Introduction
The stomach is the digestive system's most dilated portion. This organ lies between the esophagus, which is superior to it, and the small intestine, which is inferior to it. The stomach is a large, muscular, and hollow organ with a great capacity to hold food. This organ can hold about 2 to 3 liters of food, acting as a blender and food reservoir.[1]
Clinically, stomach disorders such as peptic ulcers and gastric cancer are significant due to their prevalence and potential complications, particularly pain and bleeding. Surgically, the stomach is often involved in procedures like gastrectomy for cancer, bariatric surgery for obesity, and the management of peptic ulcer disease. Effective management of stomach conditions is vital for maintaining overall digestive health and preventing serious complications. Understanding the stomach's anatomy and physiology is crucial for treating various gastrointestinal conditions.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Structure
The stomach is located on the left of the midline and centrally in the upper abdominal area. This organ comprises 4 main regions: the cardia, fundus, body, and pylorus. The cardia is connected to the esophagus and is the segment where food first enters the stomach. Following the cardia inferiorly is the fundus, a bulbous, dome-shaped gastric region. Distal to the fundus is the body, the stomach's largest portion. The pylorus follows the body inferiorly, funneling food into the duodenum, the most superior segment of the small intestine (see Image. Stomach Anatomical Landmarks). Digestion in the stomach occurs after mastication and deglutition.[2][3][4]
Relations of the stomach
The stomach is an intraperitoneal organ. The 2 layers of the lesser omentum run from the inferior surface of the liver toward the lesser curvature of the stomach. The 2 layers envelop the stomach and continue as the greater omentum at the greater curvature. The diaphragm, left hepatic lobe, and anterior abdominal wall are situated anterior to the stomach. Meanwhile, the structures posterior to this organ lie deep to the lesser sac (omental bursa). Structures behind the posterior wall of the lesser sac are thus related to the stomach posteriorly. These structures include the pancreas, left diaphragm dome, the spleen, left kidney and suprarenal gland, splenic artery, and transverse mesocolon.
Layers of the stomach
Four layers constitute the stomach wall: the mucosa, submucosa, muscularis externa, and serosa. The innermost layer, the mucosa, is covered by epithelial tissue and mainly comprises gastric glands that secrete gastric juices. The fundus secretes gastric juices. The cardia secretes protective mucus, which coats the inner gastric mucosal wall via mucus (Foveolar) cells. Mucus protects the stomach wall from being digested by the gastric juices produced by the chief cells (pepsin) and parietal cells (HCl). The submucosa comprises dense connective tissue and contains blood, lymphatic vessels, and nerves. The submucosa supports the mucosal layer. This layer has many folds analogous to that of an accordion called "rugae," allowing for intraluminal distension when food enters the stomach.
The muscularis externa, explained further under "Muscles," surrounds the submucosa (see Muscles). The serosa is the outermost layer, comprising multiple strata of connective tissue that network with the peritoneum (see Image. Stomach Exterior and Interior Aspects).
Function
The primary functions of the stomach include the temporary storage and partial chemical and mechanical digestion of food. The upper portions of the stomach (ie, cardia, fundus, and body) relax as food enters to allow the stomach to hold increasing quantities of food. The lower portion of the stomach contracts rhythmically to break down food mechanically. The food bolus mixes with stomach juices in the lower gastric region, degrading food chemically. Partially digested food then becomes a mixture, termed "chyme" at this point of digestion. Mixing waves are produced at intervals of about 20 seconds, increasing in intensity as they reach the inferior gastric regions. With each wave, the pyloric sphincter allows small quantities of sufficiently liquefied chyme into the small intestine. Chyme is further digested in the duodenum.
Stomach juices are liquids naturally secreted by the fundus cells to chemically digest food. Stomach juices include hydrochloric acid (HCl) and the enzyme pepsin. HCl is produced by the gastric parietal cells. The enzyme pepsin is a breakdown product of the proenzyme pepsinogen secreted by the gastric chief cells. Pepsinogen is converted to pepsin after mixing with HCl.
