 Anatomy, Shoulder and Upper Limb, Humerus
Anatomy, Shoulder and Upper Limb, Humerus
Introduction
The humerus is the largest bone of the upper extremity and defines the human brachium (arm). It articulates proximally with the glenoid via the glenohumeral (GH) joint and distally with the radius and ulna at the elbow joint. The most proximal portion of the humerus is the head of the humerus, which forms a ball and socket joint with the glenoid cavity on the scapula.[1] Just inferior to the head of the humerus is the anatomical neck of the humerus, which divides the head of the humerus from the greater and lesser tubercles. The anatomical neck of the humerus is the residual epiphyseal plate. An intertubercular groove appears proximally, which demarcates the two tubercles vertically. Following the tubercles is the surgical neck of the humerus, a site commonly susceptible to fractures.
Continuing distally is the cylindrical-shaped shaft of the humerus, which contains a deltoid tubercle on its lateral aspect and a radial groove on its posterior aspect (also referred to as the spiral groove).[2] At the distal portion of the humerus, there exists a widening of the bone that forms the medial and lateral epicondyles. The distal portion of the humerus ends with an area referred to as the condyle, which is composed of the trochlea, capitulum, olecranon, coronoid and radial fossae.[3] On the anterior lateral surface of the condyle is the lateral capitulum, which articulates with the head of the radius bone, and on the anterior medial surface of the condyle is the trochlea, which articulates the trochlear notch of the ulna bone. The coronoid fossa is located superior to the trochlea and accommodates the coronoid process of the ulna and superior to the capitulum on the anterior surface of the condyle, which is the radial fossa which receives with the head of the radius, both upon flexion of the elbow joint. On the posterior surface of the condyle is the olecranon fossa, which articulates with the olecranon of the ulnar bone upon flexion of the elbow joint.[4]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The humeral head articulates with the glenoid fossa of the scapula and forms the glenohumeral joint, a synovial ball and socket joint.[5] This joint allows movement along multiple planes, including internal and external rotation, abduction and adduction, flexion and extension, and is principally determined by activation of the rotator cuff muscles (teres minor, subscapularis, supraspinatus, infraspinatus) pectoralis major and deltoid. The glenohumeral joint contains multiple synovial bursae that allow frictionless mobility, including the subacromial, subdeltoid, subcoracoid, and coracobrachial bursae.[6] The coracoacromial and acromioclavicular ligaments stabilize the GH joint; these prevent proximal migration of the humerus.[7]
Articulation of the capitellum and trochlea of the humerus with the head of the radius bone and trochlear notch of the ulna forms the elbow joint, a synovial hinge joint. This joint is stabilized by the ulnar (medial) collateral ligament and radial (lateral) collateral ligament complexes.[8] The ulnar collateral ligament (UCL) has three components:
- Anterior oblique band: the strongest and most significant stabilizer to valgus stress forces
- Courses from the medial epicondyle of the humerus to the sublime tubercle at the proximal ulna
- Posterior oblique band: tightest in flexion; the posterior component of the UCL demonstrates the most significant change in tension from flexion to extension range of motion (ROM) at the elbow.
- Transverse ligament: contributes minimal, if any, to elbow joint stability.
An olecranon bursa exists here to reduce friction during movement as well. This joint allows only extension and flexion. Elbow movement is principally the result of the biceps brachii, coracobrachialis, and triceps muscles.[9] One should note that in anatomical position, the humerus and antebrachial bones do not perfectly align, and instead form what is known as a carrying angle. In males, this angle varies from 5 to 10 degrees, and in females may reach up to 18 degrees.[10] This angle allows clearing of the hips, and an excessive lateral deviation is referred to as cubitus valgus, with excessive medial deviation referred to as cubitus varus.
