Introduction
The vagina is a female reproductive organ that changes over the lifespan of a woman. It serves a multitude of functions in response to hormonal changes as appreciated during puberty, menstruation, pregnancy, and menopause. The vagina plays a vital role in the female reproductive system and female sexual pleasure.
Anatomic Overview
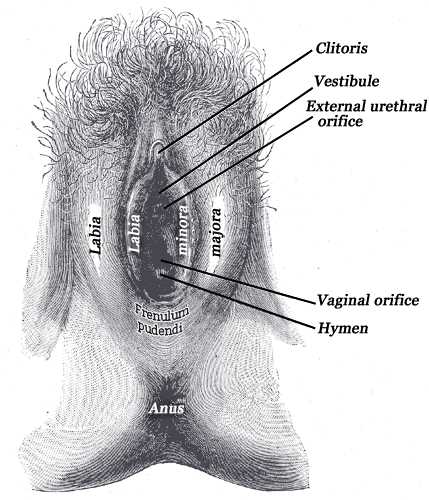
The vagina is an elastic muscular tube of 7 to 10 cm in length that extends from the vulva (female external genitalia) to the cervix of the uterus where it ends in an anterior and posterior fornix. The vaginal canal is positioned between the urethra and bladder anteriorly, and the rectum posteriorly. The vaginal opening is in the posterior portion of the vulvar vestibule, behind the urethral opening. It is surrounded on either side by the labia minora medially and labia majora laterally. A thin perforated layer of hymen partially forms the entrance of the vaginal opening. The vaginal canal has an outer fibrous adventitia, a middle layer of smooth muscle cells, and an inner layer of mucosa. The inner mucosal membrane has transverse folds called rugae, which can be appreciated grossly.[1][2]
Cellular Level
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Cellular Level
The vaginal walls are composed of multi-layered stratified squamous epithelial cells which contain cytokeratin.[3] This epithelial layer consists of an actively dividing stratum basale, suprabasal layer, and stratum corneum.[4] Mullerian derived columnar cells begin to migrate caudally into the endocervical canal leaving behind a squamous epithelial lining.[5] This process is alluded to in patients exposed to diethylstilbestrol (DES) where maturation halts and columnar cells persist in the vaginal canal.[5] The vagina does not contain any glands, rather, fluid transudates through the vaginal wall.[1] The cells of the vagina are responsive to the hormone estrogen and contain receptors for this hormone, which produces a response that is crucial in the maintenance of the vaginal walls.[1]
Development
The vagina has embryologic derivatives from both the Mullerian ducts proximally and urogenital sinus distally.[2] The physiology of the vagina changes drastically over the lifetime of a woman as a response to changes in hormones. At birth, the vagina is heavily estrogenized from maternal hormones, and this causes the vagina to be acidic with a predominance of lactobacilli. The walls contain a high proportion of glycogen during this period. When these hormone levels drop off approximately four weeks postnatal, the physiology of the vagina will change to a pre-pubertal stage with a neutral to the alkaline environment associated with fewer acid-producing bacteria. As the female develops, the vagina will take on mature characteristics due to adrenal and gonadal maturation. During reproductive years, lactic-acid producing bacteria predominate once more. As women enter the premenopausal period and eventually menopause, the vaginal tissue atrophies secondary to ovarian quiescence and concomitant low estrogen levels. Colonization with enteric flora may increase at this time.[3]
Organ Systems Involved
The vagina is a reproductive organ which connects the vulva to the cervix of the uterus and ultimately to the uterine cavity. Sexual arousal, with a strong psychologic and neurologic component, is also closely related to the process of lubrication.[3][6]
Function
The vagina has multiple functions, including[4][6][4]:
- Menstruation- as a canal for menstrual fluid and tissue to leave the uterine cavity
