Introduction
Mindfulness is a self-regulated state of non-judgemental and purposeful awareness of the present moment.[1] Psychotherapy pioneer Jon Kabat-Zinn developed the mindfulness-based stress reduction (MBSR) protocol for the self-regulation of chronic pain and stress through meditation and mindfulness.[2] In preliminary studies, Kabat-Zinn describes how meditation facilitates a state of detached observation by redirecting attention toward proprioception.[2] This "uncouples" the sensory component of pain from the affective or emotional element, thus reducing suffering through cognitive reappraisal.[2] Individuals can reinterpret and reframe their thoughts through cognitive reappraisal, reducing stress and suffering. Studies report strong adherence and long-term positive effects of MBSR on stress, depression, anxiety, and pain following the training period, with benefits lasting for several years.[3][2] A pivotal study on mindfulness and the brain demonstrated that a brief MBSR program increased left-sided anterior activity correlated with positive affect.[4]
More recent research further supports this finding, indicating that mindfulness meditation reduces stress and enhances the activation of brain regions linked to mood regulation and attention control.[5] Specifically, it is suggested that MBSR improves the activation of the brain's anterior cingulate cortex, an executive attention center.[5] These findings highlight how mindfulness strengthens neuronal networks, cultivating self-awareness, emotional regulation, and adaptive stress responses.[5] Furthermore, mindfulness may strengthen the mind-body connection, enabling individuals to effectively self-regulate symptoms of pain, anxiety, depression, and stress.[6] Mindfulness aims to liberate the self from physical and psychological suffering while cultivating the necessary skills to manage stressful situations.[7] It is emphasized that mindfulness is not a quick fix but a long-term intervention that requires dedicated practice and an intentional way of living.
Stress is a fundamental and necessary part of life. Stress is not exclusive to negative experiences and may result from any form of stimulation, including positive experiences.[8] Cortisol, the stress hormone, is produced during negative and positive experiences and is crucial in promoting alertness, focus, and energy. It allows us to get up in the morning and maintain energy throughout the day. However, prolonged or excessive stress can have detrimental effects on our health. High cortisol levels over an extended period can disrupt sleep patterns, impair cognitive function, weaken the immune system, and contribute to various health problems.[9] Therefore, while stress is essential in moderate amounts, it is crucial to manage excessive stress to maintain a healthy lifestyle. The body's response to stressors can be observed through physiological and behavioral changes controlled by biological processes.[9]
Recent research supports the theory that the hypothalamic-pituitary-adrenal (HPA) axis regulates the stress response.[9] Activation of the HPA axis begins through an initial exposure to a stressor. The activation of the HPA axis has neuronal origins regulated by the paraventricular nucleus of the hippocampus, which releases corticotropin-releasing factors.[10] The HPA axis then releases glucocorticoids, stimulating the body's physical response to stress.[10]
Glucocorticoids and other cortical hormones are major regulators of the HPA axis and normally produce a healthy, adaptive stress response. However, chronic stress results in excessive or prolonged activation of the HPA axis, leading to dysregulation and a maladaptive stress response.[10] A wide body of evidence supports using a mind-body approach to regulate the HPA axis and address psychophysiological stress.[11][12][13] Non-pharmacological behavioral interventions like MBSR have been shown to effectively regulate exaggerated or problematic stress responses through breathing exercises, meditation, and mindfulness (see Image. MSBR and Stress).[6] Behavioral interventions like MBSR aim not to remove stress but to manage it effectively and completely.
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
MBSR Protocol
Jon Kabat-Zinn developed the Mindfulness-Based Stress Reduction protocol in the 1980s.[2] The MBSR protocol is implemented over 8 consecutive weeks, improving awareness of health and reducing stress. The program requires that participants attend a weekly, 2-hour group class that teaches non-religious meditation-based behavioral techniques to manage stress.[2][7] The meditation-based techniques include Hatha Yoga, breathing exercises, sitting meditations, and "body scans." The protocol assigns homework through yoga and meditation sessions lasting 45 minutes daily, 6 days a week. Participants supplement the meditation and yoga study with guided audio recordings. Using a workbook, participants must also engage in awareness exercises for 15 minutes daily. On the 6th week of the program, participants attend an 8-hour-long retreat. The goal of practicing mindfulness-based techniques daily is to establish their efficacy as a sustainable, lifelong intervention.
