Introduction
Diving in open waters is popular. It is enjoyed by novices and professionals alike. Many people dive for recreation, competitive sport, commercial employment, and military training. Diving as a profession can be dated back to more than 5000 years, yet diving-related diseases were not described until Paul Bert wrote about caisson disease in 1878. Symptoms of caisson disease were observed among bridge workers after finishing their shifts underwater and coming back to the surface. These symptoms included dizzy spells, difficulty breathing, and sharp pain in the abdomen or joints. The caisson workers often said that they felt well while working. This was due to their being rested at the start of the shift compared to being exhausted when the workday was through. The workers would often have intense back pain that left them bent over, which is how caisson disease earned the nickname "the bends."
Pulmonary barotrauma is a potential diving injury. Pulmonary barotrauma can occur during self-contained underwater breathing apparatus (SCUBA) diving or free diving. It can happen during descent (negative pulmonary barotrauma or lung squeeze) or during ascent (positive pulmonary barotrauma is also known as pulmonary overinflation syndrome (POIS).[1] Pulmonary barotrauma most often occurs during ascent and is due to lung overexpansion when a SCUBA diver returns to the surface without exhaling or when the air becomes trapped in the lung.[2] Barotrauma is an injury inflicted by a difference in pressure between a gas inside or outside the body and the pressure of the surrounding gas or fluid. Damage occurs due to over tension or shear forces from the expansion of the gas within or by pressure hydrostatically transmitted through the tissues. Complications include local infiltration of gas into the damaged tissue or local circulation interfering with organ function or resulting in circulatory compromise.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
According to Boyle’s law, which states that at a constant temperature, a volume of a gas varies inversely with the pressure to which it is subjected, P1V1= P2V2.[3] Plainly stated, as pressure increases on the descent, the volume must decrease, and as pressure falls on the ascent, the volume must increase. At sea level (0 meters, 0 ft), the air pressure exerts a force of 14.7 lbs/in or 1 atmosphere absolute (1 ATA). For every 10 meters (32.8 ft) of depth into the sea, the water pressure will increase by 1 ATA. At 10 meters (32.8 ft), water pressure will be 2 ATA, and air pressure will exert a force of 29.4 lbs/in, causing a decrease in lung capacity by 50%. At 20 meters (65.6 ft), water pressure will be 3 ATA, and air pressure will exert a force of 44.1 lbs/in, causing a decrease in lung capacity by 67%. At 30 meters (98.4 ft), water pressure will be 4 ATA, and air pressure will exert a force of 58.8 lbs/in, causing a decrease in lung capacity by 75%. At 40 meters (131.2 ft), water pressure will be 5 ATA, and air pressure will exert a force of 73.5 lbs/in, causing a decrease in lung capacity by 80%. The lungs are most adversely affected by declines in lung capacity in the first 10 meters (32.8 ft) with a 50% reduction.[4] Pulmonary barotrauma occurs when the pressures in a person’s lungs are unequal to the ambient environmental pressures, going beyond the limits of the lungs.
Transpulmonary pressures of more than 60 to 70 mmHg can cause an alveolar rupture.[5] For example, if a SCUBA diver has a lung volume of 6L at the surface and descends to 10 meters, then the lung volume is reduced to 3L. If the SCUBA diver breathes compressed air at this depth at their lung capacity of 6L and then comes to the surface without exhaling, the volume of gas in the lungs will expand by 50% or 12L, which will cause the individual’s lungs to rupture. It is easy to understand that pulmonary barotrauma can occur even at small or shallower depths depending upon the person’s lung capacity, diving experience, equipment, and training. Many diving injuries and fatalities occur in novice and inexperienced divers, particularly in the first two years of diving.[1]
According to Henry's law, the solubility of a gas in a liquid is directly proportional to the pressure exerted on the gas and liquid. Thus when the cap of a soda pop bottle is removed, soda begins to bubble as gas is released from the liquid. As such, when nitrogen in a diver’s tank dissolves in the diver’s fatty tissues or synovial fluid at depth, nitrogen will move out from those tissues as the diver ascends to the surface (a lower pressure environment). This happens slowly and gradually if the diver ascends progressively and slowly, and the nitrogen from the bloodstream enters the lungs and is exhaled out. However, if the diver ascends rapidly, nitrogen exits tissues quickly and forms bubbles. When bubbles are formed, they can affect tissues in many ways. They can constrict blood vessels causing ischemic injury. This can be deleterious when occurring in critical areas in the brain. The bubbles can also form a surface to which proteins in the bloodstream can cling, unravel, and begin a clotting or inflammatory cascade. This cascade can lead to endothelial breakdown and permanent tissue damage.