Embryology
As one of the many long bones within the appendicular skeleton, the humerus develops via endochondral ossification.[11] This process is characterized by the replacement of a cartilage template by bone. Initially, a relatively tiny cartilage model is laid down by mesenchymal cells that form cartilage secreting chondrocytes. Second, in the center of the cartilage template (ossification center), there is chondrocyte hypertrophy and secretion factors such as alkaline phosphatase to promote calcification of that cartilage. This action forms a blockade of nutrients and causes chondrocyte death. However, before dying, these cells also secrete vascular endothelial growth factor (VEGF) to support angiogenesis towards the interior of this calcifying cartilage. Meanwhile, under the influence of Indian hedgehog homolog (IHH) protein, cells outside in the perichondrium differentiate into osteoblasts and form a layer of bone surrounding the center of cartilage known as the bony collar.[11]
As time progresses, a central area of dead chondrocytes develops, with little pieces of calcified cartilage left behind, a shell of bone around the center, and the vascular supply going around the interior. Vascular supply brings into the interior mesenchymal cells that differentiate into more osteoblasts and monocytes that form osteoclasts. In the center of the initial cartilage template, bone is resorbed on the inside and deposited on the outside, creating the growth in width of a hollow entity (forming a marrow). Simultaneously, the proximal and distal ends of the cartilage template have chondrocytes that continue to proliferate as secondary ossification centers. This activity allows cartilage growth at the end of the bones, providing vertically expansive capabilities. Ultimately, the areas where bone meets cartilage forms the epiphyseal plate (a linear zone of cartilage), where bone replaces cartilage continuously until bone growth completely fuses and stops around puberty. In the humerus specifically, there are eight ossification centers, at the head of the humerus, humeral shaft, greater and lesser tubercles, medial and lateral epicondyles, trochlea, and olecranon.
The ossification of the shaft occurs at eight weeks gestation, with the humeral head ossification occurring at birth/after birth. The greater tubercle's ossification takes place during the first year of life and the lesser tubercle ossification within the first six years of life.[12][13] By the time of adolescence, all proximal ossification centers of the humerus have fully fused with the shaft. The distal ossifications at the condyle and trochlea and olecranon take place between early and later adolescence and fuse with the shaft of the humerus by late adolescence.[14]
Blood Supply and Lymphatics
The primary blood supply of the proximal humerus comes from anastomoses between the anterior and posterior circumflex humeral arteries.[15] These are branches of the distal third of the axillary artery. Recent studies suggest the posterior humeral circumflex artery to be the primary source of blood supply to the humeral head.[16] The terminal division of the anterior humeral circumflex artery is the arcuate artery, which supplies the majority of the greater tuberosity.
The axillary artery continues to become the brachial artery, which, along with one of its branches, the profunda brachii artery, will give off peri-osteal arteries to provide the blood supply for the rest humerus and its attached muscles.[17] The inner portions of the humerus are vascularized by nutrient arteries that also branch off from the brachial artery in the vicinity of the middle of the humerus.[18]
Nerves
The axillary nerve, formed from the posterior cord of the brachial plexus, wraps around the surgical neck of the humerus, and provides innervation to the deltoid and rotator cuff muscles, specifically the teres minor.[19] Innervation of the anterior portion of the brachium is supplied by the musculocutaneous nerve, which forms as a division of the lateral cord of the brachial plexus. This nerve pierces through the coracobrachialis muscle and travels between the biceps brachii and coracobrachialis, ultimately finding its termination as the lateral cutaneous nerve of the forearm. The radial nerve from the posterior cord of the brachial plexus courses through the spiral groove of the humerus, posterior to the brachial artery, and anterior to the long head of the triceps.[20] It innervates the posterior muscles of the arm, forearm, and overlying skin. The radial nerve is also responsible for the innervation of the lateral and medial epicondyle of the humerus.[21] One should note that the median nerve and ulnar nerve likewise come off the brachial plexus and travel down along the brachium, however, do not supply innervation to this region.
Muscles
The humerus serves as the origin and insertion site of many upper limb muscles that divide into the following distinctions: scapulohumeral muscles, anterior compartment muscles, posterior compartment muscles.