- Immune defense- protection against harmful pathogens via acidic pH, local flora, and chemical signaling
- Reproduction functions- as the receptacle for sperm and canal for parturition
- Sexual functions - for female arousal response and sexual pleasure
Mechanism
While the vagina does not contain glands, fluid transudates through the vaginal walls to create lubrication. The fluid is leaked from the capillaries due to vasocongestion into the space between vaginal epithelial cells and ultimately into the lumen.[7] This process is heavily dependent on the actions of nitric oxide (NO) in the endothelium, which gets released in response to sexual arousal due to stimulation of parasympathetic nitrergic nerves.[7] NO induces vasodilation through the cGMP cascade and decreased phosphodiesterase enzyme leading to smooth muscle relaxation. Major components of the vaginal secretions include water, desquamating epithelial cells, cervical mucus, fluids from the upper genital tract, and leukocytes. Estrogens and sexual stimulation are examples of factors which increase vaginal fluid. Estrogen enhances NO synthase function.[8] Major organic constituents of vaginal fluid are proteins, carbohydrates, and fatty acids.[9][10][11]
Related Testing
Vaginal pH testing, wet prep, potassium hydroxide preparation, and culture are frequently performed during a pelvic examination to help elucidate the cause of vaginitis.[12] A biopsy may be necessary at this location if a lesion is visible on speculum examination or clinical suspicion for malignancy.
Pathophysiology
Changes in the bacterial flora and vaginal pH are closely related to vaginitis. The normal vaginal pH is from 3.8 to 4.5. This pH is secondary to acid-producing bacteria and helps to maintain the local flora, kill sperm, and produce immunologic protection against bacterial overgrowth.[12]
Candida is a naturally occurring organism that can proliferate and result in an overgrowth and yeast infection. Elevated blood sugars and COC pills increase the risk of yeast infection.[12][13]
The sexually transmitted parasites such trichomonas is acquired through sexual contact with an infected partner. This organism can be transmitted back and forth between partners unless both partners receive adequate treatment.[14]
HPV infection is sexually transmitted and highly associated with vaginal squamous cell carcinoma and related premalignant lesions, which occurs via proteins E6 and E7 interrupting proper DNA checkpoints leading to DNA mutations and nuclear changes. This situation can lead to dysplasia and eventual malignant neoplasia of the tissue.[15][16]
Clinical Significance
Vaginitis - Inflammation of the vagina can result from the overgrowth of local bacteria, yeast, or sexually transmitted infection. Bacterial Vaginosis (BV) characteristically presents with an alkaline pH and predominance of Gardnerella and Mycoplasma spp. BV is often associated with a ‘fish-like’ odor. Vaginal candidiasis is an overgrowth of a commensal organism and is another cause of vaginitis characterized by pruritus, thick ‘cottage cheese-like’ discharge and changes in vaginal flora. Trichomoniasis is a sexually transmitted disease caused by a parasite that is commonly associated with a clinical picture of yellow-green frothy discharge and vaginal irritation. Non-infectious vaginitis can be due to allergic reactions or irritation secondary to applying products to the vagina such as douches, scented perfumes, and soaps.[12][17]
