneal Nerve (Superficial Fibular Nerve)
Anatomy, Bony Pelvis and Lower Limb: Superficial Peroneal Nerve (Superficial Fibular Nerve)
Introduction
The superficial peroneal nerve, also known as the superficial fibular nerve, originates from the common peroneal nerve alongside the deep peroneal nerve. The superficial peroneal nerve is the smaller of the two common peroneal nerve branches.[1]
The common peroneal nerve comprises fibers from spinal nerves L4 through S1. The common peroneal nerve branches out from the sciatic nerve, which is composed of nerve fibers from spinal nerves L4 through S3.
The sciatic nerve terminates at the apex of the popliteal fossa, bifurcating into the common peroneal and tibial nerves as it wraps around the fibular neck.[2][3]
After diverging from the common peroneal nerve, the superficial peroneal nerve courses through the peroneus longus muscle.[1] The superficial peroneal nerve provides motor stimulation to the peroneus longus and peroneus brevis muscles (see Image, Lower Limb, Peroneal Nerve).[1]
The superficial peroneal nerve exits the peroneal muscles on the anterolateral aspect of the lower leg, approximately 12 cm above the ankle joint, at a defect in the crural fascia (aka "deep fascia of the leg").[1]
The medial and intermediate dorsal cutaneous nerves emerge inferiorly from the superficial peroneal nerve. The medial dorsal cutaneous nerve is the larger of the two. These nerves provide sensory innervation to the leg's anterolateral aspect, the dorsum of the foot, and the dorsal aspect of the toes, except the 1st interdigital space,[1] which is innervated by the deep peroneal nerve (see Image. Superficial Peroneal Nerve Block).[4]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The superficial peroneal nerve has both motor and sensory components. The motor fibers innervate the leg's lateral compartment muscles, the peroneus longus and peroneus brevis. Motor stimulation of these muscles is primarily responsible for eversion and mild plantar flexion of the foot.[5] The peroneus longus tendon is a structure that helps support the arch of the foot.[6][5]
The medial and intermediate dorsal cutaneous nerves are the terminal branches of the superficial peroneal nerve. These nerves supply sensory branches to the dorsum of the foot, except the 1st web space, which is innervated by the deep peroneal nerve.[1][4]
Blood Supply and Lymphatics
The part of the superficial peroneal nerve that lies within the leg's lateral compartment is supplied by the fibular and posterior tibial arteries.[1] However, the part that continues to the dorsum of the foot receives blood from the anterior tibial artery.[7][8][9]
The superficial peroneal nerve often runs alongside small perforating cutaneous arteries from the anterior tibial artery, including the superficial peroneal nerve accessory artery. This structural arrangement enables the creation of superficial peroneal neurocutaneous island flaps—or skin segments retaining portions of the superficial peroneal nerve—used in skin grafting and foot reconstruction procedures.[7][8][9] However, some individuals lack the superficial peroneal nerve accessory artery.[8]
Nerves
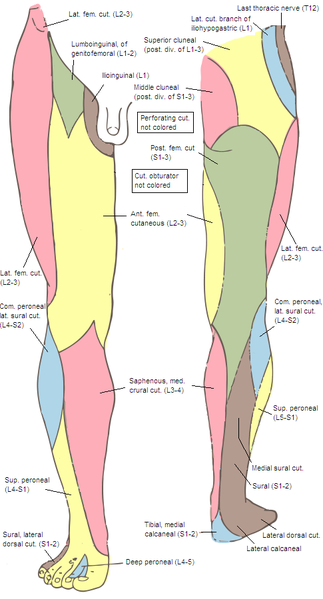
Sensory Nerves of the Leg and Foot
The superficial peroneal nerve supplies the lateral leg and dorsal foot.
The saphenous nerve, the terminal branch of the femoral nerve, innervates the medial leg and malleolar areas.
The sural nerve, formed by connecting branches of the tibial and common peroneal nerves, supplies the leg's posterolateral aspect and the foot's lateral side.
The tibial nerve arises from the sciatic nerve and provides motor stimulation to the posterior muscles of the knee joint and leg. In the foot, the tibial nerve divides into the medial and lateral plantar nerves, which have both motor and sensory functions. The medial plantar nerve supplies the skin and muscles on the medial aspect of the sole. The lateral plantar nerve innervates the skin and muscles on the lateral side of the sole.