Scapulohumeral muscles: The deltoid muscle, which defines the shoulder contour of the upper limb, originates at three locations: the acromion of the scapula, the spine of the scapula and clavicle, with each part inserting into the deltoid tuberosity of the humerus. The deltoid muscle allows internal/external rotation and abduction/adduction of the humerus.[22] The pectoralis major muscle originates at the clavicle, manubrium, sternum body, and true ribs and inserts into the intertubercular sulcus of the humerus. It allows adduction, flexion, extension, and medial rotation of the humerus.[23] Four muscles form the rotator cuff; the subscapularis, supraspinatus, infraspinatus, and teres minor. The subscapularis muscle originates from the subscapular fossa of the scapula and inserts onto the lesser tubercle of the humerus, facilitating internal rotation of the humerus. The supraspinatus muscle originates in the supraspinous fossa of the scapula and inserts into the greater tubercle of the humerus, facilitating the abduction of the humerus. The infraspinatus muscle originates in the infraspinous fossa and scapula spine and inserts into the greater tubercle of the humerus as well and allows external rotation of the humerus. The teres major originates the inferior angle of the scapula and inserts into the lesser tuberosity of the humerus, allowing internal rotation and adduction. The teres minor originates on the lateral border of the scapula and inserts into the greater tubercle and allows external rotation.[24][25][26][27]
Anterior compartment muscles: The biceps brachii muscle has a long head and short head but does not have an actual origin or insertion sites on the humerus.[28] However, there is a transverse humeral ligament which projects from the lesser tubercle to the greater tubercle of the humerus and converts the humeral intertubercular groove into a canal which the tendon of the biceps brachii long head travels through on its way from its origination on the supraglenoid tubercle of the scapula to the radius. The coracobrachialis originates on the coracoid process of the scapula and inserts onto the humerus and its medial surface, allowing flexion and internal rotation.[29] The brachialis muscle originates on the anterior surface of the distal humerus and inserts onto the ulna for flexion of the forearm.[30]
Posterior compartment muscles: The triceps brachii muscle contains three heads, with the medial head originating on the posterior aspect of the humerus, inferior to the spiral groove, and the lateral head originating on the posterior surface, both insert into the olecranon process of the ulna and allow extension of the forearm at the elbow joint.[31] Of note, the humerus along with the long head of the triceps, teres major and teres minor, form a quadrangular space through which the posterior circumflex artery and vein and radian nerve travel.[32]
Surgical Considerations
Elderly patients who fall on their shoulders or land on their outstretched arm can sustain proximal humeral fractures.[33] This injury presents with shoulder pain and immobility of the extremity. Multiple fragmentations of these proximal fractures can also lead to post-traumatic osteonecrosis, which can cause long-term morbidity.[34] The majority of proximal humerus fractures receive non-operative treatment. However, elderly patients with severe displacement can benefit from operative intervention, as these patients have limited bone remodeling and growth. Internal fixation via smooth wires, threaded wires, cannulated screws and intramedullary nailing are interventional choices.[35]. A reverse shoulder arthroplasty is also an option for proximal humerus fracture in the elderly, glenohumeral dislocations, rotator cuff tears, or joint disease.[36] Shoulder arthroplasty can also be indicated for shoulder osteoarthritis, inflammatory arthritis.[37] Anterior dislocation of the glenohumeral joint is common among young and active patients.[38] The greater tuberosity of the humerus is susceptible to displacement fractures, which can affect the rotator cuff muscles and also cause subacromial impingement. Surgical intervention is usually required with displacements greater than 3 mm.[39]
Children ages three and younger can sustain transphyseal fractures of the distal humerus after a fall or trauma.[40] On radiologic imaging, the humerus and forearm bone will not align according to the standard carrying angle and will have a noticeable cubitus varus. Surgical intervention should take place with closed reduction and percutaneous pinning techniques. Common sequelae include osteonecrosis of the condyles and growth arrest. Surgical intervention usually includes lateral closing wedge osteotomy, dome osteotomy, or multi-planar osteotomy.[41]
Intercondylar fractures at the distal humerus are often treated surgically as well with olecranon osteotomy.[42] Post-traumatic supracondylar humeral fractures can lead to avascular necrosis as there is an interruption of the trochlear blood supply. Patients may present asymptomatically at the time of the injury but can develop pain or loss of motion due to necrosis within six months.[43]
Clinical Significance
Radial Nerve Injury
Radial nerve palsy is among the most common peripheral nerve injuries following a humeral fracture.[44] Typically, treatment includes observation, unless nerve recovery (as demonstrated on EMG/NCS studies) does not occur within 3 to 6 months. Advocates for early exploration of the radial nerve cite delayed repair and significant internal loss of patient function as deterrents for late exploration. Trauma or fracture at the radial groove (mid-shaft) may cause radial nerve injury.
Conditions of the Shoulder
Conditions such as calcific tendinitis of the rotator cuff and adhesive capsulitis of the shoulder (i.e., frozen shoulder syndrome) are relatively common conditions with controversial and/or multifactorial etiologies.[45] Treatment consists of rest and exercise, with little need for operative intervention. However, surgical management of frozen shoulder syndrome can occur via infiltration brisement under general anesthesia.