Epidemiology
There are 9 million divers worldwide, with three million located in the United States. The median age is 30 years old, and 60% are male, while 40% are female.[6] A review of the Divers Alert Network fatality data shows that barotrauma is the most reported injury related to diving. Approximately 80% of the injuries are related to ear and sinus barotrauma; 15% are due to pulmonary barotrauma, including arterial gas embolism. The remaining 5% of damage is due to gastrointestinal, dental, mask, or suit squeeze barotrauma. The majority of diving fatalities are due to drowning, atherosclerotic heart disease, and pulmonary barotrauma-related arterial gas embolism. Many have called for specialized autopsy and reporting procedures to understand the incidence of this injury better.[7]
Pathophysiology
The alveoli are the smallest lung units where oxygen and carbon dioxide exchange take place. Under decreasing pressure and expanding volume, the alveoli will rupture along with their surrounding blood vessels. The alveoli will be flooded with blood and debris and will collapse. Alveoli are located centrally and peripherally. Depending on the location of the ruptured collapsed alveoli, air will leak out. Generally, air travels to five areas in the body.[4] It can move centrally to the mediastinum, causing pneumomediastinum, pneumopericardium, and then towards the head and neck, manifesting as subcutaneous emphysema, or track along the esophagus and cause pneumoperitoneum. It can travel peripherally to the pleural spaces causing pneumothorax or tension pneumothorax. Alveolar air can enter the capillary vessels, pulmonary veins, and central circulation, forming air gas embolism, a severe life-threatening event.[8]
History and Physical
Physical signs and symptoms of pulmonary barotrauma related to SCUBA diving can be subtle with pneumomediastinum or subcutaneous emphysema.[9] However, more severe pulmonary barotrauma associated with SCUBA diving with pneumothorax, tension pneumothorax, or cerebral air-gas embolism symptoms are immediate upon surfacing or within ten minutes.[10] Overall symptoms include cough, shortness of breath, hemoptysis, chest pain, dyspnea, choking, change in voice, hoarseness, difficulty swallowing, cyanosis, respiratory failure, loss of consciousness, cardiac arrest, and death.[4] Pneumomediastinum can be symptomless, or patients can experience chest discomfort, substernal chest pain, cough, shortness of breath, change in voice, hoarseness, and difficulty swallowing. Hamman’s sign is a crunching, crackling sound auscultated over the precordium with the heartbeat in the presence of pneumomediastinum.[4] Pneumopericardium can cause chest pain, shoulder or back pain, rapid heart rate, and arrhythmias.[4]
Subcutaneous emphysema in the cervical region can lead to voice changes, difficulty swallowing, choking, or foreign body sensation. Crepitus or a crackling sensation can be felt under the skin as air travels through the subcutaneous tissues. Air can track down the esophagus and cause pneumoperitoneum.[4] Pneumothorax is much less common than pneumomediastinum due to the increased resistance while air travels between the visceral and parietal pleura.[4] However, the rupture of the alveoli at the pleural surface will lead to pneumothorax and lung collapse. Tension pneumothorax will develop as more pressure is exerted on the heart and great vessels blood flow leading to circulatory failure, cardiac arrest, and death. Pneumothorax causes chest pain after rupture along with shortness of breath, rapid shallow breathing, chest asymmetry, tachycardia, and tympanic chest sounds on the side of rupture.[4]
Air emboli are formed when air is forced into the capillaries, pulmonary veins, and central circulation. These bubbles collect in the heart or brain and obstruct blood flow. The damaged epithelial and endothelial cells release inflammatory mediators. This damage to the cells leads to leaky vessels causing swelling and edema. In the brain, this manifests as cerebral edema. The initial presentation of arterial gas embolism is the loss of consciousness, seizure, and cardiac arrest due to lack of blood flow in the large vessels or air gas emboli in the brainstem.[8] Air-gas emboli can also cause headaches, confusion, numbness, tingling, paresthesia, fatigue, hemiplegia, paralysis, aphasia, or any stroke symptom.[4] Air-gas emboli can also reach the coronary arteries and present as an acute myocardial infarction with chest pain, chest pressure, pain radiating to the neck, shoulders, back, or jaw.[4] Shock and cardiac arrest can ensue. Patients with patent foramen ovale are at higher risk of gas bubbles passing from right to left shunt and causing CNS injuries.[11][12]
An inquiry should be made regarding previous decompression injuries, pulmonary blobs, Marfan syndrome, asthma, chronic obstructive pulmonary disease (COPD), pregnancy, and any prior pulmonary injuries or surgeries.[13]
Evaluation
A diver with suspected pulmonary barotrauma needs prompt medical evaluation and treatment. Upon arrival at the medical facility, a history, physical exam, basic labs, electrocardiogram (EKG), and chest roentgenogram are required.
