 Anatomy, Shoulder and Upper Limb, Suprascapular Nerve
Anatomy, Shoulder and Upper Limb, Suprascapular Nerve
Introduction
Suprascapular nerve injury has recently gained popularity as a leading cause of shoulder pain and weakness. The course of the nerve through narrow osseoligamentous structures renders it susceptible to compressional and traction injuries at the suprascapular and spinoglenoid notches. Knowledge of the anatomy of the nerve is necessary to diagnose and provide the best clinical outcomes in cases of suprascapular nerve injury.[1] See Image. The Anterior Divisions, the Suprascapular, Axillary, and Radial Nerves.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The suprascapular nerve is a branch from the upper trunk of the brachial plexus; it innervates the infraspinatus and the supraspinatus muscles. It originates in the posterior triangle of the neck, where it runs to the upper part of the scapula downward and laterally parallel to the belly of the omohyoid muscle. It runs under the suprascapular ligament to the supraspinatus fossa. Here, it provides muscular innervation to the infraspinatus and supraspinatus muscles.[1]
The suprascapular nerve is a mixed nerve, it has both a motor and sensory parts. The suprascapular nerve gives sensory branches to the acromioclavicular and glenohumeral joints, which serve as sensory innervation. The motor part of the suprascapular nerve innervates the supraspinatus and infraspinatus muscles, respectively. The suprascapular nerve originates from the upper trunk of the brachial plexus, the ventral rami of the fifth and sixth cervical nerves from the upper trunk of the brachial plexus join to form the suprascapular nerve, and in approximately 18% of the population, the ventral ramus of the fourth cervical nerve is also involved. The suprascapular nerve branches from the upper trunk and runs along the posterior triangle of the neck. During its course, it runs to the upper part of the scapula downward and laterally parallel to the belly of the omohyoid muscle; then, it runs under the suprascapular ligament to the supraspinatus fossa. In the supraspinous fossa, it runs under the supraspinatus muscle and branches twice for innervation before curving around the lateral border of the spine of the scapula, through the spinoglenoid notch, and into the infraspinous fossa. In the infraspinatus fossa, the nerve branches innervate the infraspinatus muscle.[1][2][3][4] See Image. The Anterior Divisions, Suprascapular and Axillary Nerves of the Right Side.
Embryology
The suprascapular nerve arises from the ventral rami of the fifth and sixth cervical nerves and, in some populations, the ventral ramus of the fourth cervical nerve. Motor nerve roots originate from the ventral ramus of the spinal cord. The ventral (motor) plate begins as a ventrolateral thickening of the intermediate zone of the neural tube. The intermediate zone gives rise to motor neuroblasts of the ventral and lateral horns. Branched axons begin at the motor neuroblast, exit the spinal cord, and become the ventral (motor) roots. The basal plate later becomes the dorsal horn of the spinal cord. the neural crest migrates to the nerve and then differentiates to form the Schwan cells.[5]
Blood Supply and Lymphatics
The suprascapular artery and vein run along with the suprascapular nerve to provide the nerve its blood supply. The suprascapular artery can function either as a branch of the thyrocervical trunk or as a direct branch of the subclavian artery. The artery runs inferolateral to the anterior scalene muscles, phrenic nerve, subclavian artery, and brachial plexus, crossing posterolateral and parallel to the clavicle. Then, the nerve passes superior to the transverse scapular ligament, while the suprascapular nerve passes inferior to it while entering the supraspinous fossa. Finally, the artery courses laterally to the scapular spine (deep to the acromion) and then gains entry to the infraspinous fossa, which is on the posterior surface of the scapula. The suprascapular vein travels parallel to the artery. The lymphatic drainage for the upper limb and area along the suprascapular nerve distribution is primarily from the subscapular (posterior) nodes. The subscapular nodes comprise 6 or 7 lymph nodes along the posterior axillary fold. These lymph nodes run along the course of the subscapular blood vessels. The efferent drainage of the subscapular, pectoral, and humeral nodes passes through the central nodes. The central nodes consist of 4 or 4 nodes found deep within the pectoralis minor near the base of the axilla and the second part of the axilla. Efferent drainage from the central nodes passes to the apical nodes, which lie at the axilla's apex by the axillary vein's medial side and the axillary artery's first part. Efferent vessels that arise from the apical group run across the cervico-axillary canal. These efferent vessels combine to form the subclavian lymphatic trunk. The subclavian lymphatic trunk may join the jugular and bronchomediastinal trunk to form the right lymphatic duct or enter the right venous angle.
Muscles
The suprascapular nerve has a motor and sensory innervation. Its motor innervation is to the supraspinatus and infraspinatus muscles. The supraspinatus and infraspinatus muscles are 2 of the 4 muscles that make up the glenohumeral (shoulder) joint. The supraspinatus muscle originates from the supraspinous fossa of the posterior scapula. It then attaches to the superior facet of the greater tubercle of the humerus. With innervation from the suprascapular nerve, the supraspinatus initiates and aids the deltoid in abduction of the arm and acts in synergy with the rotator cuff muscles. The infraspinatus muscle originates from the infraspinous fossa of the posterior scapula. It then wraps around the lateral proximal humerus to attach to the middle facet of the greater tubercle. The infraspinatus acts to externally rotate the arm and act in synergy with the rotator cuff muscles.