Metastatic Disease
Metastatic bone disease causes destructive bone lesions and significant localized pain, most often in the humerus. Lesions can increase the risk of a fracture within the humerus.[46] In patients with lesions less than 50% of the cortex, treatment is done via external beam irradiation. However, with destructive lesions involving more than half the cortex, treatment consists of intramedullary nailing with postoperative external beam irradiation. Bone resection/reconstruction may be indicated in the instance where the disease persists.
Supracondylar Fractures of the Distal Humerus
This fracture is the most common elbow fracture in the pediatric population. The fracture location is superior to the medial and lateral condyles and epicondyles. Supracondylar fractures of the distal humerus by the elbow joint can compromise nerve and vasculature depending on its displacement. Anterior displacement puts the median nerve and brachial artery at risk. Posterior displacement puts the radial artery at risk. Palpation of distal pulses and capillary refill should be part of the initial workup to survey for preserved blood supply. Anteroposterior and lateral radiographs are necessary for accurate diagnosis and treatment. Nondisplaced fractures are treated initially with a posterior splint and eventual casting. Displaced fractures are reduced, and pinned percutaneously. Malunion, compartment syndrome, and neurovascular complications are morbidities related to this fracture.[47]
Other/Miscellaneous Conditions
Hematologic, infectious, genetic, and neurologic disorders may cause humerus varus.[48] In this condition, the medial portion of the proximal humerus will fail to develop correctly, and the lateral portion will develop more rapidly. This condition creates a varus rotation of the humerus causing decreased arm abduction and limited flexion at the shoulder joint. However, functional impairment is not common. Surgical intervention involves a valgus osteotomy of the humerus using a plate screw fixation.
Disappearing bone disease is a rare musculoskeletal condition marked by bone resorption, lack of bone formation, and lack of vascular proliferation. This disorder has severe quality of life implications.[49] Similarly, Gorham-Stout disease in the humerus is characterized by resorption of the osseous matrix with a lack of bone formation.[50] The etiology of the disease is unknown; however, lymphovascular malformation in the bone is present. Common symptoms include aching pain, progressive weakness, and subsequent fractures. Treatment is challenging and involves a combination of surgical intervention, medication, and radiotherapy.
Charcot arthropathy is a rare disorder characterized by debilitating joint destruction. The disease can lead to bone and soft tissue loss around the humerus and can alter muscular control. Treatment involves shoulder arthroplasty.[51]
Osteochondrosis of the humerus is associated with Panner disease and osteochondritis dissecans. The two diseases present similarly.[52] Panner disease involves avascular necrosis of the capitulum, and onset is typically between ages 7 and 10, younger than the onset of osteochondritis dissecans. Panner disease generally is not treated with operative intervention.[53]
Media
(Click Image to Enlarge)
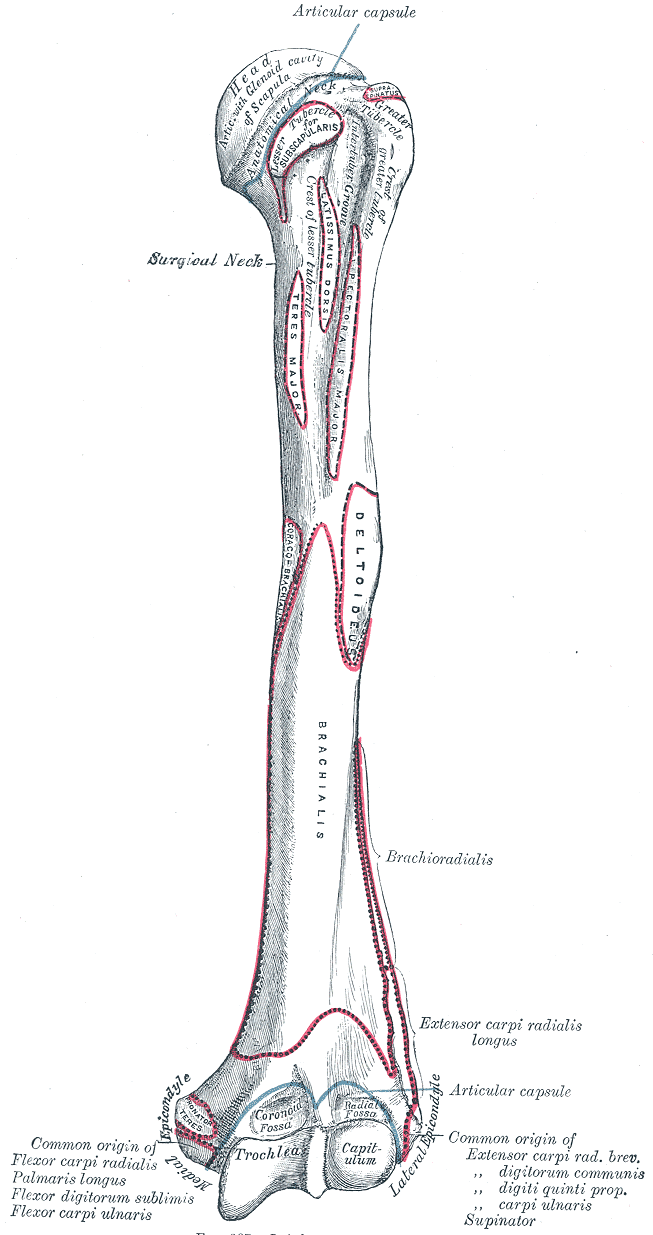