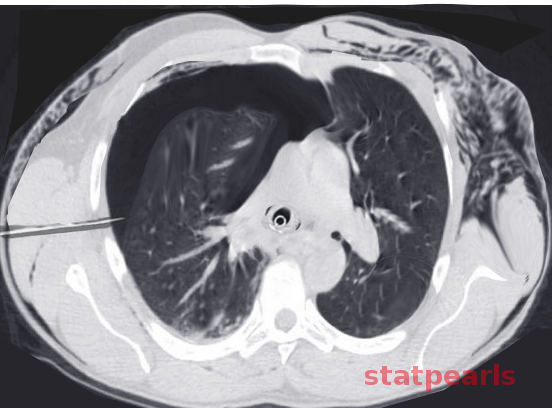
Chest radiograph most commonly will reveal pneumomediastinum, but pneumothorax can be present. Edema or infiltrates may also be present.[14] Any patient who has a severe headache or severe back pain after a dive, subcutaneous emphysema, changes in the level of consciousness, dyspnea, or unexplained chest pain is a potential candidate for a computed tomography (CT) scan or magnetic resonance imaging (MRI).[15] Spiral CT is most sensitive to evaluate for pneumothorax.[16] It should be performed in all patients with barotrauma suspected of having pneumothorax, but chest radiograph is normal. CT done within six hours can show air in both arterial and venous systems. This information has prognostic and pathological significance.[17] Ultrasonography and echocardiography can be used to detect the number and size of bubbles in the right side of the heart, gas in subcutaneous tissue, the presence of an abscess in swelling of the face and neck, and air in the peritoneum.[18]
A complete blood count can help determine if an infection is present, and if hematocrit is more than 48%, the chance of neurologic sequelae one month after the injury is high. Rising serum creatinine phosphokinase (CPK) indicates tissue damage due to microemboli. EKG can reveal tachycardia, arrhythmias, or myocardial infarction. Pulse oximetry or arterial blood gas can indicate hypoxia. Then, the need for recompression and hyperbaric oxygen therapy needs to be efficiently and accurately assessed for the patient.
Treatment / Management
The diver should be stabilized with basic and advanced cardiac life support. Intravenous access should be obtained along with the application of supplemental oxygen. Administration of crystalloid intravenous fluid for hydration is recommended. Perform intubation in patients who have an unstable airway or have persistent hypoxia despite breathing 100% oxygen.
No specific treatment is required for mild cases of pneumomediastinum as air will reabsorb on its own.[4] Supplemental oxygen can be initiated for persons experiencing hypoxia. Higher concentrations of oxygen increase the reabsorption rate of the air.[4] Pneumothorax may resolve without treatment or require chest tube thoracostomy. Tension pneumothorax mandates chest tube thoracostomy to drain air and reduce pressure to allow blood flow and circulatory function.
Treatment for arterial gas embolism related to pulmonary barotrauma should ideally be completed within the first two hours. This provides the most benefit and best chance of complete resolution of symptoms. Any delays in recompression and hyperbaric oxygen therapy (HBOT) of more than six hours are associated with worse outcomes.[19] Recompression therapy should be done at a dive chamber by medical personnel certified in hyperbaric medicine. Indications for recompression therapy include spinal cord injury and neurologic impairment. Patients who are seriously ill and do not respond to initial treatment may need higher pressure decompression at 4 to 5 atmospheres of absolute pressure and may need breathing gas of 50% helium/50% oxygen mixture (heliox). Although research has been done on the use of surfactants being given before deep dives, it is still in the research stage of development.[20](B3)
Differential Diagnosis
The differential diagnosis of pulmonary barotrauma related to SCUBA diving includes:
- Drowning
- Near drowning
- Myocardial infarction
- Pulmonary embolism
- Cerebral vascular accident
- Carotid artery dissection
- Immersion pulmonary edema
- Asthma exacerbation
- Laryngospasm
- Marine envenomation
- Contaminated gas toxicities
Prognosis
The prognosis for pulmonary barotrauma related to SCUBA diving depends on the severity of and type of pulmonary barotrauma suffered. Mild cases of pneumomediastinum or pneumothorax resolve with little or no treatment. Complete resolution occurs in most cases.[4] Large pneumothorax or tension pneumothorax requires chest tube drainage of air, but the healing should resolve without further sequelae. Air-gas embolism from pulmonary barotrauma, unfortunately, carries a 30% rate of mortality. It is the second most common cause of death in divers after drowning.[8]
Complications
Complications of pulmonary barotrauma due to lung overexpansion while surfacing from SCUBA diving include pneumomediastinum, pneumopericardium, pneumoperitoneum, subcutaneous emphysema, pneumothorax, tension pneumothorax, and air gas embolism. Cerebral air gas embolism is the most devastating and feared complication.[4] Lung infiltrates are common on initial chest radiographs and CT scans of the chest of patients suffering from pulmonary barotrauma.[14]
Aspiration pneumonitis, pneumonia, pleural effusions, empyema, pyopneumothorax, scarring, fibrosis, and decreased lung function have been documented in patients after pulmonary barotrauma injuries.[1] Air-gas embolism is a medical emergency. Incorrect diagnosis and delayed treatment can have a catastrophic neurologic injury with irreversible damage to the brain and spinal cord.[4] Fortunately, most patients with pulmonary barotrauma have minor injuries and presentations and recover with little to no deficits.