Body Scanning
An essential meditation technique used in MBSR is the "body scan." This meditation is performed lying down and involves energetically "sweeping" the body with the mind.[14] The guided body scan directs the meditator to visualize a "compassionate awareness" starting at the tip of their toes that slowly progresses from their feet, going up their legs, passing through their pelvic region, hips, buttocks, abdomen, ribs, chest, lungs, shoulder blades, fingers, and arms, then back up to the shoulders and through the neck, throat, face, and head.[14] Along the way, the guide will instruct the meditator to recognize certain anatomical areas like the heart, throat, or pelvic region, which may hold particularly emotional or strong memories.[14]
The body scan meditation can also be self-guided. This allows the meditator to spend more time scanning certain areas of the body, which may hold the personal significance of past experiences and emotions, before moving on to the next region. The MBSR protocol includes 45 minutes of daily body scan meditation and breathing exercises. The benefits of body scan meditation have been studied in research. A recent functional magnetic resonance imaging (fMRI) study found that body scan meditation increases interoceptive awareness by enhancing the connection between the salience network and frontal/central gyri.[15] The same study found that the body scan improved emotional regulation, which persisted after the MBSR intervention.[15]
Hatha Yoga
A critical component of MBSR is Hatha yoga. Like other forms of yoga, Hatha yoga integrates a series of physical poses and structured movements known as "asanas" with breathing exercises known as "pranayamas."[16] A popular breathwork technique used in Hatha yoga is diaphragmatic breathing. This breathing technique involves a deep and prolonged inhalation, a period of breath retention, and a slow, controlled exhalation.[16] Diaphragmatic breathing has been proven to reduce cortisol levels produced by the HPA axis during the stress response.[17] Research on Hatha yoga reports improved attention, concentration, psychological distress, and sleep quality.[18][19] These findings highlight the critical role of Hatha yoga in MBSR.
Issues of Concern
Anxiety MBSR
Pharmacotherapy has usually been the first-line treatment for anxiety. However, psychotherapy programs such as mindfulness-based stress reduction are especially effective for individuals suffering from mental health conditions like anxiety.[20][6] Treatment using MBSR therapy is performed similarly to escitalopram, a popular anxiety medication.[20] Through MBSR training, individuals with generalized anxiety disorder experienced decreased inflammatory cytokines and a decrease in HPA axis effectors like adrenocorticotropic hormone.[13] Mindfulness-based stress reduction training was reported to be more effective than general stress management education at improving generalized anxiety disorder.[13]
The successful regulation of the HPA axis can reduce cortisol levels, improving symptoms of stress and anxiety.[21] One study utilized fMRI to demonstrate the neural effects of MBSR training on individuals with social anxiety disorder.[22] The training resulted in (1) an increase in neural network activity in areas of the brain associated with attention regulation, (2) a reduction in neural activity in the parts of the brain associated with conceptual self-view, and (3) a decrease in reported anxiety.[22]
Depression MBSR
MBSR is a promising and increasingly popular treatment option for depression. An increasing number of patients prefer psychotherapy over pharmacotherapy to treat depression.[23] Clinicians must honor patient preference as it strongly predicts successful outcomes.[23] Furthermore, several meta-analyses report that mindfulness-based interventions significantly improved depressive symptoms and provided comparable outcomes to standard care interventions.[24][25] Several studies found that MBSR training significantly reduced depression in healthy individuals and those suffering from chronic illnesses like cancer.[26][27][28]
Similar to other forms of psychotherapy, there is concern that moderating variables like spirituality, religiosity, or age sway the benefits of MBSR. A recent study examined the most common moderating variables and proved that an MBSR treatment program improved depressive symptoms across all groups, regardless of trait mindfulness, age, spirituality, or religiosity.[29] Psychotherapy like MBSR can be used alone or in combination with other interventions like pharmacotherapy to address the unique needs of every individual patient.[30]