Upper Arm Anatomy. This illustration details the humerus and various attachment sites on its surface. Shown are the head, surgical and anatomical necks, greater and lesser tubercles, crest of lesser tubercle, intertubercular groove, trochlea capitulum, radial and coronoid fossae, lateral and medial epicondyles, and attachment sites for the subscapularis, coracobrachialis, teres major, latissimus dorsi, pectoralis major, deltoid, brachialis, forearm extensors and flexors, brachioradialis, and extensor carpi radialis longus.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Capo JT, Criner KT, Shamian B. Exposures of the humerus for fracture fixation. Hand clinics. 2014 Nov:30(4):401-14, v. doi: 10.1016/j.hcl.2014.07.001. Epub 2014 Oct 23 [PubMed PMID: 25440069]
Paryavi E, Pensy RA, Higgins TF, Chia B, Eglseder WA. Salvage of upper extremities with humeral fracture and associated brachial artery injury. Injury. 2014 Dec:45(12):1870-5 [PubMed PMID: 25249243]
Level 2 (mid-level) evidenceSamart S, Apivatgaroon A, Lakchayapakorn K, Chemchujit B. The correlation between acromion-axillary nerve distance and upper arm length; a cadaveric study. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2014 Aug:97 Suppl 8():S27-33 [PubMed PMID: 25518290]
Hamilton MA, Diep P, Roche C, Flurin PH, Wright TW, Zuckerman JD, Routman H. Effect of reverse shoulder design philosophy on muscle moment arms. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2015 Apr:33(4):605-13. doi: 10.1002/jor.22803. Epub 2015 Feb 12 [PubMed PMID: 25640775]
Prescher A. Anatomical basics, variations, and degenerative changes of the shoulder joint and shoulder girdle. European journal of radiology. 2000 Aug:35(2):88-102 [PubMed PMID: 10963915]
Wilk KE, Arrigo CA, Andrews JR. Current concepts: the stabilizing structures of the glenohumeral joint. The Journal of orthopaedic and sports physical therapy. 1997 Jun:25(6):364-79 [PubMed PMID: 9168344]
Kanatli U, Bölükbaşi S, Ekin A, Ozkan M, Simşek A. [Anatomy, biomechanics, and pathophysiology of instability of the glenohumeral joint]. Acta orthopaedica et traumatologica turcica. 2005:39 Suppl 1():4-13 [PubMed PMID: 15925914]
Karbach LE, Elfar J. Elbow Instability: Anatomy, Biomechanics, Diagnostic Maneuvers, and Testing. The Journal of hand surgery. 2017 Feb:42(2):118-126. doi: 10.1016/j.jhsa.2016.11.025. Epub [PubMed PMID: 28160902]
Martin S, Sanchez E. Anatomy and biomechanics of the elbow joint. Seminars in musculoskeletal radiology. 2013 Nov:17(5):429-36. doi: 10.1055/s-0033-1361587. Epub 2013 Dec 10 [PubMed PMID: 24327407]
Paraskevas G, Papadopoulos A, Papaziogas B, Spanidou S, Argiriadou H, Gigis J. Study of the carrying angle of the human elbow joint in full extension: a morphometric analysis. Surgical and radiologic anatomy : SRA. 2004 Feb:26(1):19-23 [PubMed PMID: 14648036]
Level 2 (mid-level) evidenceLong F, Ornitz DM. Development of the endochondral skeleton. Cold Spring Harbor perspectives in biology. 2013 Jan 1:5(1):a008334. doi: 10.1101/cshperspect.a008334. Epub 2013 Jan 1 [PubMed PMID: 23284041]
Level 3 (low-level) evidenceKwong S, Kothary S, Poncinelli LL. Skeletal development of the proximal humerus in the pediatric population: MRI features. AJR. American journal of roentgenology. 2014 Feb:202(2):418-25. doi: 10.2214/AJR.13.10711. Epub [PubMed PMID: 24450686]