Physiologic Variants
There is not much literature on variants of the suprascapular nerve. Literature by Polguj et al describes 3 variants in the relationship between the superior transverse scapular ligament, suprascapular vessels, and nerve. The first variant, which is the most common, is where the suprascapular artery runs superior to the superior transverse scapular ligament, while the nerve and vein run inferior to the ligament. The second is where the artery and vein run superior to the ligament, and the nerve runs inferior. The least common third variant is where the artery, vein, and nerve pass inferior to the superior transverse scapular ligament.
Surgical Considerations
The suprascapular nerve is at risk during massive rotator cuff repairs. Literature has described the nerve as being close to the operative field used in rotator cuff repairs. The nerve is susceptible near the glenoid rim, rotator cuff footprint, and lateral border of the acromion. The nerve is also at risk of injury near these areas during a double interval slide technique for arthroscopic cuff repairs. The nerve is also at risk for compression neuropathy at the suprascapular and spinoglenoid notch, which is a consideration of suprascapular nerve blocks in treating shoulder pain.
Clinical Significance
The supraspinatus and infraspinatus receive their innervation from the suprascapular nerve. When these muscles show signs of atrophy, the nerve is usually at risk for compression neuropathy. If both muscles show signs of atrophy, then the compression is at the level of the suprascapular notch. When there is isolated atrophy in the infraspinatus muscle, the compression level is at the spinoglenoid notch.
Media
(Click Image to Enlarge)
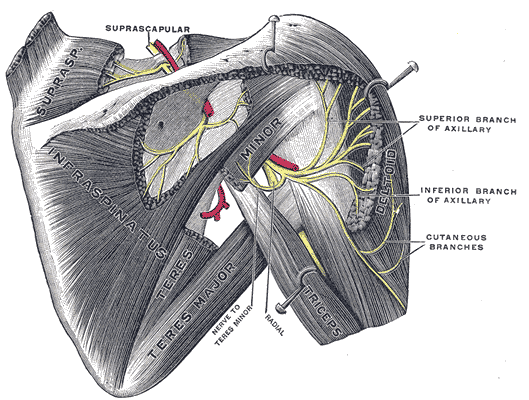
The Anterior Divisions, Suprascapular and Axillary Nerves of the Right Side. Suprascapular and axillary nerves of right side seen from behind, cutaneous branches, nerves to teres minor, and radial nerve.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
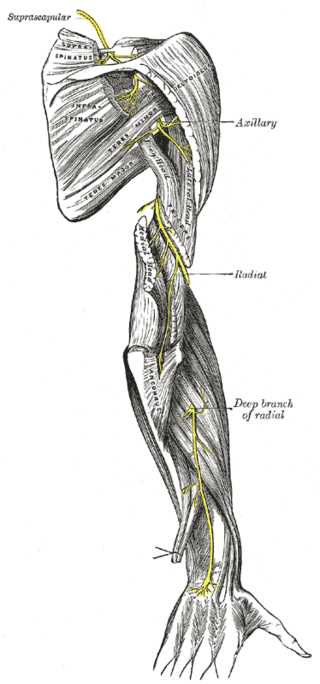
The Anterior Divisions, the Suprascapular, Axillary, and Radial Nerves.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Kostretzis L, Theodoroudis I, Boutsiadis A, Papadakis N, Papadopoulos P. Suprascapular Nerve Pathology: A Review of the Literature. The open orthopaedics journal. 2017:11():140-153. doi: 10.2174/1874325001711010140. Epub 2017 Feb 28 [PubMed PMID: 28400882]
Fernandes MR, Barbosa MA, Sousa AL, Ramos GC. Suprascapular nerve block: important procedure in clinical practice. Revista brasileira de anestesiologia. 2012 Jan-Feb:62(1):96-104. doi: 10.1016/S0034-7094(12)70108-3. Epub [PubMed PMID: 22248771]
Shin C, Lee SE, Yu KH, Chae HK, Lee KS. Spinal root origins and innervations of the suprascapular nerve. Surgical and radiologic anatomy : SRA. 2010 Mar:32(3):235-8. doi: 10.1007/s00276-009-0597-5. Epub 2009 Nov 25 [PubMed PMID: 19937327]
Avery BW,Pilon FM,Barclay JK, Anterior coracoscapular ligament and suprascapular nerve entrapment. Clinical anatomy (New York, N.Y.). 2002 Nov; [PubMed PMID: 12373728]
Catala M, Kubis N. Gross anatomy and development of the peripheral nervous system. Handbook of clinical neurology. 2013:115():29-41. doi: 10.1016/B978-0-444-52902-2.00003-5. Epub [PubMed PMID: 23931773]
Level 3 (low-level) evidence