Introduction
Platysmaplasty is a rejuvenation procedure performed to increase the definition of the neck from the angle of the jaw down to the chin, thereby restoring a youthful and aesthetic contour to the face. It is generally indicated in persons between 40 and 60 years of age, and for those who want improved jaw and neck definition. It is not suitable for patients above 60 years of age who have significant excess skin and fat in the neck. For these patients, other procedures, such as face-lifting and liposuction, have to be added along with a plastymaplasty. However, platysmaplasty is most commonly performed in conjunction with a full cervicofacial rhytidectomy, in which the aim is to improve everything below the lower eyelids and down to the clavicles.[1]
Bourguet (1928) was the first to describe a variation of the modern-day platysmaplasty, wherein he used a sub-mental incision to divide the prominent platysma muscle. Skoog (1969) reported a one-layer neck-lift in which the skin, subcutaneous tissue, and platysma muscle were suspended up through a lateral face-lift incision. Guerro–Santos (1978) first described lateral imbrication of the platysma to the fascia of the sternocleidomastoid muscle and mastoid periosteum. Feldman (1988) pioneered the technique of corset platysmaplasty, in which the two halves of muscle were sutured together and further cinched and shaped to recreate a youthful aesthetic neckline. Fuente del Campo (1998) published the “hammock platysmaplasty” technique, employing a double-breasted type of plication of the platysma to the contralateral mastoid fascia.[2][3][4][5]
There have been many other variations of these initial techniques which involve the use of fascia, meshes, small-incision insertion of supporting sutures, and small-incision platysmal plication with subcutaneous plasma injection to incite skin contraction.[6]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The neck is a complex anatomical structure. To obtain a youthful and aesthetically pleasing contour, a thorough knowledge of its anatomy and physiology is essential for the operating surgeon.
The neck is divided into three aesthetic subunits: (1) the chin subunit, (2) the submental subunit, and (3) the anterior neck subunit. Anatomically, the neck has three layers; skin, superficial fascia, and deep fascia. The superficial fascia consists of fat, connective tissue, platysma muscle, superficial veins, lymph nodes, and cutaneous nerves. The deep fascia has three layers: the external or investing layer of deep fascia, the middle or pretracheal fascia, and the deep or inner prevertebral fascia.
The platysma is a broad, thin muscle located in the anterolateral aspect of the neck, thicker in men than in women (see figure). It is controlled by the cervical branch of the facial nerve, which travels beneath the muscle, and its action is to assist in depressing the lower lip in concert with the depressor anguli oris. The platysma is a continuation of the superficial musculoaponeurotic system (SMAS) that begins just above the inferior border of the mandible. Both the SMAS and the platysma divide the subcutaneous fat of the neck and face into two layers. The subplatysmal plane in the neck contains the deep layer of fat, facial nerve branches, submandibular gland, the tail of the parotid gland, and the external jugular vein. In the submental and suprahyoid region, a thick fat layer overlies the platysma and becomes thinner inferiorly, such that the platysma lies in close approximation to the skin.
It is essential to understand the anatomy of the marginal mandibular and cervical branches of the facial nerve, and the great auricular nerve (GAN) when performing a neck-lift or a cervicofacial rhytidectomy.
The marginal mandibular nerve exits from the anteroinferior portion of the parotid gland and courses anteriorly and deep to the SMAS and platysma. It then courses along the inferior border of the mandible. At the mid-body of the mandible, it rises into a superficial plane between the platysma and deep fascia, and crosses the facial artery to supply the depressor labii inferioris and mentalis muscle. The "danger area" of the marginal mandibular nerve extends from the angle of the mandible to the facial artery, where it is most prone to injury if the dissection goes deep to the platysma. Therefore, the safe plane of dissection in this area is superficial to the platysma.
The cervical branch of the facial nerve, which supplies the platysma, travels along with the marginal mandibular nerve (in 20% of cases), or after exiting the parotid gland, it may travel posterior to the angle of the mandible (in 80% of cases). Ultimately, both branches diverge at the submandibular gland just anterior to the hyoid bone. The "danger area” for the cervical branch is at the level of the hyoid bone, when the dissection is deep to the platysma. Therefore, when performing a neck-lift, the surgeon must be extra-cautious while dissecting deep to the platysma in the posterior neck.