Level 2 (mid-level) evidenceZember JS, Rosenberg ZS, Kwong S, Kothary SP, Bedoya MA. Normal Skeletal Maturation and Imaging Pitfalls in the Pediatric Shoulder. Radiographics : a review publication of the Radiological Society of North America, Inc. 2015 Jul-Aug:35(4):1108-22. doi: 10.1148/rg.2015140254. Epub [PubMed PMID: 26172355]
Jaimes C, Jimenez M, Marin D, Ho-Fung V, Jaramillo D. The trochlear pre-ossification center: a normal developmental stage and potential pitfall on MR images. Pediatric radiology. 2012 Nov:42(11):1364-71. doi: 10.1007/s00247-012-2454-7. Epub 2012 Jul 19 [PubMed PMID: 22810145]
Menck J, Döbler A, Döhler JR. [Vascularization of the humerus]. Langenbecks Archiv fur Chirurgie. 1997:382(3):123-7 [PubMed PMID: 9324609]
Hettrich CM, Boraiah S, Dyke JP, Neviaser A, Helfet DL, Lorich DG. Quantitative assessment of the vascularity of the proximal part of the humerus. The Journal of bone and joint surgery. American volume. 2010 Apr:92(4):943-8. doi: 10.2106/JBJS.H.01144. Epub [PubMed PMID: 20360519]
Attum B, Thompson JH. Humerus Fractures Overview. StatPearls. 2024 Jan:(): [PubMed PMID: 29489190]
Level 3 (low-level) evidenceIchimura K, Kinose S, Kawasaki Y, Okamura T, Kato K, Sakai T. Anatomic characterization of the humeral nutrient artery: Application to fracture and surgery of the humerus. Clinical anatomy (New York, N.Y.). 2017 Oct:30(7):978-987. doi: 10.1002/ca.22976. Epub 2017 Aug 21 [PubMed PMID: 28795436]
Marion B, Leclère FM, Casoli V, Paganini F, Unglaub F, Spies C, Valenti P. Potential axillary nerve stretching during RSA implantation: an anatomical study. Anatomical science international. 2014 Sep:89(4):232-7. doi: 10.1007/s12565-014-0229-y. Epub 2014 Feb 5 [PubMed PMID: 24497198]
Ozer H, Açar HI, Cömert A, Tekdemir I, Elhan A, Turanli S. Course of the innervation supply of medial head of triceps muscle and anconeus muscle at the posterior aspect of humerus (anatomical study). Archives of orthopaedic and trauma surgery. 2006 Oct:126(8):549-53 [PubMed PMID: 16826408]
Dellon AL, Ducic I, Dejesus RA. The innervation of the medial humeral epicondyle: implications for medial epicondylar pain. Journal of hand surgery (Edinburgh, Scotland). 2006 Jun:31(3):331-3 [PubMed PMID: 16580101]
Sakoma Y, Sano H, Shinozaki N, Itoigawa Y, Yamamoto N, Ozaki T, Itoi E. Anatomical and functional segments of the deltoid muscle. Journal of anatomy. 2011 Feb:218(2):185-90. doi: 10.1111/j.1469-7580.2010.01325.x. Epub 2010 Nov 30 [PubMed PMID: 21118198]
Sanchez ER, Howland N, Kaltwasser K, Moliver CL. Anatomy of the sternal origin of the pectoralis major: implications for subpectoral augmentation. Aesthetic surgery journal. 2014 Nov:34(8):1179-84. doi: 10.1177/1090820X14546370. Epub 2014 Aug 13 [PubMed PMID: 25121786]
Curtis AS, Burbank KM, Tierney JJ, Scheller AD, Curran AR. The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2006 Jun:22(6):609.e1 [PubMed PMID: 16762697]
Salhi A, Burdin V, Mutsvangwa T, Sivarasu S, Brochard S, Borotikar B. Subject-specific shoulder muscle attachment region prediction using statistical shape models: A validity study. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual International Conference. 2017 Jul:2017():1640-1643. doi: 10.1109/EMBC.2017.8037154. Epub [PubMed PMID: 29060198]