Deterrence and Patient Education
Divers with preexisting or prior lung disease are at increased risk of pulmonary barotrauma while diving.[2][21] Any person with current or preexisting lung disease should be medically screened before diving. Individuals with asthma (controlled or uncontrolled), obstructive lung disease, emphysema, bullae, cysts or cystic lung disease, fibrosis, tuberculosis (active or past), sarcoidosis, and spontaneous pneumothorax history are at increased risk for pulmonary barotrauma during diving. Many diving injuries and fatalities are avoidable.
Following a pre-diving checklist, assessing equipment for proper functioning before each dive, and adhering to safe diving practices with appropriate education and training is paramount to saving lives and preventing future injury.[1] Divers should be warned against multiple daily dives, diving, and flying on the same day, and trying to alter their dive profile.[22] Recent studies have shown that aerobic exercises before a dive or during decompression stop may decrease the post-dive gas bubble formation.[23][24]
Enhancing Healthcare Team Outcomes
More and more individuals from all age groups are learning and continuing to dive. Barotrauma is the most commonly reported diving-related injury, with arterial gas embolism-related pulmonary barotrauma being the second most common diving-related cause of death. Divers that suffer any form of pulmonary barotrauma need to be medically evaluated before returning to diving. Health care providers need to be aware of the recommendations for fitness to dive.[4] Air-gas emboli related to pulmonary barotrauma can be a severe life-threatening event. An interprofessional team including EMS providers, emergency clinicians, nurses, and hyperbaric medicine clinicians must recognize these dangers quickly to diagnose and treat for improved patient outcomes. [Level 5] Patients with asthma with a mild and well-controlled condition may be permitted to dive under restricted circumstances.[25]
Media
References
Buzzacott P, Denoble PJ. DAN Annual Diving Report 2018 Edition: A Report on 2016 Diving Fatalities, Injuries, and Incidents. 2018:(): [PubMed PMID: 31021587]
Russi EW. Diving and the risk of barotrauma. Thorax. 1998 Aug:53 Suppl 2(Suppl 2):S20-4 [PubMed PMID: 10193343]
Melamed Y, Shupak A, Bitterman H. Medical problems associated with underwater diving. The New England journal of medicine. 1992 Jan 2:326(1):30-5 [PubMed PMID: 1727063]
Bove AA. Diving medicine. American journal of respiratory and critical care medicine. 2014 Jun 15:189(12):1479-86. doi: 10.1164/rccm.201309-1662CI. Epub [PubMed PMID: 24869752]
SCHAFFER KE, McNULTY WP Jr, CAREY C, LIEBOW AA. Mechanisms in development of interstitial emphysema and air embolism on decompression from depth. Journal of applied physiology. 1958 Jul:13(1):15-29 [PubMed PMID: 13563337]
Penrice D, Cooper JS. Diving Casualties. StatPearls. 2025 Jan:(): [PubMed PMID: 29083771]
Casadesús JM, Aguirre F, Carrera A, Boadas-Vaello P, Serrando MT, Reina F. Diagnosis of arterial gas embolism in SCUBA diving: modification suggestion of autopsy techniques and experience in eight cases. Forensic science, medicine, and pathology. 2018 Mar:14(1):18-25. doi: 10.1007/s12024-018-9951-4. Epub 2018 Feb 19 [PubMed PMID: 29460254]
Level 3 (low-level) evidenceNeuman TS, Jacoby I, Bove AA. Fatal pulmonary barotrauma due to obstruction of the central circulation with air. The Journal of emergency medicine. 1998 May-Jun:16(3):413-7 [PubMed PMID: 9610969]