Stress MBSR
Stress is detrimental to health and results in adverse physical and psychological consequences. One study examined the effect of MBSR on healthy individuals and found that participation in an MBSR program reduced symptoms of stress while enhancing mindfulness and self-compassion.[31] Meta-analyses describe similar results among healthy individuals, including increased self-compassion, reduction of stress symptoms, and even a reduction in symptoms of anxiety and reflective thinking.[32][28]
Generally, MBSR may provide nonspecific benefits for health and wellness. However, MBSR may also be a specific intervention for chronic illness and other stress-inducing states. Studies have examined the effect of MBSR training on cancer patients and reported reductions in stress-induced cardiopulmonary and gastrointestinal symptoms, emotional irritability, mood disturbances, and even a 31% decrease in overall stress.[27][26] Additional research demonstrates that the training reduced perceived medical symptoms, including pain, in populations suffering from chronic illnesses.[33][34] In addition, MBSR produced a sustainable reduction in symptoms of stress and anxiety in individuals working high-demand jobs, including healthcare and teaching.[35][36]
Pain
The consequences of the opioid epidemic popularized MBSR as an alternative or complement to pharmaceutical use.[37] Long-term use of opioids is correlated with a lack of therapeutic efficacy, addiction, and hyperalgesia, highlighting the need for treatment alternatives.[38] Approximately two-thirds (65%) of the patients in a preliminary study on MBSR experienced a ≥33% reduction in pain in the following categories: back, facial, neck, headache, shoulder, noncoronary chest pain, and GI pain.[39][2] Additionally, some participants experienced a statistically significant reduction in physical pain and mood disturbances.[39][2] Further research on MBSR and chronic pain demonstrates significant reductions in medication reliance and present-moment pain, with some patients reporting reduced medication use by the study's end.[7]
A more recent study further supports these findings, showing a 30% improvement in long-term clinical symptoms of lower back pain.[40] Recent research on lower back pain found that MBSR produced more clinically meaningful pain improvement than usual care interventions.[41] The benefits of MBSR extend to patients with chronic headaches, fibromyalgia, and general bodily pain, significantly reducing perceived pain severity across pain types.[42] MBSR can complement standard care by providing a multimodal treatment approach for individuals with chronic conditions like fibromyalgia. Several studies have shown that integrating MBSR with usual care significantly reduces chronic pain and improves the quality of life for fibromyalgia patients.[2][43] Non-pharmacological pain treatments offer extensive benefits beyond pain relief, enhancing their overall quality of life and functional capacity. As a result, psychotherapy is recommended as the first-line treatment for chronic pain.[37]
Clinical Significance
Healthcare Delivery
Provider mindfulness has been proposed for integration into regular medical practice. Mindfulness teaches presence, self-reflection, and non-judgment and may enhance clinician decision-making and technical competence.[44] Present-moment awareness allows providers to engage with the patient fully and to be free from preoccupations. This “presence” facilitates accurate assessment, diagnosis, and treatment planning while fostering a patient-centered environment. Self-reflection encourages clinicians to recognize errors and refine clinical skills.[44] A mindful clinician may suspend preconceived biases and allow curiosity and compassion to lead their care. Conversely, mindlessness may result in technical errors like anchoring bias, judgment errors, and attribution errors (stereotyping).[44][1] A recent study involving healthcare workers found that an MBSR program increased feelings of common humanity, self-compassion, and awareness while reducing reactivity and judgment.[45] The valuable contribution of MBSR to healthcare delivery is evident and warrants greater utilization.
