Definition/Introduction
The National Quality Forum (NQF) is an independent, nonpartisan organization tasked with devising a national strategy to set standards for quality improvement and reporting in the United States healthcare industry. It is the first-ever public service organization explicitly focused on addressing the quality of healthcare. The NQF consists of more than 400 member bodies, including consumer organizations, private and public purchasers, hospitals, physicians, certifying and accreditation agencies, and other healthcare stakeholders.
The modern movement of “healthcare quality and improvement” as a distinct field of study in the United States began in 1966, with the development of conceptualizing healthcare in terms of structure, processes, and outcomes. In 1987, the Healthcare Financing Administration released the first-ever publically available hospital-specific mortality data. In the early 1990s, the National Committee on Quality Assurance used the Healthcare Effectiveness Data and Information Set as a performance improvement tool to standardize evaluating and reporting quality improvement initiatives within individual health plans nationwide. However, perhaps the most influential event that ultimately led to the development of the NQF was a landmark 1999 Institute of Medicine (IOM) report, “To Err Is Human,” which persuasively tied healthcare quality to patient safety.[1][2][3]
There remained a growing focus on patient safety and healthcare quality over the ensuing years, including the founding of the NQF by syndication of private and non-profit organizations.
Evolution of NQF
Before the NQF, there was very little systematic information available on healthcare quality. Similarly, no framework existed for the measurement or reporting of quality metrics. As a result, developing an appropriate healthcare policy was difficult. One of the NQF’s first tasks was to establish a Strategic Framework Board which consisted of nine healthcare quality experts to 1) design a national strategy for quality measurement and reporting system; 2) set forth fair and transparent benchmarking; and 3) identify potential barriers and recommend possible solutions to successful implementation. With consistent and ongoing intensive review and involvement of multiple stakeholders, NQF-endorsed measures began to be considered the gold standard for healthcare quality measurement.[1]
Role of The NQF on Quality Improvement and Cost-effectiveness
The NQF’s focus on national quality measurement and reporting transformed the United States into a worldwide leader in addressing complex issues such as risk adjustment for severity of illness. Stakeholders, including physicians, patients, and healthcare organizations, have utilized NQF systems as initiatives to reduce healthcare costs by improving quality. The NQF’s approach fits in two discrete but complementary roles:
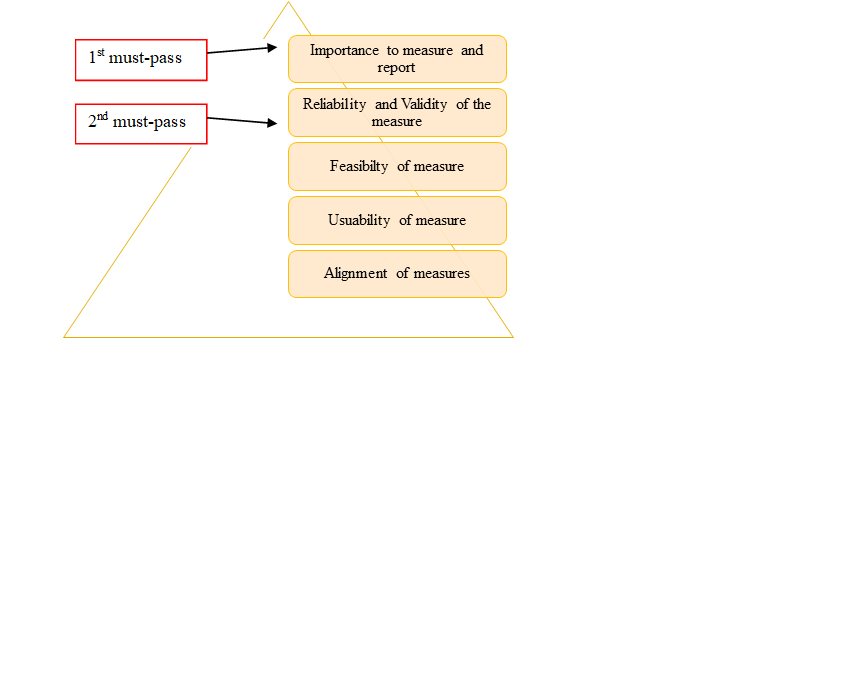
- Endorsing standardized performance measures: This approach involves pooling and prioritizing recommendations from various stakeholders such as the American Medical Association, the National Committee for Quality Assurance, Center for Medicare & Medicaid Services, and Joint Commission. The NQF uses distinct criteria to evaluate submitted metrics. Each proposed metric must meet the first and second criteria in the pyramid to be endorsed (Fig.1). In other words, an endorsed measure must demonstrate a high-impact health target or priority and must meet scientific standards. Also, measures should be relatively easy to use and tailor to specific healthcare settings with little burden. Hence, NQF endorsed measures are considered as a gold standard and granted privileged status in federal regulations.[1][4]
- Convene leaders in the public and private sectors to build consensus and guidelines regarding:
- Formulating priorities for National Quality Strategy on behalf of the US Department of Health and Human Services, with particular focus on access and affordability
- Quality measures selection to be used in federal public reporting and value-based programs
- Curtailing total healthcare costs by utilizing endorsed measures within varied programs
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
1. Alignment among diverse stakeholders
Although NQF-endorsed measures are widely available, every stakeholder operates independently and with limited collaboration with others. This arrangement results in the duplication of data collection and analysis, ultimately leading to increased burden and cost for providers. For instance, many specialty-specific registries have robust data registries but have limited data-sharing processes with each other. Establishing transparency of specific types of measures amongst clinical registries can align stakeholders and enhance quality reporting and outcomes.[1]
2. Ongoing review of the effects of implemented NQF- endorsed measures
Currently, there is no central, publically available catalog of all fully implemented NQF-endorsed measures across stakeholders. Published reviews and outcomes after NQF-program implementation could help end-users (e.g., providers) to understand the broader implication of these efforts.