Muscles
The superficial peroneal nerve supplies motor innervation to the following muscles:
- Peroneus longus, ie, fibularis longus
- Peroneus brevis, ie, fibularis brevis
The peroneus longus arises from the head and superior two-thirds of the lateral side of the fibula. The peroneus longus is located within the leg's lateral compartment, passing posterior to the lateral malleolus, where it can be palpated. The peroneus longus then enters a groove on the cuboid bone, crossing the plantar foot surface and inserting on the lateral aspect of the 1st metatarsal and medial cuneiform bones. The peroneus longus helps to stabilize the leg on the foot when a person stands on one foot.
The peroneus brevis lies deep and inferior to the peroneus longus in the lateral compartment of the leg. It passes posterior to the lateral malleolus, inserting on the base of the 5th metatarsal.
The lateral compartment of the leg is innervated by the superficial peroneal nerve, which has the following functions:
- Supplies motor impulses to the peroneus longus and peroneus brevis muscles
- Collects sensory information from the anterior leg and almost the entire foot dorsum.
A clinically important exception to this pattern is the skin between the first two digits, as numbness or altered sensation in this area is attributed to deep peroneal nerve damage.
Physiologic Variants
The superficial peroneal nerve can pierce the crural fascia in different ways, and a few variants have been identified.[10][11][12]
In type 1, which is the most common, the nerve pierces the crural fascial before bifurcating into the medial and intermediate dorsal cutaneous nerves. The type 1 variant appears in approximately 82.7% of individuals.[10]
In type 2, the superficial peroneal nerve bifurcates even before it pierces the crural fascia so that the medial and intermediate dorsal cutaneous nerves exit the fascia as separate structures. Around 15.6% of the population exhibits the type 2 variant.[10]
In type 3, the superficial peroneal nerve does not split into 2 but instead exits the crural fascia only as the medial dorsal cutaneous nerve, with the intermediate dorsal cutaneous nerve absent. The type 3 variant is present in 1.8% of individuals.[10]
Besides fascial piercing, the superficial peroneal nerve's location also varies individually. The superficial peroneal nerve is typically found in the lateral leg compartment. However, a study in India revealed that 28.3% of cadaveric specimens had the superficial peroneal nerve situated in the anterior compartment.[11]
Surgical Considerations
The superficial peroneal nerve is the only nerve that can be visualized in the human body without dissection. Foot dorsum examination and simple maneuvers like plantar flexion and ankle inversion can make the superficial peroneal nerve more prominent.[13][14][15] Regardless, superficial peroneal nerve damage is the most commonly reported complication when performing anterior ankle arthroscopy, likely because this procedure is typically performed in the neutral or slightly dorsiflexed position rather than the plantarflexed and inverted position.[14] Anterior ankle arthroscopy complication rates are as high as 17%, and more than 25% of the cases are related to superficial peroneal nerve damage.[13] Preoperatively visualizing the nerve and marking its course on the skin are recommended to avoid damage.[14][16]
The presence of a rare superficial peroneal nerve branching pattern variant must also be determined before a surgical procedure to prevent iatrogenic injuries. The intermediate dorsal cutaneous nerve is highly at risk when it passes lateral to the distal fibula or near the fibula's anterior border. The intermediate and medial dorsal cutaneous nerves passing at the ankle level are at risk when performing an anterior ankle arthrotomy or arthroscopy.[12]
Clinical Significance
Superficial Peroneal Nerve Entrapment
Injury to the superficial peroneal nerve diminishes the ability to evert the foot.[1] Additionally, the foot dorsum exhibits loss of sensation, except in the web space between the first two digits, which is innervated by the deep peroneal nerve.[1][4] Common peroneal nerve damage resulting from a blow to the lateral side of the knee or a fibular head fracture may present with the same deficit pattern.[1][3]
Superficial peroneal nerve entrapment produces pain and paresthesias over the lower leg and dorsal aspect of the foot. Such a condition may result from an ankle sprain or twisting ankle injury, causing the superficial peroneal nerve to stretch in the lower leg or foot.[17] Acute or chronic compartment syndrome, which reduces tissue perfusion and oxygenation in the lateral leg compartment, can also lead to superficial peroneal nerve entrapment. Surgical decompression is required to relieve pain and other symptoms, especially in the acute setting.[17]
Common Peroneal Nerve Injury
Common peroneal nerve entrapment at the fibular head can cause neuropathic pain. Weight loss, leg crossing, and prolonged sleep are some causes of common peroneal nerve entrapment.[18] Leg ultrasound has proven to be useful in diagnosing this condition.[19]
Complete common peroneal nerve damage weakens the deep and superficial peroneal nerves, producing deficits in the areas of distribution of both nerve branches. Deep peroneal nerve deficits include muscle paralysis in the anterior leg and foot dorsum and numbness in the 1st interdigital space. Symptoms like lateral leg muscle paralysis and sensory loss over the lateral leg and dorsal foot surfaces are attributed to superficial peroneal nerve injury.