Clinical Application
The acceptability and accessibility of mindfulness-based interventions is the greatest barrier to patient utilization. Patients may believe pain medication is the only approach to treating chronic pain, disregarding the potential effectiveness of non-pharmacological interventions. Providers can address the issue of acceptability by educating patients about the biological process of pain regulation and highlighting compelling evidence that supports mindfulness interventions. Clinicians can support their recommendations with the following evidence: (1) pain regulation involves top-down processing which is not fully engaged during pharmacotherapy, (2) meditation engages central brain networks that are involved in pain regulation, (3) pain medication carries the risk of dependency and can induce hyperalgesia, a condition characterized by increased sensitivity to pain, (4) mindfulness interventions reduce pain in the long term and help maintain functional capacity, (5) MBSR has been shown to decrease levels of inflammatory cytokines, and stress hormones ACTH and cortisol.[37][13]
Furthermore, the lack of clarity surrounding the accessibility of mindfulness-based interventions often discourages patients from seeking them out. Clinicians should guide patients to online and telephone-based programs or refer them to individual or group therapy sessions at local mindfulness centers. It is essential to discuss self-implementation strategies to address personal barriers and to empower patients to participate in the treatment process. Providers can enhance their treatment approaches by incorporating MBSR as a complementary intervention. The clinical application and efficacy of MBSR may open the door to a transformative approach to how medicine addresses chronic conditions.
Enhancing Healthcare Team Outcomes
Pain and Psychological Conditions
Stress, pain, depression, and anxiety are conditions that can significantly impact an individual's well-being and overall quality of life. These conditions may coexist and exacerbate each other, leading to a complex and challenging clinical presentation. Mindfulness-based stress reduction (MBSR) is a valuable intervention for individuals struggling with pain, depression, stress, and anxiety. MBSR combines meditation, yoga, and other contemplative practices to cultivate a non-judgmental awareness of the present moment. By incorporating mindfulness into their daily lives, individuals can develop skills to manage pain better, regulate emotions, and manage stressful situations.
Evidence-based Approach
The interprofessional team plays a crucial role in the evaluation and treatment of individuals with pain, stress, depression, and anxiety. Collaborating professionals, including physicians, psychologists, psychiatrists, and therapists, work together to assess and comprehensively address the multifaceted aspects of these conditions. Through shared decision-making and effective communication, the interprofessional team tailors personalized treatment plans that may include a combination of pharmacological interventions, psychotherapy, mindfulness-based interventions like MBSR, and other complementary approaches. MBSR therapy is an evidence-based approach in the Lifestyle Medicine Board Review Manual.[46]