Vaginal neoplasia - Vaginal intraepithelial neoplasia (VAIN) precursor lesions are associated with HPV and may progress to malignant vaginal squamous cell carcinoma; this is the most common form of vaginal malignancy. Vaginal clear cell carcinoma is associated with DES exposure in utero due, in part, by the persistence of columnar cells. Several more rare neoplasms, both malignant and benign can occur in the vagina.[15][16][18]
- Benign vaginal lesions: angiomyofibroblastoma, fibroepithelial polyp, hymenal polyp, leiomyoma, Mullerian papilloma, polyposis, vaginalis postoperative spindle cell nodule, pseudosarcomatous fibroepithelial stromal polyp, rhabdomyoma, spindle cell epithelioma, squamous papilloma, superficial cervicovaginal myofibroblastoma, tubulovillous adenoma
- Malignant vaginal lesions: adenocarcinoma, aggressive angiomyxoma, clear cell adenocarcinoma, endometrioid adenocarcinoma, granulocytic sarcoma leiomyosarcoma, lymphoma, malignant mixed tumor melanoma, mesonephric adenocarcinoma, metastases, mucinous adenocarcinoma, myeloid sarcoma, rhabdomyosarcoma, small cell carcinoma, spindle cell carcinoma, squamous cell carcinoma, urothelial carcinoma, VAIN, verrucous carcinoma, yolk sac tumor
Vaginal trauma - Causes range from vaginal intercourse to parturition and iatrogenically from instrumentation. Tears can range in severity from mucosal involvement to underlying muscle involvement.[19] A rare postoperative complication is vaginal evisceration.[20]
Vaginal atrophy - Declining levels of estrogen during peri-menopausal and menopausal years are associated with thinning of the vaginal walls and loss of rugae.[21] This atrophy can cause pain, bleeding from micro-tears, and painful intercourse also called dyspareunia.[22][23]
Vaginal prolapse - Vaginal vault prolapse occurs with weakened vaginal walls, fascia, and ligaments that are supporting the surrounding structures such as uterus, rectum, bowel, and bladder. These may prolapse out of the vaginal canal and present as a bulge, sensation of increased pressure and a spectrum of changes in bowel and urinary continence.[24][25]
Media
(Click Image to Enlarge)
References
KRANTZ KE. The gross and microscopic anatomy of the human vagina. Annals of the New York Academy of Sciences. 1959 Nov 18:83():89-104 [PubMed PMID: 14411705]
WELLS LJ. Embryology and anatomy of the vagina. Annals of the New York Academy of Sciences. 1959 Nov 18:83():80-8 [PubMed PMID: 13843905]
Paavonen J. Physiology and ecology of the vagina. Scandinavian journal of infectious diseases. Supplementum. 1983:40():31-5 [PubMed PMID: 6582587]
Anderson DJ, Marathe J, Pudney J. The structure of the human vaginal stratum corneum and its role in immune defense. American journal of reproductive immunology (New York, N.Y. : 1989). 2014 Jun:71(6):618-23. doi: 10.1111/aji.12230. Epub 2014 Mar 24 [PubMed PMID: 24661416]
Forsberg JG. Estrogen, vaginal cancer, and vaginal development. American journal of obstetrics and gynecology. 1972 May 1:113(1):83-7 [PubMed PMID: 5025001]
Level 3 (low-level) evidenceLevin RJ. Sexual arousal--its physiological roles in human reproduction. Annual review of sex research. 2005:16():154-89 [PubMed PMID: 16913291]
Dawson SJ, Sawatsky ML, Lalumière ML. Assessment of Introital Lubrication. Archives of sexual behavior. 2015 Aug:44(6):1527-35. doi: 10.1007/s10508-015-0519-z. Epub 2015 Mar 27 [PubMed PMID: 25813611]
Chambliss KL, Shaul PW. Estrogen modulation of endothelial nitric oxide synthase. Endocrine reviews. 2002 Oct:23(5):665-86 [PubMed PMID: 12372846]
Level 3 (low-level) evidenceWitkin SS, Nasioudis D, Leizer J, Minis E, Boester A, Forney LJ. Epigenetics and the vaginal microbiome: influence of the microbiota on the histone deacetylase level in vaginal epithelial cells from pregnant women. Minerva ginecologica. 2019 Apr:71(2):171-175. doi: 10.23736/S0026-4784.18.04322-8. Epub 2018 Oct 11 [PubMed PMID: 30318873]