Vosloo M, Keough N, De Beer MA. The clinical anatomy of the insertion of the rotator cuff tendons. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2017 Apr:27(3):359-366. doi: 10.1007/s00590-017-1922-z. Epub 2017 Feb 16 [PubMed PMID: 28204962]
Dancker M, Lambert S, Brenner E. Teres major muscle - insertion footprint. Journal of anatomy. 2017 May:230(5):631-638. doi: 10.1111/joa.12593. Epub 2017 Feb 9 [PubMed PMID: 28185265]
Quach T, Jazayeri R, Sherman OH, Rosen JE. Distal biceps tendon injuries--current treatment options. Bulletin of the NYU hospital for joint diseases. 2010:68(2):103-11 [PubMed PMID: 20632985]
Ilayperuma I, Nanayakkara BG, Hasan R, Uluwitiya SM, Palahepitiya KN. Coracobrachialis muscle: morphology, morphometry and gender differences. Surgical and radiologic anatomy : SRA. 2016 Apr:38(3):335-40. doi: 10.1007/s00276-015-1564-y. Epub 2015 Oct 13 [PubMed PMID: 26464302]
Tagliafico A, Michaud J, Perez MM, Martinoli C. Ultrasound of distal brachialis tendon attachment: normal and abnormal findings. The British journal of radiology. 2013 May:86(1025):20130004. doi: 10.1259/bjr.20130004. Epub 2013 Feb 18 [PubMed PMID: 23420050]
Handling MA, Curtis AS, Miller SL. The origin of the long head of the triceps: a cadaveric study. Journal of shoulder and elbow surgery. 2010 Jan:19(1):69-72. doi: 10.1016/j.jse.2009.06.008. Epub [PubMed PMID: 19748801]
Brown SA, Doolittle DA, Bohanon CJ, Jayaraj A, Naidu SG, Huettl EA, Renfree KJ, Oderich GS, Bjarnason H, Gloviczki P, Wysokinski WE, McPhail IR. Quadrilateral space syndrome: the Mayo Clinic experience with a new classification system and case series. Mayo Clinic proceedings. 2015 Mar:90(3):382-94. doi: 10.1016/j.mayocp.2014.12.012. Epub 2015 Jan 31 [PubMed PMID: 25649966]
Level 2 (mid-level) evidenceLaunonen AP, Sumrein BO, Lepola V. Treatment of proximal humerus fractures in the elderly. Duodecim; laaketieteellinen aikakauskirja. 2017:133(4):353-8 [PubMed PMID: 29205983]
Patel S, Colaco HB, Elvey ME, Lee MH. Post-traumatic osteonecrosis of the proximal humerus. Injury. 2015 Oct:46(10):1878-84. doi: 10.1016/j.injury.2015.06.026. Epub 2015 Jun 19 [PubMed PMID: 26113032]
King EC, Ihnow SB. Which Proximal Humerus Fractures Should Be Pinned? Treatment in Skeletally Immature Patients. Journal of pediatric orthopedics. 2016 Jun:36 Suppl 1():S44-8. doi: 10.1097/BPO.0000000000000768. Epub [PubMed PMID: 27100038]
Acevedo DC, Vanbeek C, Lazarus MD, Williams GR, Abboud JA. Reverse shoulder arthroplasty for proximal humeral fractures: update on indications, technique, and results. Journal of shoulder and elbow surgery. 2014 Feb:23(2):279-89. doi: 10.1016/j.jse.2013.10.003. Epub [PubMed PMID: 24418780]
Lin DJ, Wong TT, Kazam JK. Shoulder Arthroplasty, from Indications to Complications: What the Radiologist Needs to Know. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 Jan-Feb:36(1):192-208. doi: 10.1148/rg.2016150055. Epub [PubMed PMID: 26761537]
Kane P, Bifano SM, Dodson CC, Freedman KB. Approach to the treatment of primary anterior shoulder dislocation: A review. The Physician and sportsmedicine. 2015 Feb:43(1):54-64. doi: 10.1080/00913847.2015.1001713. Epub 2015 Jan 6 [PubMed PMID: 25559018]
Rouleau DM, Mutch J, Laflamme GY. Surgical Treatment of Displaced Greater Tuberosity Fractures of the Humerus. The Journal of the American Academy of Orthopaedic Surgeons. 2016 Jan:24(1):46-56. doi: 10.5435/JAAOS-D-14-00289. Epub [PubMed PMID: 26700632]