Media
(Click Image to Enlarge)
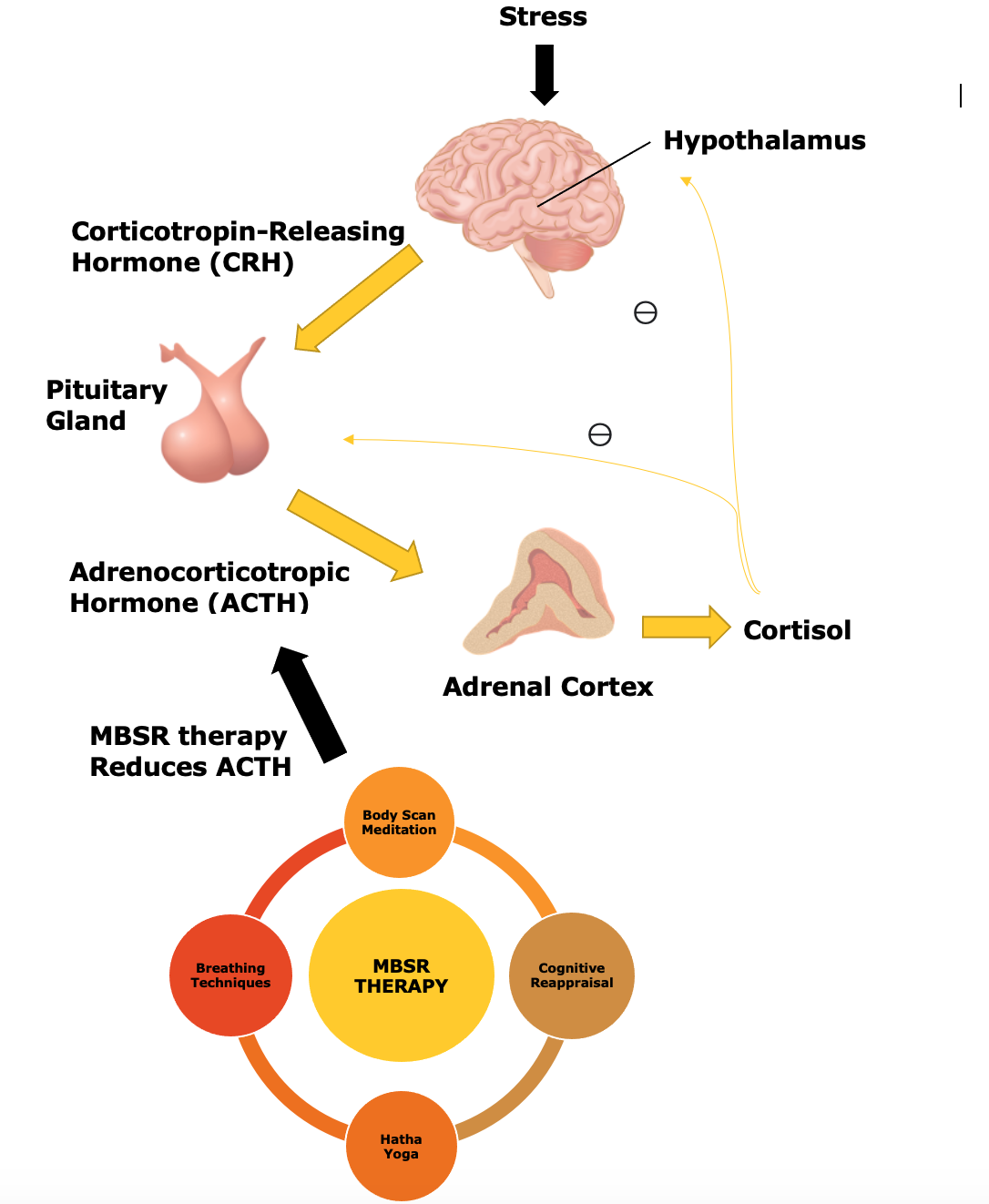
MSBR and Stress. MBSR training leads to a reduction in ACTH levels produced during stressful tasks. ACTH controls cortisol production. Less cortisol is produced, dampening the physiological stress response.
https://commons.wikimedia.org/wiki/File:201405_pituitary_gland.png, licensed under the Creative Commons Attribution 4.0 International https://en.wikipedia.org/wiki/File:201405_adrenal_medulla.png licensed under the Creative Commons Attribution 4.0 International https://commons.wikimedia.org/wiki/File:Human_Brain.png licensed under the Creative Commons Attribution 4.0 International
References
Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008 Sep 17:300(11):1350-2. doi: 10.1001/jama.300.11.1350. Epub [PubMed PMID: 18799450]
Kabat-Zinn J, Chapman-Waldrop A. Compliance with an outpatient stress reduction program: rates and predictors of program completion. Journal of behavioral medicine. 1988 Aug:11(4):333-52 [PubMed PMID: 3070046]
Santamaría-Peláez M, González-Bernal JJ, Verdes-Montenegro-Atalaya JC, Pérula-de Torres LÁ, Roldán-Villalobos A, Romero-Rodríguez E, Hachem Salas N, Magallón Botaya R, González-Navarro TJ, Arias-Vega R, Valverde FJ, Jiménez-Barrios M, Mínguez LA, León-Del-Barco B, Soto-Cámara R, González-Santos J. Mindfulness-Based Program for Anxiety and Depression Treatment in Healthcare Professionals: A Pilot Randomized Controlled Trial. Journal of clinical medicine. 2021 Dec 17:10(24):. doi: 10.3390/jcm10245941. Epub 2021 Dec 17 [PubMed PMID: 34945237]
Level 1 (high-level) evidenceDavidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, Urbanowski F, Harrington A, Bonus K, Sheridan JF. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic medicine. 2003 Jul-Aug:65(4):564-70 [PubMed PMID: 12883106]
Level 1 (high-level) evidenceTang YY, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nature reviews. Neuroscience. 2015 Apr:16(4):213-25. doi: 10.1038/nrn3916. Epub 2015 Mar 18 [PubMed PMID: 25783612]
Hofmann SG, Gómez AF. Mindfulness-Based Interventions for Anxiety and Depression. The Psychiatric clinics of North America. 2017 Dec:40(4):739-749. doi: 10.1016/j.psc.2017.08.008. Epub 2017 Sep 18 [PubMed PMID: 29080597]
Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of behavioral medicine. 1985 Jun:8(2):163-90 [PubMed PMID: 3897551]
Lu S, Wei F, Li G. The evolution of the concept of stress and the framework of the stress system. Cell stress. 2021 Apr 26:5(6):76-85. doi: 10.15698/cst2021.06.250. Epub 2021 Apr 26 [PubMed PMID: 34124582]
Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nature reviews. Neuroscience. 2009 Jun:10(6):397-409. doi: 10.1038/nrn2647. Epub [PubMed PMID: 19469025]
Level 3 (low-level) evidenceSmith SM, Vale WW. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues in clinical neuroscience. 2006:8(4):383-95 [PubMed PMID: 17290797]