Besides HCl, gastric parietal cells produce intrinsic factor, a glycoprotein critical to the transportation and absorption of vitamin B12 (cobalamin) distally in the small intestine's terminal ileum. Intrinsic factor production is vital, as vitamin B12 is essential for red blood cell production and neurological function.[5][6]
The stomach can process food and transport it to the duodenum within 2 to 4 hours. However, this rate heavily depends on the type of food consumed. Carbohydrates and proteins are broken down in the stomach relatively fast, as opposed to lipids like triglycerides, which take longer to be processed by the stomach. The stomach does not primarily absorb nutrients. However, this organ can absorb some substances, including water (during dehydration states) and certain medications, including aspirin, amino acids, ethanol, caffeine, and water-soluble vitamins.
The stomach also has neuroendocrine cells, including the gastrin-producing G cells, that synthesize various hormones vital for regulating acid production and gastric motility. The surface mucous cells secrete a layer of mucus, which protects the stomach wall from its acidic environment. Gastric acid may be lethal to many types of bacteria and other microorganisms that enter the body through ingestion, protecting the body from infection and disease.[7][8]
Embryology
The stomach appears during the 4th week of development, becoming the foregut's most dilated portion. This organ descends from the C2 to the T11 vertebral level by week 12 due to rapid esophageal elongation. By the 5th week of development, the dorsal wall starts to grow faster than the ventral wall. This disproportionate growth gives rise to the greater and lesser curvatures, giving the stomach its characteristic shape.
During week 7 of growth, the stomach rotates 90° clockwise about the longitudinal axis, causing the right side to turn posteriorly and the left anteriorly. Stomach rotation changes the positions of the organ's nerves. The right vagus nerve, initially supplying the right gastric area, shifts to the posterior wall. Similarly, the left vagus nerve moves from the left to the anterior wall. With further development, the stomach undergoes clockwise rotation about the anteroposterior axis during the 8th week, pulling the pyloric region upward to the right and the cardiac portion downward to the left.
Blood Supply and Lymphatics
The stomach is a highly mobile and distensible organ with a rich blood supply. This organ has 5 different cell types functioning at high metabolic rates and multiple muscle layers to facilitate waves of brisk peristalsis for the 2nd phase of digestion.
The celiac trunk, branching directly anteriorly from the aorta at the T12 vertebral level, provides the stomach's main arterial supply. The celiac trunk supplies the common hepatic (CHA), splenic, and left gastric (LGA) arteries. A descending branch of the LGA proximally supplies the lesser curvature, while its ascending branch perfuses portions of the distal esophagus. The CHA courses to the right of the celiac trunk, runs superior to the pancreas, gives off the gastroduodenal artery (GDA), and continues as the proper hepatic artery. The proper hepatic artery gives off the right gastric artery (RGA), which runs from right to left along the inferior area of the lesser curvature and branches into smaller vessels through the gastric body to join the network of smaller arteries branching from the LGA. The LGA and RGA supply the lesser curvature.
The GDA runs posterior to the 1st part of the duodenum and gives off the right gastroomental (gastroepiploic) artery (RGOA). The RGOA then traverses from right to left to supply the greater curvature. The left gastroomental artery (LGOA) branches off the splenic artery, supplies the greater curvature, and anastomoses with the RGOA. About 3 to 5 short gastric arteries also branch off from the splenic artery to supply the gastric fundus.
The veins of the stomach mimic the arterial supply in position and course. The left and right gastric veins drain into the portal vein. The short gastric and left gastroomental veins drain into the splenic vein. The splenic vein joins the superior mesenteric vein to form the portal vein. The right gastroomental veins drain into the superior mesenteric vein.
The stomach's lymphatic drainage is multidirectional, with a complex system of lymphatic vessels and nodes. These lymphatics run alongside the arteries of the lesser and greater curvatures, draining lymph from the anterior and posterior surfaces toward the gastric and gastroomental lymph nodes. The efferent lymphatics from most of the lymph nodes ultimately reach the celiac lymph nodes after passing through intermediary nodes.
The lymph from the stomach characteristically drains into 4 zones. Zone 1 includes the gastric lymph nodes, which drain lymphatic vessels from the cardia and the upper right two-thirds of the stomach. Zone 2 encompasses lymph from the lower right two-thirds of the organ, which drains into the suprapyloric lymph nodes. Zone 3 includes lymphatic vessels from the body and fundus (upper left one-third of the stomach), tracking along the left gastroomental and short gastric arteries to the pancreaticosplenic lymph nodes. Zone 4 contains lymph from the lower left one-third of the stomach, traversing the right gastroomental vessels and draining into the subpyloric lymph nodes.[9][10]
Nerves
The vagus nerve supplies the stomach's parasympathetic innervation via the anterior and posterior vagal fibers. Stomach rotation during development positions the left vagus nerve anteriorly and the right vagus nerve posteriorly. The anterior and posterior vagal fibers travel toward the lesser curvature and give rise to anterior and posterior gastric branches, respectively. The stomach's sympathetic innervation arises from the T5 to T9 spinal cord segments via the greater splanchnic nerve, which transits toward the celiac plexus to be distributed along with the region's arterial supply.