Clinical Significance
NQF-endorsed measures are used by various stakeholders and have proven to be highly impactful in improving healthcare quality. One example involves central line-associated bloodstream infections. After implementing NQF-endorsed measures, there was a 58% reduction in these infections between 2001 and 2009 nationwide, which by some estimates resulted in 6000 deaths prevented and $1.8 billion in costs saved. Also, in 650 hospitals that fully implemented NQF endorsed safety practices, there has been a decline in mortality. The Centers for Medicare & Medicaid Services reported that 27 hospitals saw an average 16% decrease in neonatal intensive care unit (NICU) admissions and resultant savings of hundreds of millions of dollars after implementation of NQF-endorsed quality reporting measures.[7][8][9]
NQF Funding:
Currently, the NQF receives funding from a combination of private and public efforts: one-third of its budget is from the private sector and the remainder from the public. The NQF also receives funding from philanthropic organizations such as Robert Wood Johnson Foundation and the Commonwealth Fund. The federal government provides funding under the Medicare Improvements for Patients and Providers Act (2008) and The American Taxpayer Relief Act (2013) (NQF, 2018).[1]
Nursing, Allied Health, and Interprofessional Team Interventions
NQF has endorsed 15 nursing-specific measures recognizing the impact of nurses in healthcare delivery and outcomes. These measures quantify the delivery of safe, timely, efficient, and equitable care provided by nursing units in hospitals. By implementing NQF endorsed nursing-specific measures, hospitals can generate performance reports, which, in turn, help institutions with quality improvement efforts, RN recruitment and retention, patient engagement, staff education, and nursing administration.[10]
Media
(Click Image to Enlarge)
References
Burstin H, Leatherman S, Goldmann D. The evolution of healthcare quality measurement in the United States. Journal of internal medicine. 2016 Feb:279(2):154-9. doi: 10.1111/joim.12471. Epub [PubMed PMID: 26785953]
Level 2 (mid-level) evidenceAdirim T, Meade K, Mistry K, COUNCIL ON QUALITY IMPROVEMENT AND PATIENT SAFETY, COMMITTEE ON PRACTICE AND AMBULATORY MANAGEMENT. A New Era in Quality Measurement: The Development and Application of Quality Measures. Pediatrics. 2017 Jan:139(1):. pii: e20163442. doi: 10.1542/peds.2016-3442. Epub [PubMed PMID: 28025242]
Level 2 (mid-level) evidenceKizer KW. The National Quality Forum seeks to improve health care. Academic medicine : journal of the Association of American Medical Colleges. 2000 Apr:75(4):320-1 [PubMed PMID: 10893112]
Level 2 (mid-level) evidenceHyder JA,Niconchuk J,Glance LG,Neuman MD,Cima RR,Dutton RP,Nguyen LL,Fleisher LA,Bader AM, What can the national quality forum tell us about performance measurement in anesthesiology? Anesthesia and analgesia. 2015 Feb; [PubMed PMID: 25602454]
Level 2 (mid-level) evidencede Vries EF, Struijs JN, Heijink R, Hendrikx RJ, Baan CA. Are low-value care measures up to the task? A systematic review of the literature. BMC health services research. 2016 Aug 18:16(1):405. doi: 10.1186/s12913-016-1656-3. Epub 2016 Aug 18 [PubMed PMID: 27539054]
Level 1 (high-level) evidenceDamberg CL, Sorbero ME, Lovejoy SL, Lauderdale K, Wertheimer S, Smith A, Waxman D, Schnyer C. An Evaluation of the Use of Performance Measures in Health Care. Rand health quarterly. 2012 Winter:1(4):3 [PubMed PMID: 28083210]
Centers for Disease Control and Prevention (CDC). Vital signs: central line-associated blood stream infections--United States, 2001, 2008, and 2009. MMWR. Morbidity and mortality weekly report. 2011 Mar 4:60(8):243-8 [PubMed PMID: 21368740]
Clark SL, Frye DR, Meyers JA, Belfort MA, Dildy GA, Kofford S, Englebright J, Perlin JA. Reduction in elective delivery at {39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admission and stillbirth. American journal of obstetrics and gynecology. 2010 Nov:203(5):449.e1-6. doi: 10.1016/j.ajog.2010.05.036. Epub 2010 Jul 8 [PubMed PMID: 20619388]
Level 2 (mid-level) evidenceBrega AG, Hamer MK, Albright K, Brach C, Saliba D, Abbey D, Gritz RM. Organizational Health Literacy: Quality Improvement Measures with Expert Consensus. Health literacy research and practice. 2019 Apr:3(2):e127-e146. doi: 10.3928/24748307-20190503-01. Epub 2019 Jul 1 [PubMed PMID: 31294314]
Level 2 (mid-level) evidenceKurtzman ET, Corrigan JM. Measuring the contribution of nursing to quality, patient safety, and health care outcomes. Policy, politics & nursing practice. 2007 Feb:8(1):20-36 [PubMed PMID: 17470769]
Level 2 (mid-level) evidence