The most commonly injured nerve in rhytidectomy is the great auricular nerve. It emerges from the posterior border of the sternocleidomastoid muscle at a point 6.5 cm inferior to the external auditory meatus, known as McKinney's point. The GAN is a sensory nerve and supplies the cutaneous territory over the parotid gland and lobule of the ear. During posterior skin flap elevation, the surgeon must be careful to avoid elevating a thick flap that runs deep into the subcutaneous layer, as the GAN runs very superficial in this area.
An attractive, youthful neck is defined by the following criteria which are used in the evaluation of age-related changes in the neck, including:[7]
- Cervico-mental angle (CMA) is the angle between the chin and the neck. It should be well defined, with the ideal angle being between 105 and 120 degrees
- Mental prominence – the mentum, or chin, should be prominent, well defined, and sculpted on anterior and profile views
- Hyoid position – the ideal position of the hyoid bone is superior and posterior, thereby creating an acute and prominent CMA
- Well-defined inferior mandibular border
- Visible anterior border of the sternocleidomastoid muscle (SCM)
- Subhyoid depression
- Visible thyroid bulge (thyroid cartilage)
Some of the age-related changes leading to neck deformities can be attributed to a loss of skin elasticity due to degeneration of dermal collagen and elastin, accumulation of fat, chronic sun damage, lipodystrophy, and hormonal changes. With aging, the platysma muscle becomes lax, and the fascia supporting the midline decussation also attenuates, leading to hanging medial borders of the platysma, forming the platysmal bands. The lateral borders of the muscles may also sag. Additionally, there is ptosis of the submandibular glands, which leads to loss of definition of the mandibular border. There is also attenuation and relaxation of retaining ligaments of the face and neck. The zygomatic and masseteric cutaneous ligaments become lax and stretch, permitting a descent of facial soft tissue into the neck and leading to prominent nasolabial folds with reduction of neck-face definition. Similarly, labiomandibular folds (jowls) are caused by weakening and stretching of the masseteric cutaneous ligament and mandibulocutaneous (mandibular) ligaments, which allow the excess and lax soft tissue of the cheek to descend and spill over the inferior border of the mandible. Fat accumulation within the jowls further disrupts the jawline.[1]
The secondary changes that contribute to the aged neck include prominent labiomandibular folds or jowls, prominent nasolabial folds associated with facial soft tissue descent, loss of volume of the bony facial skeleton, and submental fullness. However, recent studies have challenged the idea that platysmal bands are due to sagging skin and muscular atony, and suggest that they are actually caused by muscular hyperactivity.[8][9][10][11][12][13][14][15][16]
Indications
Platysmaplasty is an elective cosmetic procedure and is indicated in those patients who want to reverse age-related changes in the neck, such as loose, saggy skin, platysmal bands/cords, and excess fat in the neck (turkey-gobbler neck). A standard face-lift (cervicofacial rhytidectomy) will adequately address most of these age-related neck changes and remains the gold standard, but for those patients who are unwilling to undergo a face-lift, the neck-lift or platysmaplasty remains a reasonable alternative.
Giampapa and Di Bernardo have proposed the following five criteria for neck-lift candidacy:
- A poorly-defined CMA
- A poorly-defined inferior mandibular border or jawline
- Absence of laxity in the midfacial structures
- Small to moderate amounts of jowl and neck fat
- Patients who do not want to undergo a full face-lift
Certain absolute indications for midline platysmaplasty include:
- Patients with excessive redundancy in platysmal banding (depth more than 1.5 cm) and not corrected by lateral suspension/advancement of platysma
- Subplatysmal lipectomy, if performed, must be combined with midline platysmaplasty
- Patients with a type III platysmal decussation pattern (platysma muscle split apart or dehisced from midline).[17][18]
Contraindications
There are no absolute contraindications, but certain patients are not good candidates for surgery. These include:
- Patients with unrealistic expectations
- Patients with psychiatric problems (body dysmorphic disorder, psychosis, mania, and major depression)
- Heavy smokers who do not stop smoking at least one month before surgery
- Patients who are medically unfit for surgery
- Patients who are on certain drugs like isotretinoin, which may lead to poor wound healing[19]
- Patients with significant changes along the jawline and jowls, and those with midfacial ptosis
Equipment
Equipment required for platysmaplasty includes standard facial plastic surgery instruments:
- Long and medium length needle holders
- Webster needle holder
- Metzenbaum scissors with fine, curved, blunt tips (for undermining of platysma)
- Deaver retractor
- Lighted retractors
- Fine Mayo or McIndoe scissors
- Castañares scissors
- Skin hooks
- Adson-Brown forceps
- Barron knife holder
- Fine bipolar forceps
- Monopolar electrrocautery
- Liposuction cannulae
- Nerve hooks
- Tissue elevators or dissectors
- Headlight and loupes
Personnel
The personnel involved in this procedure should include the surgeon, the surgeon's assistant, a scrub nurse, an anaesthetist, an anaesthesia technician, a circulating nurse, and a postoperative care nurse.