The Auerbach or myenteric plexus is a network of neurons located between the longitudinal and circular layers of the gastrointestinal tract's muscularis externa. This plexus regulates gut motility. The Meissner or submucosal plexus is situated within the submucosal layer. The Meissner plexus primarily regulates local blood flow and gastric secretion. The Auerbach and Meissner plexuses are part of the enteric nervous system, an autonomous and extensive network of neurons comprising what is known as the "brain of the gut."[11][12]
Muscles
The muscularis externa has thick, smooth muscle tissue arranged in 3 layers, running longitudinally, obliquely, and circularly as part of the stomach wall. The inner oblique layer is unique to the stomach and is primarily responsible for food churning and mechanical digestion. The middle circular layer is concentric with the stomach’s longitudinal axis. This layer thickens in the pylorus region to form the pyloric sphincter, which regulates the output from the stomach into the duodenum. The outer longitudinal layer surrounds the middle layer. The Auerbach (myenteric) plexus runs between the outer longitudinal and middle circular muscle layers. Contractions of the outer longitudinal layer facilitate food movement toward the pylorus.
Physiologic Variants
The stomach does not have many natural physiological variations. However, variability often arises from differences in the organ's exact position, size, and shape, which may be heavily related to diet. For example, rugae may remain distended in individuals who overeat frequently. Congenital anomalies involving the stomach include gastric outlet obstruction, duplication, transposition, diverticula, and bilocular (hourglass) contraction.
Surgical Considerations
Stomach conditions requiring surgery include cancers, ulcers, and perforations. The stomach is also the target organ of bariatric surgeries for weight reduction, such as gastric bypass surgery and banding. Laparoscopic surgery is recommended where applicable and possible to promote minimally invasive access to the stomach and facilitate quicker patient recovery. Various radiographic techniques may be used to evaluate the stomach. Endoscopy can also be used to evaluate the stomach for surgical planning.[13][14]