Level 3 (low-level) evidenceManigault AW, Shorey RC, Hamilton K, Scanlin MC, Woody A, Figueroa WS, France CR, Zoccola PM. Cognitive behavioral therapy, mindfulness, and cortisol habituation: A randomized controlled trial. Psychoneuroendocrinology. 2019 Jun:104():276-285. doi: 10.1016/j.psyneuen.2019.03.009. Epub 2019 Mar 18 [PubMed PMID: 30917336]
Level 1 (high-level) evidencePuhlmann LMC, Vrtička P, Linz R, Stalder T, Kirschbaum C, Engert V, Singer T. Contemplative Mental Training Reduces Hair Glucocorticoid Levels in a Randomized Clinical Trial. Psychosomatic medicine. 2021 Oct 1:83(8):894-905. doi: 10.1097/PSY.0000000000000970. Epub [PubMed PMID: 34259441]
Level 1 (high-level) evidenceHoge EA, Bui E, Palitz SA, Schwarz NR, Owens ME, Johnston JM, Pollack MH, Simon NM. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry research. 2018 Apr:262():328-332. doi: 10.1016/j.psychres.2017.01.006. Epub 2017 Jan 26 [PubMed PMID: 28131433]
Roll SC, Hardison ME, Vigen C, Black DS. Mindful Body Scans and Sonographic Biofeedback as Preparatory Activities to Address Patient Psychological States in Hand Therapy: A Pilot Study. Hand therapy. 2020 Sep:25(3):98-106. doi: 10.1177/1758998320930752. Epub 2020 Jun 9 [PubMed PMID: 33244321]
Level 3 (low-level) evidenceGuu SF, Chao YP, Huang FY, Cheng YT, Ng HH, Hsu CF, Chuang CH, Huang CM, Wu CW. Interoceptive awareness: MBSR training alters information processing of salience network. Frontiers in behavioral neuroscience. 2023:17():1008086. doi: 10.3389/fnbeh.2023.1008086. Epub 2023 Mar 21 [PubMed PMID: 37025109]
Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. International journal of yoga. 2011 Jul:4(2):49-54. doi: 10.4103/0973-6131.85485. Epub [PubMed PMID: 22022122]
Level 2 (mid-level) evidenceMa X, Yue ZQ, Gong ZQ, Zhang H, Duan NY, Shi YT, Wei GX, Li YF. The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Frontiers in psychology. 2017:8():874. doi: 10.3389/fpsyg.2017.00874. Epub 2017 Jun 6 [PubMed PMID: 28626434]
Baklouti S, Aloui A, Baklouti H, Souissi N, Jarraya M. Effects of Hatha yoga on cognitive functions in the elderly: a cross-sectional study. The Libyan journal of medicine. 2022 Dec:17(1):2080799. doi: 10.1080/19932820.2022.2080799. Epub [PubMed PMID: 35657065]
Level 2 (mid-level) evidenceBaklouti S, Fekih-Romdhane F, Guelmami N, Bonsaksen T, Baklouti H, Aloui A, Masmoudi L, Souissi N, Jarraya M. The effect of web-based Hatha yoga on psychological distress and sleep quality in older adults: A randomized controlled trial. Complementary therapies in clinical practice. 2023 Feb:50():101715. doi: 10.1016/j.ctcp.2022.101715. Epub 2022 Dec 13 [PubMed PMID: 36521407]
Level 1 (high-level) evidenceHoge EA, Bui E, Mete M, Dutton MA, Baker AW, Simon NM. Mindfulness-Based Stress Reduction vs Escitalopram for the Treatment of Adults With Anxiety Disorders: A Randomized Clinical Trial. JAMA psychiatry. 2023 Jan 1:80(1):13-21. doi: 10.1001/jamapsychiatry.2022.3679. Epub [PubMed PMID: 36350591]
Level 1 (high-level) evidenceLenze EJ, Mantella RC, Shi P, Goate AM, Nowotny P, Butters MA, Andreescu C, Thompson PA, Rollman BL. Elevated cortisol in older adults with generalized anxiety disorder is reduced by treatment: a placebo-controlled evaluation of escitalopram. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2011 May:19(5):482-90. doi: 10.1097/JGP.0b013e3181ec806c. Epub [PubMed PMID: 20808146]