Nunn KL, Forney LJ. Unraveling the Dynamics of the Human Vaginal Microbiome. The Yale journal of biology and medicine. 2016 Sep:89(3):331-337 [PubMed PMID: 27698617]
Leizer J, Nasioudis D, Forney LJ, Schneider GM, Gliniewicz K, Boester A, Witkin SS. Properties of Epithelial Cells and Vaginal Secretions in Pregnant Women When Lactobacillus crispatus or Lactobacillus iners Dominate the Vaginal Microbiome. Reproductive sciences (Thousand Oaks, Calif.). 2018 Jun:25(6):854-860. doi: 10.1177/1933719117698583. Epub 2017 Mar 17 [PubMed PMID: 28301987]
Egan ME, Lipsky MS. Diagnosis of vaginitis. American family physician. 2000 Sep 1:62(5):1095-104 [PubMed PMID: 10997533]
Gonçalves B, Ferreira C, Alves CT, Henriques M, Azeredo J, Silva S. Vulvovaginal candidiasis: Epidemiology, microbiology and risk factors. Critical reviews in microbiology. 2016 Nov:42(6):905-27. doi: 10.3109/1040841X.2015.1091805. Epub 2015 Dec 21 [PubMed PMID: 26690853]
Edwards T, Burke P, Smalley H, Hobbs G. Trichomonas vaginalis: Clinical relevance, pathogenicity and diagnosis. Critical reviews in microbiology. 2016 May:42(3):406-17. doi: 10.3109/1040841X.2014.958050. Epub 2014 Nov 10 [PubMed PMID: 25383648]
Hoppe-Seyler K, Bossler F, Braun JA, Herrmann AL, Hoppe-Seyler F. The HPV E6/E7 Oncogenes: Key Factors for Viral Carcinogenesis and Therapeutic Targets. Trends in microbiology. 2018 Feb:26(2):158-168. doi: 10.1016/j.tim.2017.07.007. Epub 2017 Aug 17 [PubMed PMID: 28823569]
Nuovo GJ. The role of human papillomavirus in gynecological diseases. Critical reviews in clinical laboratory sciences. 2000 Jun:37(3):183-215 [PubMed PMID: 10894184]
Level 2 (mid-level) evidenceMills BB. Vaginitis: Beyond the Basics. Obstetrics and gynecology clinics of North America. 2017 Jun:44(2):159-177. doi: 10.1016/j.ogc.2017.02.010. Epub [PubMed PMID: 28499528]
Horn LC, Klostermann K, Hautmann S, Höhn AK, Beckmann MW, Mehlhorn G. [HPV-associated alterations of the vulva and vagina. Morphology and molecular pathology]. Der Pathologe. 2011 Nov:32(6):467-75. doi: 10.1007/s00292-011-1476-5. Epub [PubMed PMID: 22038133]
Scott JR. Episiotomy and vaginal trauma. Obstetrics and gynecology clinics of North America. 2005 Jun:32(2):307-21, x [PubMed PMID: 15899363]
Quiróz-Guadarrama CD, Martínez-Ordaz JL, Rojano-Rodríguez ME, Beristain-Hernández JL, Moreno-Portillo M. [Vaginal evisceration. Report of a case and a literature review]. Ginecologia y obstetricia de Mexico. 2013 Jun:81(6):349-52 [PubMed PMID: 23837301]
Level 3 (low-level) evidenceFarage M, Maibach H. Lifetime changes in the vulva and vagina. Archives of gynecology and obstetrics. 2006 Jan:273(4):195-202 [PubMed PMID: 16208476]
Lev-Sagie A. Vulvar and Vaginal Atrophy: Physiology, Clinical Presentation, and Treatment Considerations. Clinical obstetrics and gynecology. 2015 Sep:58(3):476-91. doi: 10.1097/GRF.0000000000000126. Epub [PubMed PMID: 26125962]
Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. The Cochrane database of systematic reviews. 2016 Aug 31:2016(8):CD001500. doi: 10.1002/14651858.CD001500.pub3. Epub 2016 Aug 31 [PubMed PMID: 27577677]
Level 1 (high-level) evidenceMaher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. The Cochrane database of systematic reviews. 2016 Oct 1:10(10):CD012376 [PubMed PMID: 27696355]
Level 1 (high-level) evidenceIglesia CB, Smithling KR. Pelvic Organ Prolapse. American family physician. 2017 Aug 1:96(3):179-185 [PubMed PMID: 28762694]