Clinical Significance
Early detection of stomach problems helps prevent significant damage to the organ and the patient's overall health. As a primary digestive organ, the stomach is crucial in the delivery of food to the duodenum. Consequently, stomach disorders can impair a patient's nutritional well-being by disrupting the digestion and delivery of essential nutrients.
Several clinical conditions affect the stomach, including gastroesophageal reflux disease (GERD), characterized by the continuous reflux of stomach acid into the esophagus, often presenting with symptoms like heartburn, regurgitation, dysphagia, chronic cough, and hoarseness.[15] GERD is crucial to treat due to its association with esophageal adenocarcinoma risk. Dyspepsia causes frequent stomach discomfort and indigestion, while gastric ulcers result from stomach acid erosion of the stomach lining.[16][17] Stomach tumors, bleeding, and cancer can also occur. Treatment typically involves medications like histamines, proton pump inhibitors, and antacids to reduce stomach acid, motility agents to aid muscle contractions, and antibiotics to treat infections such as Helicobacter pylori.[18]
Media
(Click Image to Enlarge)
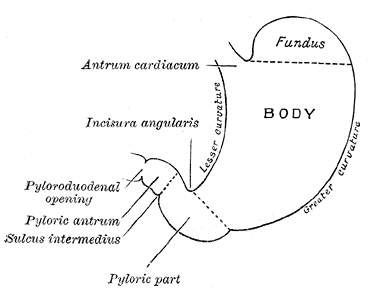
Stomach Anatomical Landmarks. An illustration of the stomach showing its anatomical landmarks, including the fundus, lesser and greater curvatures, body, pylorus, pyloric antrum, pyloroduodenal opening, sulcus intermedius, incisura angularis, and cardiac antrum.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
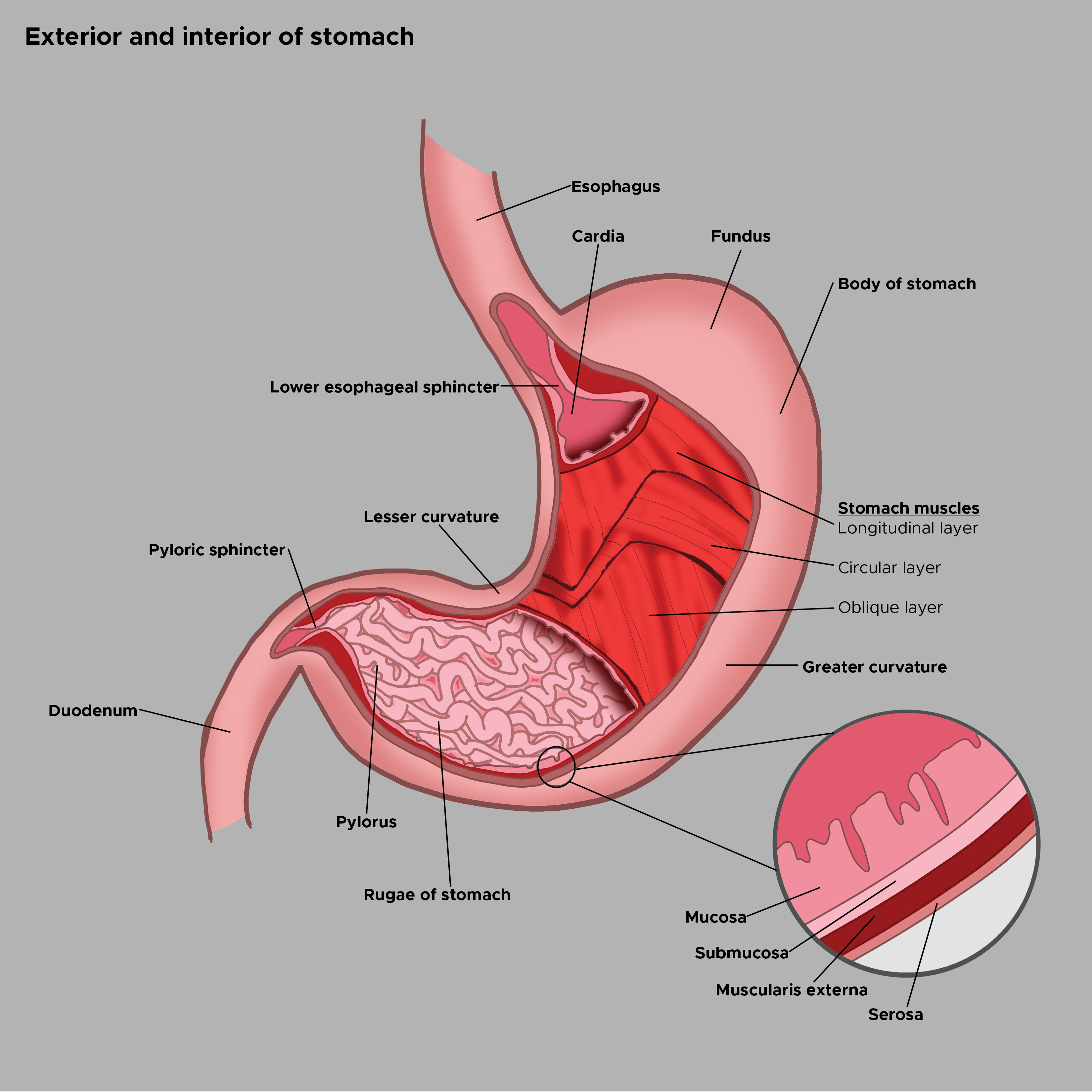
Stomach Exterior and Interior Aspects. The illustration shows the exterior landmarks for the stomach's cardia, fundus, body, lesser and greater curvatures, pylorus, and pyloric sphincter. The interior lining of the stomach comprises the mucosa, submucosa, and muscularis externa, all covered by the serosal layer. The muscularis externa is comprised of the inner oblique, middle circular, and outer longitudinal layers. The lower esophageal sphincter and stomach rugae are also shown. The esophagus and duodenum are included for reference.