Level 3 (low-level) evidenceRaymond LW. Pulmonary barotrauma and related events in divers. Chest. 1995 Jun:107(6):1648-52 [PubMed PMID: 7781361]
Level 3 (low-level) evidenceBattisti AS, Haftel A, Murphy-Lavoie HM. Barotrauma. StatPearls. 2025 Jan:(): [PubMed PMID: 29493973]
Bove AA. Risk of decompression sickness with patent foramen ovale. Undersea & hyperbaric medicine : journal of the Undersea and Hyperbaric Medical Society, Inc. 1998 Fall:25(3):175-8 [PubMed PMID: 9789338]
Level 1 (high-level) evidenceGermonpré P, Dendale P, Unger P, Balestra C. Patent foramen ovale and decompression sickness in sports divers. Journal of applied physiology (Bethesda, Md. : 1985). 1998 May:84(5):1622-6 [PubMed PMID: 9572808]
Level 2 (mid-level) evidenceCamporesi EM. Diving and pregnancy. Seminars in perinatology. 1996 Aug:20(4):292-302 [PubMed PMID: 8888455]
Level 3 (low-level) evidenceHarker CP, Neuman TS, Olson LK, Jacoby I, Santos A. The roentgenographic findings associated with air embolism in sport scuba divers. The Journal of emergency medicine. 1993 Jul-Aug:11(4):443-9 [PubMed PMID: 8228108]
Level 2 (mid-level) evidenceSegev Y, Landsberg R, Fliss DM. MR imaging appearance of frontal sinus barotrauma. AJNR. American journal of neuroradiology. 2003 Mar:24(3):346-7 [PubMed PMID: 12637280]
Level 3 (low-level) evidenceReuter M, Tetzlaff K, Warninghoff V, Steffens JC, Bettinghausen E, Heller M. Computed tomography of the chest in diving-related pulmonary barotrauma. The British journal of radiology. 1997 May:70(833):440-5 [PubMed PMID: 9227223]
Level 3 (low-level) evidenceLaurent PE, Coulange M, Bartoli C, Boussuges A, Rostain JC, Luciano M, Cohen F, Rolland PH, Mancini J, Piercecchi MD, Vidal V, Gorincour G. Appearance of gas collections after scuba diving death: a computed tomography study in a porcine model. International journal of legal medicine. 2013 Jan:127(1):177-84. doi: 10.1007/s00414-011-0662-6. Epub 2011 Dec 30 [PubMed PMID: 22207142]
Level 3 (low-level) evidencePayne SJ, Chappell MA. Automated determination of bubble grades from Doppler ultrasound recordings. Aviation, space, and environmental medicine. 2005 Aug:76(8):771-7 [PubMed PMID: 16110694]
Walker, III JR, Hexdall EJ, Murphy-Lavoie HM. Diving Gas Embolism. StatPearls. 2025 Jan:(): [PubMed PMID: 29493946]
Eckmann DM, Zhang J, Lampe J, Ayyaswamy PS. Gas embolism and surfactant-based intervention: implications for long-duration space-based activity. Annals of the New York Academy of Sciences. 2006 Sep:1077():256-69 [PubMed PMID: 17124129]
Level 3 (low-level) evidenceTetzlaff K, Reuter M, Leplow B, Heller M, Bettinghausen E. Risk factors for pulmonary barotrauma in divers. Chest. 1997 Sep:112(3):654-9 [PubMed PMID: 9315797]
Level 2 (mid-level) evidenceSheffield PJ. Flying after diving guidelines: a review. Aviation, space, and environmental medicine. 1990 Dec:61(12):1130-8 [PubMed PMID: 2285403]
Blatteau JE, Gempp E, Galland FM, Pontier JM, Sainty JM, Robinet C. Aerobic exercise 2 hours before a dive to 30 msw decreases bubble formation after decompression. Aviation, space, and environmental medicine. 2005 Jul:76(7):666-9 [PubMed PMID: 16018350]
Dujić Z, Palada I, Obad A, Duplancić D, Baković D, Valic Z. Exercise during a 3-min decompression stop reduces postdive venous gas bubbles. Medicine and science in sports and exercise. 2005 Aug:37(8):1319-23 [PubMed PMID: 16118578]
Adir Y, Bove AA. Can asthmatic subjects dive? European respiratory review : an official journal of the European Respiratory Society. 2016 Jun:25(140):214-20. doi: 10.1183/16000617.0006-2016. Epub [PubMed PMID: 27246598]