Preparation
Preparation before the surgery involves a detailed history, clinical examination, preoperative photography, blood workup, an anesthetic assessment, and other investigations as indicated by the patient's medical history. Clinical assessment of the signs of facial aging must include the following:
- Amount of skin excess/laxity
- Thickness and elasticity of the skin
- Signs of photoaging and solar actinosis
- Assessment of rhytids at rest and on animation. Skin pinch tests should be performed to assess the quality, thickness, and amount of fat below the skin, at rest and with animation.
It is essential to look for excess skin along the SCM and chin and thyroid cartilage area. The submental and neck fat must be evaluated, including the relative amounts of subcutaneous and sub-platysmal fat; the two fat compartments can be differentiated by pinching the skin at rest and with contraction of the platysma. When there is a reduced skin pinch size with animation, it signifies excess subplatysmal fat and vice versa. It is also vital to assess the amount of excess skin in the neck and the depth of the platysma bands both at rest and with animation. The submandibular glands and digastric muscle should also be examined by looking for a bulge below the inferior mandibular border and on neck flexion.
Patients areadvised to discontinue aspirin, non-steroidal anti-inflammatory drugs, other anticoagulants, and herbal supplements other than Arnica montana two weeks before surgery. Arnica in the perioperative period may be helpful to limit postoperative bruising.
The skin markings are made with the patient upright before surgery, using the patient's ability to smile, contract the platysma, and flex the neck to allow an accurate assessment and to mark the important structures. These include the submental incision line, jowl lines, mandibular borders, subcutaneous fat prominences in the neck, platysmal neck bands, anterior borders of the SCMs, external jugular veins, and markings for the face-lift incisions, if this is planned concomitantly with plastymaplasty. The estimated course of the greater auricular nerve is also marked on the neck. After induction of general anesthesia, the patient is scrubbed and draped in a sterile fashion. Tumescent local anesthetic solution (0.1% lidocaine with 1 in 1,000,000 adrenaline) is injected into the skin markings, and the subcutaneous neck is infiltrated with at least 100 ml of this solution.
Technique or Treatment
Over the last 50 years, many different techniques for neck-lifting/platysmaplasty have been described to rejuvenate the aging neck. Platysmaplasty is usually combined with submental liposuction and a full face-lift, if indicated. Other ancillary procedures performed along with platysmaplasty, when indicated, include supraplatysmal fat reduction, subplatysmal lipectomy, submandibular gland reduction, and partial digastric myectomy. A wide array of platysmaplasties have been described in the literature, such as the midline platysmaplasty, corset platysmaplasty, several suture techniques (plication, imbrication, overlap, suture suspension, sling platysmaplasty, and pursestring sutures), lateral platysmapexy, transverse platysma myotomy, and partial platysma myectomy.[1]
Anterior (Medial) Platysmaplasty
This is the most commonly employed technique and entails midline approximation of the platysmal diastasis from the chin to the thyroid cartilage. A transverse skin crease incision is made just caudal to the submental fold, and the skin is undermined caudally to the cricoid cartilage and beyond. Next, the platysmal bands are corrected by separating the muscle in the midline and from the anterior bellies of the digastrics.