Foot Drop
Foot drop can result from peroneal injuries, varying in form based on the location of the damage.
An anterior foot drop, wherein the foot slaps on the ground whenever walking is attempted, arises from deep peroneal nerve paralysis and subsequent weakening of ankle dorsiflexion.
A lateral foot drop is more characteristic of superficial peroneal nerve damage, which weakens the muscles that evert the foot. Walking is accompanied by dragging of the foot's lateral margin.
Complete common peroneal nerve injuries or concurrent deep and superficial peroneal nerve damage produces both anterior and lateral foot drop.
Foot drop may manifest during pregnancy and parturition when the fetal head compresses the lumbosacral trunk (L4, L5) during the 3rd trimester.[20][21]
Other Issues
Double crush nerve injuries or syndromes involve peripheral nerve damage at two or more points so that neuropathy and radiculopathy are both present. Double crush syndromes of the leg are uncommon and can be challenging to diagnose.
For example, a man presenting with a foot drop from left foot dorsiflexion weakness is found to have left common peroneal nerve entrapment by leg electrodiagnostic and ultrasound studies. A left common peroneal nerve cyst is also evident on further workup. However, the foot drop persisted despite surgical cyst removal. Spinal MRI reveals stenosis of the vertebral foramen at L5-S1. Fusion of the vertebrae following multiple laminectomies led to improvement of the foot drop. This case demonstrates the utility of using electrodiagnostic studies in combination with ultrasound and MRI when diagnosing a complex neurological condition like double crush syndrome.[22][19]
Media
References
De Maeseneer M, Madani H, Lenchik L, Kalume Brigido M, Shahabpour M, Marcelis S, de Mey J, Scafoglieri A. Normal Anatomy and Compression Areas of Nerves of the Foot and Ankle: US and MR Imaging with Anatomic Correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 2015 Sep-Oct:35(5):1469-82. doi: 10.1148/rg.2015150028. Epub 2015 Aug 18 [PubMed PMID: 26284303]
Juneja P, Hubbard JB. Anatomy, Bony Pelvis and Lower Limb: Tibialis Anterior Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30020676]
Giuffre BA, Black AC, Jeanmonod R. Anatomy, Sciatic Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 29494038]
Garrett A, Geiger Z. Anatomy, Bony Pelvis and Lower Limb: Calf Deep Peroneal Nerve (Deep Fibular Nerve). StatPearls. 2023 Jan:(): [PubMed PMID: 30252289]
Khan IA, Mahabadi N, D’Abarno A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Lateral Compartment. StatPearls. 2023 Jan:(): [PubMed PMID: 30137811]
Thevenon A, Serafi R, Fontaine C, Grauwin MY, Buisset N, Tiffreau V. An unusual cause of foot clonus: spasticity of fibularis longus muscle. Annals of physical and rehabilitation medicine. 2013 Sep:56(6):482-8. doi: 10.1016/j.rehab.2013.04.002. Epub 2013 May 3 [PubMed PMID: 23688581]
Level 3 (low-level) evidenceWang CY, Chai YM, Wen G, Han P, Cheng L. Superficial peroneal neurocutaneous flap based on an anterior tibial artery perforator for forefoot reconstruction. Annals of plastic surgery. 2015 Jun:74(6):703-7. doi: 10.1097/SAP.0b013e3182a6ae22. Epub [PubMed PMID: 25969973]
Kim JS, Son DG, Choi TH, Kim NG, Lee KS, Han KH, Kim JH, Lee SI, Kang D. An anatomic study of the superficial peroneal nerve accessory artery and its perforators, and clinical application of superficial peroneal nerve accessory artery perforator flaps. Annals of plastic surgery. 2008 Jun:60(6):710-6. doi: 10.1097/SAP.0b013e3180cab77f. Epub [PubMed PMID: 18520212]