Abzug JM, Ho CA, Ritzman TF, Brighton BK. Transphyseal Fracture of the Distal Humerus. The Journal of the American Academy of Orthopaedic Surgeons. 2016 Feb:24(2):e39-44. doi: 10.5435/JAAOS-D-15-00297. Epub [PubMed PMID: 26808044]
Bauer AS, Pham B, Lattanza LL. Surgical Correction of Cubitus Varus. The Journal of hand surgery. 2016 Mar:41(3):447-52. doi: 10.1016/j.jhsa.2015.12.019. Epub 2016 Jan 16 [PubMed PMID: 26787408]
Chen H, Li D, Zhang J, Xiong X. Comparison of treatments in patients with distal humerus intercondylar fracture: a systematic review and meta-analysis. Annals of medicine. 2017 Nov:49(7):613-625. doi: 10.1080/07853890.2017.1335429. Epub 2017 Jun 14 [PubMed PMID: 28537435]
Level 1 (high-level) evidenceEtier BE Jr, Doyle JS, Gilbert SR. Avascular Necrosis of Trochlea After Supracondylar Humerus Fractures in Children. American journal of orthopedics (Belle Mead, N.J.). 2015 Oct:44(10):E390-3 [PubMed PMID: 26447417]
Niver GE, Ilyas AM. Management of radial nerve palsy following fractures of the humerus. The Orthopedic clinics of North America. 2013 Jul:44(3):419-24, x. doi: 10.1016/j.ocl.2013.03.012. Epub 2013 Apr 24 [PubMed PMID: 23827843]
Simon WH. Soft tissue disorders of the shoulder. Frozen shoulder, calcific tendintis, and bicipital tendinitis. The Orthopedic clinics of North America. 1975 Apr:6(2):521-39 [PubMed PMID: 1093096]
Frassica FJ, Frassica DA. Metastatic bone disease of the humerus. The Journal of the American Academy of Orthopaedic Surgeons. 2003 Jul-Aug:11(4):282-8 [PubMed PMID: 12889867]
Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Current reviews in musculoskeletal medicine. 2008 Dec:1(3-4):190-6. doi: 10.1007/s12178-008-9027-2. Epub [PubMed PMID: 19468905]
Ogden JA, Weil UH, Hempton RF. Developmental humerus varus. Clinical orthopaedics and related research. 1976 May:(116):158-65 [PubMed PMID: 819197]
Ganal-Antonio AK, Samartzis D, Bow C, Cheung KM, Luk KD, Wong YW. Disappearing bone disease of the humerus and the cervico-thoracic spine: a case report with 42-year follow-up. The spine journal : official journal of the North American Spine Society. 2016 Feb:16(2):e67-75. doi: 10.1016/j.spinee.2015.09.056. Epub 2015 Oct 5 [PubMed PMID: 26436955]
Level 3 (low-level) evidenceEllati R, Attili A, Haddad H, Al-Hussaini M, Shehadeh A. Novel approach of treating Gorham-Stout disease in the humerus--Case report and review of literature. European review for medical and pharmacological sciences. 2016:20(3):426-32 [PubMed PMID: 26914115]
Level 3 (low-level) evidenceSchoch B, Werthel JD, Sperling JW, Cofield RH, Sanchez-Sotelo J. Is shoulder arthroplasty an option for charcot arthropathy? International orthopaedics. 2016 Dec:40(12):2589-2595 [PubMed PMID: 27743013]
Wróblewski R, Urban M, Michalik D, Zakrzewski P, Langner M, Pomianowski S. Osteochondrosis of the capitellum of the humerus (Panner's disease, Osteochondritis Dissecans). Case study. Ortopedia, traumatologia, rehabilitacja. 2014 Jan-Feb:16(1):79-90. doi: 10.5604/15093492.1097492. Epub [PubMed PMID: 24728797]
Level 3 (low-level) evidenceSakata R, Fujioka H, Tomatsuri M, Kokubu T, Mifune Y, Inui A, Kurosaka M. Treatment and Diagnosis of Panner's Disease. A Report of Three Cases. The Kobe journal of medical sciences. 2015 Apr 22:61(2):E36-9 [PubMed PMID: 26628012]
Level 3 (low-level) evidence