Before approximation, the redundant medial muscle borders are trimmed and sutured together without invagination or imbrication in a smooth edge-to-edge fashion (see figure). At this stage, depending on the patient, a decision is made intraoperatively whether to excise the subplatysmal fat. The anterior platysmaplasty is not ideal for treatment of excess subplatysmal fat, prominent submandibular glands, bulky anterior bellies of the digastric muscles, or 'hard' dynamic platysmal bands. When concomitant face-lift and neck-lift is performed, platysmaplasty should be performed after cheek-SMAS flap dissection and suspension, as it provides optimal correction of cheek folds and jowls when executed last.
Lateral Platysmapexy/Platysmaplasty
Lateral platysmapexy is performed when there is a mild horizontal redundancy of the platysma. This procedure is usually performed after medial platysmaplasty and involves the suturing of the platysma to the upper quarter of the SCM fascia. Some authors advocate anchoring the lateral border of the platysma to the preauricular platysma auricular fascia, giving a more vertical vector to the support and lift. This ensures an even, smooth neck contour and consolidates the neck-lift.
When horizontal platysmal redundancy is excessive, a postauricular transposition flap (PATF) of cheek SMAS-platysma is planned. The PATF is sutured to the mastoid fascia on both sides, and this leads to an optimal reduction of horizontal platysma redundancy even when the patient looks down. This procedure is usually combined with a face-lift and should be performed only after anterior/medial platysmaplasty has been completed.
Corset Platysmaplasty (Feldman)
This is a type of anterior platysmaplasty wherein the medial borders of the platysma, after trimming, are sutured with a continuous monofilament suture that is run up and down the midline neck until the desired result is obtained (see figure). Some authors prefer buried, interrupted sutures and may do this in conjunction with a full face-lift and lateral platysmapexy, depending on the indication. Performing just a corset platysmaplasty without lateral and superior support runs the risk of bringing the platysma downwards, potentially resulting in failure of the procedure.
Hammock Platysmaplasty (Platysmal Overlap)
Fuente del Campo first described this technique of platysma overlapping in the midline; he called it "hammock platysmaplasty." It consists of overlapping the platysma in a double-breasted fashion in the middle of the neck and provides good functional muscular reconstruction and cosmesis. It was subsequently modified by Gentile, in which he used interlacing sutures through the platysma, resulting in a medial to lateral plication.
Pursestring Platysmaplasty
This technique involves interlacing a suture through the platysma in a circular fashion. When the suture is tightened, the platysma inverts and folds, thereby reducing its surface area and deepening the fold just below the mandibular border, which in turn improves jawline definition. Three varieties of pursestring platysmaplasty have been described:
Type I Pursestring platysmaplasty simply involves placing interlacing sutures just below the angle of the mandible and following its border to define it further.
Type II Pursestring platysmaplasty involves overlapping sutures on the medial border of platysma, simulating a hammock platysmaplasty.
Type III Pursestring platysmaplasty – in this type, continuous interlacing sutures are placed starting from the mastoid fascia on one side to the contralateral side and back again. Initially, non-absorbable sutures were used, but now expanded polytetrafluoroethylene (ePTFE) and barbed sutures are often preferred.
Suture Sling Platysmaplasty
In this technique, after plication and suspension of the SMAS-platysma complex, a suture or broader material (ePTFE implant) may be used to offer additional intrinsic and extrinsic support. Conrad was the first to describe placing an ePTFE implant, which is used as a sling to support the submental structures, leading to a sharper, more defined CMA. This evolving cervical sling technique yields excellent and predictable results for the correction of an obtuse CMA; an added advantage is that secondary adjustments are possible for recurrent laxity of neck tissue and submental redundancy.
Recent advances include the use of absorbable bioimplants, such as polymeric ribbon suspension devices made of polylactic acid and polyglycolic acid, which are inserted using minimal incisions and used to redrape the platysma to improve neck contour.
Transverse Platysma Myotomy
This technique is indicated to eliminate dynamic platysmal banding or striations that appear during conversation and with animation. Platysmal myotomy must be performed only after anterior platysmaplasty and lateral platysmapexy have been completed to ensure a uniform redraping and smooth redistribution of platysma around the neck. Platysma myotomy is usually performed low in the neck, at the level of cricoid cartilage, as at this level the muscle is thin and is less likely to bleed. Furthermore, a smooth transition to the CMA is obtained, and more importantly, lower lip weakness is avoided.