Level 3 (low-level) evidenceRecalde Rocha JF, Gilbert A, Masquelet A, Yousif NJ, Sanger JR, Matloub HS. The anterior tibial artery flap: anatomic study and clinical application. Plastic and reconstructive surgery. 1987 Mar:79(3):396-406 [PubMed PMID: 3823215]
Level 3 (low-level) evidenceTomaszewski KA, Graves MJ, Vikse J, Pękala PA, Sanna B, Henry BM, Tubbs RS, Walocha JA. Superficial fibular nerve variations of fascial piercing: A meta-analysis and clinical consideration. Clinical anatomy (New York, N.Y.). 2017 Jan:30(1):120-125. doi: 10.1002/ca.22741. Epub 2016 Jul 7 [PubMed PMID: 27271092]
Level 1 (high-level) evidencePrakash, Bhardwaj AK, Singh DK, Rajini T, Jayanthi V, Singh G. Anatomic variations of superficial peroneal nerve: clinical implications of a cadaver study. Italian journal of anatomy and embryology = Archivio italiano di anatomia ed embriologia. 2010:115(3):223-8 [PubMed PMID: 21287977]
Blair JM, Botte MJ. Surgical anatomy of the superficial peroneal nerve in the ankle and foot. Clinical orthopaedics and related research. 1994 Aug:(305):229-38 [PubMed PMID: 8050234]
de Leeuw PA, Golanó P, Blankevoort L, Sierevelt IN, van Dijk CN. Identification of the superficial peroneal nerve: Anatomical study with surgical implications. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2016 Apr:24(4):1381-5. doi: 10.1007/s00167-016-4063-8. Epub 2016 Mar 26 [PubMed PMID: 27017216]
de Leeuw PA, Golanó P, Sierevelt IN, van Dijk CN. The course of the superficial peroneal nerve in relation to the ankle position: anatomical study with ankle arthroscopic implications. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2010 May:18(5):612-7. doi: 10.1007/s00167-010-1099-z. Epub 2010 Mar 12 [PubMed PMID: 20224993]
Stephens MM, Kelly PM. Fourth toe flexion sign: a new clinical sign for identification of the superficial peroneal nerve. Foot & ankle international. 2000 Oct:21(10):860-3 [PubMed PMID: 11128019]
Ferkel RD, Small HN, Gittins JE. Complications in foot and ankle arthroscopy. Clinical orthopaedics and related research. 2001 Oct:(391):89-104 [PubMed PMID: 11603693]
Styf JR, Körner LM. Chronic anterior-compartment syndrome of the leg. Results of treatment by fasciotomy. The Journal of bone and joint surgery. American volume. 1986 Dec:68(9):1338-47 [PubMed PMID: 3782205]
Öztürk İ, Fidanci H, Arlier Z. Neuropathic pain in peroneal nerve entrapment at the fibular head. Arquivos de neuro-psiquiatria. 2022 Nov:80(11):1134-1140. doi: 10.1055/s-0042-1758644. Epub 2022 Dec 28 [PubMed PMID: 36577412]
Kim JY, Song S, Park HJ, Rhee WI, Won SJ. Diagnostic Cutoff Value for Ultrasonography of the Common Fibular Neuropathy at the Fibular Head. Annals of rehabilitation medicine. 2016 Dec:40(6):1057-1063. doi: 10.5535/arm.2016.40.6.1057. Epub 2016 Dec 30 [PubMed PMID: 28119836]
Nguyen DT, Zaferanieh MH, Black AC Jr, Hamedi KR, Goodwin RL, Nathaniel TI. Obstetric Neuropathy in Diabetic Patients: The "Double Hit Hypothesis". International journal of molecular sciences. 2023 Apr 6:24(7):. doi: 10.3390/ijms24076812. Epub 2023 Apr 6 [PubMed PMID: 37047786]
Black AC, Williams SE, Holt JA, Jackson M, Hawks K, Munakomi S. Foot Drop in Obstetrics. StatPearls. 2023 Jan:(): [PubMed PMID: 35881745]
Shields LBE, Iyer VG, Harpring JE, Rao AJ, Zhang YP, Shields CB. Role of electromyography and ultrasonography in the diagnosis of double crush lumbar radiculopathy and common fibular injury: illustrative cases. Journal of neurosurgery. Case lessons. 2022 Apr 18:3(16):. pii: CASE21566. doi: 10.3171/CASE21566. Epub 2022 Apr 18 [PubMed PMID: 36303488]
Level 3 (low-level) evidence