Contributed by C Rowe
References
Hosoda K, Watanabe M, Yamashita K. Re-emerging role of macroscopic appearance in treatment strategy for gastric cancer. Annals of gastroenterological surgery. 2019 Mar:3(2):122-129. doi: 10.1002/ags3.12218. Epub 2018 Oct 19 [PubMed PMID: 30923781]
Shaikh H, Wehrle CJ, Khorasani-Zadeh A. Anatomy, Abdomen and Pelvis: Superior Mesenteric Artery. StatPearls. 2024 Jan:(): [PubMed PMID: 30137844]
Lopez PP, Gogna S, Khorasani-Zadeh A. Anatomy, Abdomen and Pelvis: Duodenum. StatPearls. 2024 Jan:(): [PubMed PMID: 29494012]
Collins JT, Nguyen A, Badireddy M. Anatomy, Abdomen and Pelvis, Small Intestine. StatPearls. 2024 Jan:(): [PubMed PMID: 29083773]
Cheng J, Wu J, Ye Y, Zhang C, Zhang Y, Wang Y. The prognostic significance of extramural venous invasion detected by multiple-row detector computed tomography in stage III gastric cancer. Abdominal radiology (New York). 2016 Jul:41(7):1219-26. doi: 10.1007/s00261-015-0627-1. Epub [PubMed PMID: 27315092]
Fagoonee S, Pellicano R. Helicobacter pylori: molecular basis for colonization and survival in gastric environment and resistance to antibiotics. A short review. Infectious diseases (London, England). 2019 Jun:51(6):399-408. doi: 10.1080/23744235.2019.1588472. Epub 2019 Mar 25 [PubMed PMID: 30907202]
Gonsalves N. Eosinophilic Gastrointestinal Disorders. Clinical reviews in allergy & immunology. 2019 Oct:57(2):272-285. doi: 10.1007/s12016-019-08732-1. Epub [PubMed PMID: 30903439]
Pimentel AM, Rocha R, Santana GO. Crohn's disease of esophagus, stomach and duodenum. World journal of gastrointestinal pharmacology and therapeutics. 2019 Mar 7:10(2):35-49. doi: 10.4292/wjgpt.v10.i2.35. Epub [PubMed PMID: 30891327]
Cho HS, Ahn JH. Nomenclature and Lymphatic Drainage Patterns of Abdominal Lymph Nodes. Journal of the Korean Society of Radiology. 2022 Nov:83(6):1240-1258. doi: 10.3348/jksr.2021.0189. Epub 2022 May 23 [PubMed PMID: 36545415]
Lirosi MC, Biondi A, Ricci R. Surgical anatomy of gastric lymphatic drainage. Translational gastroenterology and hepatology. 2017:2():14. doi: 10.21037/tgh.2016.12.06. Epub 2017 Mar 1 [PubMed PMID: 28447049]
El Munshid HA. The brain of the gut. Saudi journal of gastroenterology : official journal of the Saudi Gastroenterology Association. 2000 Jan:6(1):18-26 [PubMed PMID: 19864724]
Hsu M, Safadi AO, Lui F. Physiology, Stomach. StatPearls. 2024 Jan:(): [PubMed PMID: 30571046]
PDQ Screening and Prevention Editorial Board. Stomach (Gastric) Cancer Prevention (PDQ®): Health Professional Version. PDQ Cancer Information Summaries. 2002:(): [PubMed PMID: 26389263]
Stern E, Sugumar K, Journey JD. Peptic Ulcer Perforated. StatPearls. 2024 Jan:(): [PubMed PMID: 30855910]
Clarrett DM, Hachem C. Gastroesophageal Reflux Disease (GERD). Missouri medicine. 2018 May-Jun:115(3):214-218 [PubMed PMID: 30228725]
Medić B, Babić Ž, Banić M, Ljubičić L. MODERN APPROACH TO DYSPEPSIA. Acta clinica Croatica. 2021 Dec:60(4):731-738. doi: 10.20471/acc.2021.60.04.21. Epub [PubMed PMID: 35734496]
Woolf A, Rose R. Gastric Ulcer. StatPearls. 2024 Jan:(): [PubMed PMID: 30725813]
Fischbach W, Malfertheiner P. Helicobacter Pylori Infection. Deutsches Arzteblatt international. 2018 Jun 22:115(25):429-436. doi: 10.3238/arztebl.2018.0429. Epub [PubMed PMID: 29999489]