Partial Platysma Myectomy
Partial platysma myectomy involves the excision of a part of the platysma muscle with a full-width transection at a high mid-thyroid cartilage level. This procedure is the most effective way to restore a smooth contour in difficult necks of patients who have undergone multiple previous invasive and non-invasive skin tightening procedures, but who return with irregularities, dense subcutaneous fibrosis, muscle fibrosis, or an elderly 'skin on muscle' appearance. Such patients are refractory to the traditional platysmaplasties and will require partial platysma myectomy and secondary fat grafting at a later date.
An important point to note is that when performing a partial platysma myectomy, one must maintain a cuff of muscle posteriorly at the CMA in order to avoid injuring the marginal mandibular and cervical branches of the facial nerve.
Final Closure and Assessment
Once the neck-lift and/or face-lift has been completed, the final contouring of the superficial cervicofacial fat is performed. It is usually done under direct visualization using scissors. Still, it is vital to avoid over resection of fat as it can lead to a skeletonization of the neck and an unnatural result. This final fat sculpting ensures an even, smooth contour to the neck and a predictable outcome. It is followed by drain placement, which is routinely performed in all primary and secondary neck-lifts to avoid troublesome postoperative hematomas and seromas. After final confirmation of adequate hemostasis and neck contour, the submental incision is closed in two layers.
The patient's hair is washed and shampooed in the recovery room, allowed to dry, and tied; a final inspection is made of all the suture sites and drains. Typically no dressing is required, and patients are discharged the same day, prescribed oral antibiotics and analgesics for a week, advised to avoid direct sunlight for a few days, to sleep in a head-up position, and to call the surgeon's office if there is any bleeding, hematoma or infection in the wound.[20][21][18][22][23][24][25][26][27][28]
Complications
Complications following plastysmaplasty can be divided into early and late complications.
Early complications include hematoma, seroma, wound infection, marginal mandibular nerve injury/neuropraxia, cervical branch neuropraxia, great auricular nerve injury, wound infection, sialocele, and salivary fistulas.
Late complications include contour irregularities, asymmetrical fat removal, inadequate reduction, overcorrection, visible platysmal banding, and neck overskeletalization.
Management of Complications
Small hematomas can be drained percutaneously in the clinic. Still, significant expanding hematomas are a surgical emergency as they may cause airway compromise and skin flap necrosis. For this reason, they need to be expeditiously drained in the operating room and a continuous suction drain should be placed.
Marginal mandibular nerve injury or neuropraxia is the most common motor nerve injury and results in weakness of the ipsilateral lower lip due to denervation of the depressor anguli oris, depressor labii inferioris, and mentalis muscles. Re-exploration for marginal mandibular nerve injury is generally not indicated, as most of these injuries are traction injuries and resolve with time; they simply require regular follow up and reassurance. The use of botulinum toxin to weaken the contralateral lower lip muscles is a useful temporary measure while waiting for resolution of the neuropraxia.
Injury to the cervical branch of the facial nerve gives rise to a pseudoparalysis that mimics marginal mandibular nerve injury, as the platysma assists in the depression of the corner of the mouth and can also affect the ability of the patient to smile. These injuries can be differentiated from the marginal mandibular nerve injuries, as the patient will be able to evert the lip in pseudoparalysis because of functioning mentalis muscle. Full recovery occurs in the majority of these cases.
The great auricular nerve is the most commonly injured nerve in a neck-lift. Injuries to the GAN present as numbness around the pre-auricular region and ear lobe; sometimes injury can also lead to a painful neuroma and mass formation. Surgical exploration and excision of the neuroma are indicated in such cases. In many cases, sensation will return, but some hypesthesia often persists.