Level 1 (high-level) evidenceGoldin P, Ramel W, Gross J. Mindfulness Meditation Training and Self-Referential Processing in Social Anxiety Disorder: Behavioral and Neural Effects. Journal of cognitive psychotherapy. 2009 Aug:23(3):242-257 [PubMed PMID: 25568592]
Winter SE, Barber JP. Should treatment for depression be based more on patient preference? Patient preference and adherence. 2013:7():1047-57. doi: 10.2147/PPA.S52746. Epub 2013 Oct 9 [PubMed PMID: 24143080]
Klainin-Yobas P, Cho MA, Creedy D. Efficacy of mindfulness-based interventions on depressive symptoms among people with mental disorders: a meta-analysis. International journal of nursing studies. 2012 Jan:49(1):109-21. doi: 10.1016/j.ijnurstu.2011.08.014. Epub 2011 Sep 29 [PubMed PMID: 21963234]
Level 1 (high-level) evidenceKuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, Barrett B, Byng R, Evans A, Mullan E, Teasdale JD. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of consulting and clinical psychology. 2008 Dec:76(6):966-78. doi: 10.1037/a0013786. Epub [PubMed PMID: 19045965]
Level 1 (high-level) evidenceSpeca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosomatic medicine. 2000 Sep-Oct:62(5):613-22 [PubMed PMID: 11020090]
Level 1 (high-level) evidenceGarland SN, Carlson LE, Cook S, Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2007 Aug:15(8):949-61 [PubMed PMID: 17611782]
Level 1 (high-level) evidenceSharma M, Rush SE. Mindfulness-based stress reduction as a stress management intervention for healthy individuals: a systematic review. Journal of evidence-based complementary & alternative medicine. 2014 Oct:19(4):271-86. doi: 10.1177/2156587214543143. Epub 2014 Jul 22 [PubMed PMID: 25053754]
Level 1 (high-level) evidenceGreeson JM, Smoski MJ, Suarez EC, Brantley JG, Ekblad AG, Lynch TR, Wolever RQ. Decreased symptoms of depression after mindfulness-based stress reduction: potential moderating effects of religiosity, spirituality, trait mindfulness, sex, and age. Journal of alternative and complementary medicine (New York, N.Y.). 2015 Mar:21(3):166-74. doi: 10.1089/acm.2014.0285. Epub 2015 Feb 19 [PubMed PMID: 25695903]
Cuijpers P, van Straten A, Hollon SD, Andersson G. The contribution of active medication to combined treatments of psychotherapy and pharmacotherapy for adult depression: a meta-analysis. Acta psychiatrica Scandinavica. 2010 Jun:121(6):415-23. doi: 10.1111/j.1600-0447.2009.01513.x. Epub 2009 Nov 18 [PubMed PMID: 19922522]
Level 1 (high-level) evidenceBergen-Cico D, Possemato K, Cheon S. Examining the efficacy of a brief mindfulness-based stress reduction (Brief MBSR) program on psychological health. Journal of American college health : J of ACH. 2013:61(6):348-60. doi: 10.1080/07448481.2013.813853. Epub [PubMed PMID: 23930749]
Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. Journal of alternative and complementary medicine (New York, N.Y.). 2009 May:15(5):593-600. doi: 10.1089/acm.2008.0495. Epub [PubMed PMID: 19432513]
Level 1 (high-level) evidenceCarmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of behavioral medicine. 2008 Feb:31(1):23-33 [PubMed PMID: 17899351]
Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. Journal of psychosomatic research. 2008 Apr:64(4):393-403. doi: 10.1016/j.jpsychores.2007.06.015. Epub 2008 Mar 4 [PubMed PMID: 18374738]
Martín-Asuero A, García-Banda G. The Mindfulness-based Stress Reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. The Spanish journal of psychology. 2010 Nov:13(2):897-905 [PubMed PMID: 20977037]
Flook L, Goldberg SB, Pinger L, Bonus K, Davidson RJ. Mindfulness for teachers: A pilot study to assess effects on stress, burnout and teaching efficacy. Mind, brain and education : the official journal of the International Mind, Brain, and Education Society. 2013 Sep:7(3):. doi: 10.1111/mbe.12026. Epub [PubMed PMID: 24324528]
Level 3 (low-level) evidenceMorone NE. Not Just Mind Over Matter: Reviewing With Patients How Mindfulness Relieves Chronic Low Back Pain. Journal of evidence-based integrative medicine. 2019 Jan-Dec:24():2515690X19838490. doi: 10.1177/2515690X19838490. Epub [PubMed PMID: 30942087]
Zgierska AE, Burzinski CA, Cox J, Kloke J, Stegner A, Cook DB, Singles J, Mirgain S, Coe CL, Bačkonja M. Mindfulness Meditation and Cognitive Behavioral Therapy Intervention Reduces Pain Severity and Sensitivity in Opioid-Treated Chronic Low Back Pain: Pilot Findings from a Randomized Controlled Trial. Pain medicine (Malden, Mass.). 2016 Oct:17(10):1865-1881 [PubMed PMID: 26968850]
Level 1 (high-level) evidenceKabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General hospital psychiatry. 1982 Apr:4(1):33-47 [PubMed PMID: 7042457]
Morone NE, Greco CM, Moore CG, Rollman BL, Lane B, Morrow LA, Glynn NW, Weiner DK. A Mind-Body Program for Older Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA internal medicine. 2016 Mar:176(3):329-37. doi: 10.1001/jamainternmed.2015.8033. Epub [PubMed PMID: 26903081]
Level 1 (high-level) evidenceCherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, Hansen KE, Turner JA. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA. 2016 Mar 22-29:315(12):1240-9. doi: 10.1001/jama.2016.2323. Epub [PubMed PMID: 27002445]
Level 1 (high-level) evidenceMarske C, Shah S, Chavira A, Hedberg C, Fullmer R, Clark CJ, Pipitone O, Kaiser P. Mindfulness-Based Stress Reduction in the Management of Chronic Pain and Its Comorbid Depression. The Journal of the American Osteopathic Association. 2020 Sep 1:120(9):575-581. doi: 10.7556/jaoa.2020.096. Epub [PubMed PMID: 32854117]
Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U. Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and psychosomatics. 2007:76(4):226-33 [PubMed PMID: 17570961]
Epstein RM. Mindful practice. JAMA. 1999 Sep 1:282(9):833-9 [PubMed PMID: 10478689]
Zimmaro LA, Moss A, Reibel DK, Handorf EA, Reese JB, Fang CY. A Telephone-Adapted Mindfulness-Based Stress Reduction Program: Preliminary Effects among Healthcare Employees. Behavioral sciences (Basel, Switzerland). 2021 Oct 18:11(10):. doi: 10.3390/bs11100139. Epub 2021 Oct 18 [PubMed PMID: 34677232]
Shurney D. Employing Mindfulness in Lifestyle Medicine. American journal of lifestyle medicine. 2019 Nov-Dec:13(6):561-564. doi: 10.1177/1559827619867625. Epub 2019 Aug 8 [PubMed PMID: 31662722]