Persistent platysma bands can be treated non-surgically with the use of botulinum toxin or via re-excision and redraping of the neck skin. Contour irregularities can be corrected by fat grafting and redraping of the skin.[14][16][20][29][30][31][32]
Clinical Significance
Platymaplasty is one of the neck rejuvenation techniques used in patients who want to improve the aesthetics of their necks by reducing unwanted platysmal bands, jowls, and neck fat. This procedure is primarily indicated in patients who are in the age range from 40 to 60 years and who do not want a full face-lift surgery, but rather an aesthetic and pleasing neck with a smooth contour and a well-defined jawline. This procedure can be combined with other ancillary techniques like submental liposuction, sub-platysmal fat excision, and submandibular gland and digastric muscle excision to add more longevity and predictability to the final result.
Enhancing Healthcare Team Outcomes
With the increasing demand for rejuvenation procedures of the face and neck, neck-lifts are in demand as many patients perceive them to be less invasive and scarring than face-lifts. It is essential that when treating such patients, an interprofessional team approach is followed in order to avoid troublesome postoperative complications and litigation. The interprofessional team for a neck-lift patient should include a plastic surgeon, who is assisted by other specialists, including an internal medicine physician, anesthetist, psychiatrist, financial counselor, nurse, pharmacist, and dermatologist.
Each member of this team has a specific and important role to play to deliver holistic care to the patient and to ensure that the process is smooth, without any undue complications. For example, patients with psychiatric problems are not absolutely contraindicated for surgery, and if they are willing to acknowledge the limitations of the procedure, have realistic expectations, take appropriate medications, and undergo preoperative and postoperative counseling, surgery may be undertaken without an elevated risk of adverse outcomes.
Another important contributor to better outcomes is the experience level of the surgeon, who should be fellowship-trained and board-certified in plastic or facial plastic surgery, but the surgeon is only part of the interprofessional team. An interprofessional team with experience working together to provide cosmetic surgical care will further reduce complications and increase the chance of a safe, smooth, and successful operation. [level 3]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
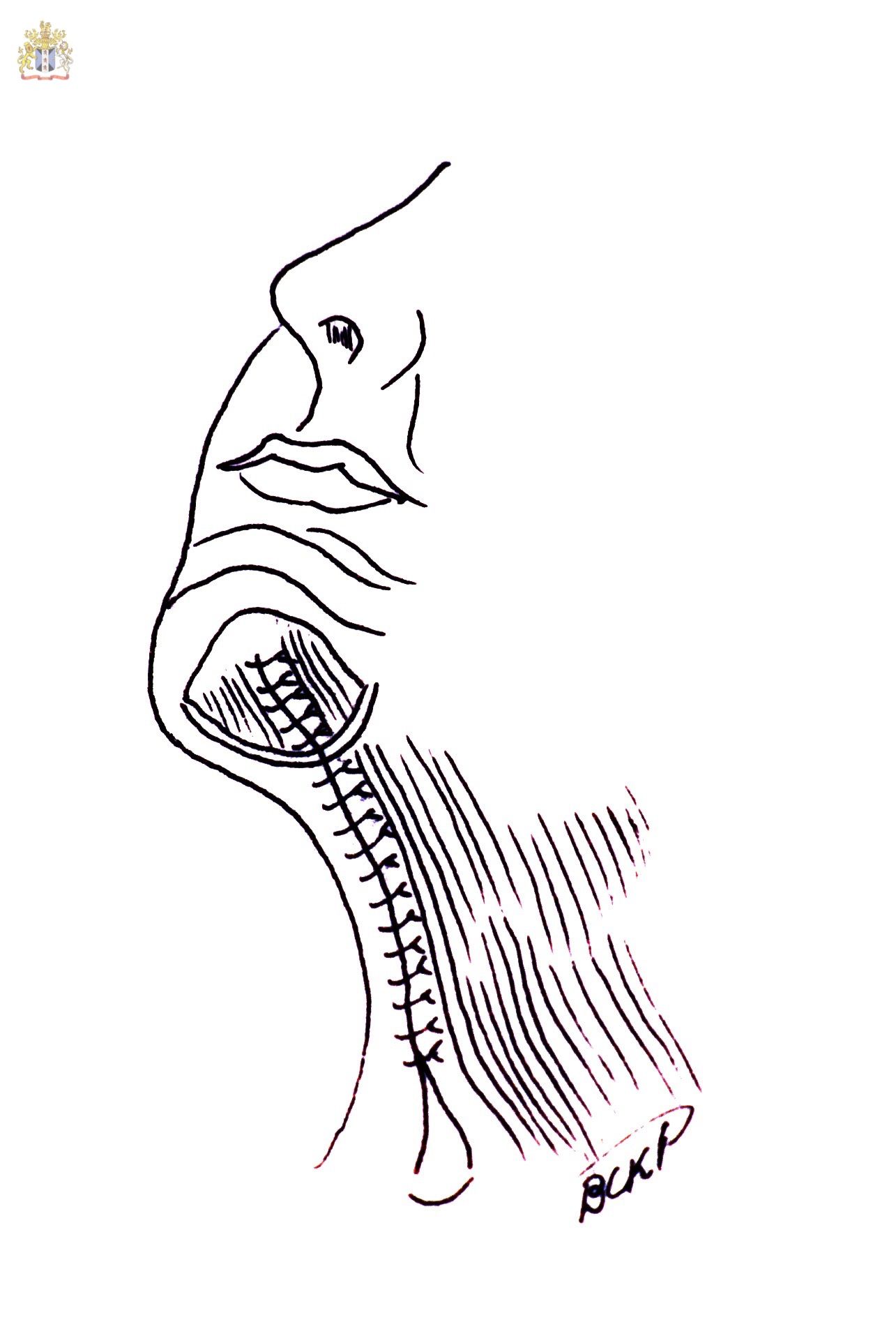
The Corset Platysmaplasty where the medial separated platysmal bands are sutured with two or three layers of sutures from the mentum to the supraclavicular zone. Some surgeons now feel that this may bring the platysma down and result in recurrence of bands in the neck and that a better way to manage the platysma is to tighten and lift it laterally and mostly superiorly with or without platysma myotomies. Contributed by Professor Bhupendra C. K. Patel MD, FRCS
References
Patrocinio LG, Naves MM, Patrocinio JA. The Facelift in South American Patients. Facial plastic surgery : FPS. 2020 Aug:36(4):416-429. doi: 10.1055/s-0040-1713848. Epub 2020 Aug 31 [PubMed PMID: 32866979]
de Castro CC. The anatomy of the platysma muscle. Plastic and reconstructive surgery. 1980 Nov:66(5):680-3 [PubMed PMID: 7433553]
Feldman JJ. Corset platysmaplasty. Clinics in plastic surgery. 1992 Apr:19(2):369-82 [PubMed PMID: 1576782]
Fuente del Campo A. Midline platysma muscular overlap for neck restoration. Plastic and reconstructive surgery. 1998 Oct:102(5):1710-4; discussion 1715 [PubMed PMID: 9774035]
Guerrero-Santos J. The role of the platysma muscle in rhytidoplasty. Clinics in plastic surgery. 1978 Jan:5(1):29-49 [PubMed PMID: 346294]
Winslow CP. Adjunctive Procedures in Facelifting. Facial plastic surgery : FPS. 2020 Aug:36(4):453-461. doi: 10.1055/s-0040-1713822. Epub 2020 Aug 31 [PubMed PMID: 32866982]
Patel BC. Aesthetic surgery of the aging neck: options and techniques. Orbit (Amsterdam, Netherlands). 2006 Dec:25(4):327-56 [PubMed PMID: 17182407]
Imanishi N, Nakajima H, Kishi K, Chang H, Aiso S. Is the platysma flap musculocutaneous? Angiographic study of the platysma. Plastic and reconstructive surgery. 2005 Apr:115(4):1018-24 [PubMed PMID: 15793439]
Ellenbogen R, Karlin JV. Visual criteria for success in restoring the youthful neck. Plastic and reconstructive surgery. 1980 Dec:66(6):826-37 [PubMed PMID: 7443846]
Guyuron B. Problem neck, hyoid bone, and submental myotomy. Plastic and reconstructive surgery. 1992 Nov:90(5):830-7; discussion 838-40 [PubMed PMID: 1410036]
Vistnes LM, Souther SG. The platysma muscle. Anatomic considerations for aesthetic surgery of the anterior neck. Clinics in plastic surgery. 1983 Jul:10(3):441-8 [PubMed PMID: 6627838]
Level 3 (low-level) evidenceTrévidic P, Criollo-Lamilla G. Platysma Bands: Is a Change Needed in the Surgical Paradigm? Plastic and reconstructive surgery. 2017 Jan:139(1):41-47. doi: 10.1097/PRS.0000000000002894. Epub [PubMed PMID: 27627054]
Furnas DW. The retaining ligaments of the cheek. Plastic and reconstructive surgery. 1989 Jan:83(1):11-6 [PubMed PMID: 2909050]
Daane SP, Owsley JQ. Incidence of cervical branch injury with "marginal mandibular nerve pseudo-paralysis" in patients undergoing face lift. Plastic and reconstructive surgery. 2003 Jun:111(7):2414-8 [PubMed PMID: 12794490]
Level 3 (low-level) evidenceZiarah HA, Atkinson ME. The surgical anatomy of the cervical distribution of the facial nerve. The British journal of oral surgery. 1981 Sep:19(3):171-9 [PubMed PMID: 6945121]
Izquierdo R, Parry SW, Boydell CL, Almand J. The great auricular nerve revisited: pertinent anatomy for SMAS-platysma rhytidectomy. Annals of plastic surgery. 1991 Jul:27(1):44-8 [PubMed PMID: 1872553]
Jacono AA, Talei B. Vertical neck lifting. Facial plastic surgery clinics of North America. 2014 May:22(2):285-316. doi: 10.1016/j.fsc.2014.01.006. Epub [PubMed PMID: 24745389]
Giampapa VC, Di Bernardo BE. Neck recontouring with suture suspension and liposuction: an alternative for the early rhytidectomy candidate. Aesthetic plastic surgery. 1995 May-Jun:19(3):217-23 [PubMed PMID: 7668166]
Rohrich RJ. Cosmetic surgery and patients who smoke: should we operate? Plastic and reconstructive surgery. 2000 Jul:106(1):137-8 [PubMed PMID: 10883626]
Choi J, Hwang K. Modified Medial and Lateral Platysmaplasty. The Journal of craniofacial surgery. 2020 Oct:31(7):1958-1961. doi: 10.1097/SCS.0000000000006515. Epub [PubMed PMID: 32472891]
Connell BF. Contouring the neck in rhytidectomy by lipectomy and a muscle sling. Plastic and reconstructive surgery. 1978 Mar:61(3):376-83 [PubMed PMID: 625501]
Nahai F. Reconsidering neck suspension sutures. Aesthetic surgery journal. 2004 Jul-Aug:24(4):365-7. doi: 10.1016/j.asj.2004.06.002. Epub [PubMed PMID: 19336181]
Owsley JQ Jr. SMAS-platysma face lift. Plastic and reconstructive surgery. 1983 Apr:71(4):573-6 [PubMed PMID: 6828592]
Henley JL, Lesnik DJ, Terk AR. Contralateral platysma suspension: an adjunct to rhytidectomy. Archives of facial plastic surgery. 2005 Mar-Apr:7(2):119-23 [PubMed PMID: 15781724]
Gentile RD. Purse-string platysmaplasty: the third dimension for neck contouring. Facial plastic surgery : FPS. 2005 Nov:21(4):296-303 [PubMed PMID: 16575707]
Level 3 (low-level) evidenceConrad K, Chapnik JS, Reifen E. E-PTFE (Gore-Tex) suspension cervical facial rhytidectomy. Archives of otolaryngology--head & neck surgery. 1993 Jun:119(6):694-8 [PubMed PMID: 8499106]
Prabhat A, Dyer WK 2nd. Improving surgery on the aging neck with an adjustable expanded polytetrafluoroethylene cervical sling. Archives of facial plastic surgery. 2003 Nov-Dec:5(6):491-501 [PubMed PMID: 14623687]
Level 2 (mid-level) evidenceKnott PD, Newman J, Keller GS, Apfelberg DB. A novel bioabsorbable device for facial suspension and rejuvenation. Archives of facial plastic surgery. 2009 Mar-Apr:11(2):129-35. doi: 10.1001/archfacial.2008.519. Epub [PubMed PMID: 19289687]
Level 2 (mid-level) evidenceBatniji RK. Complications/sequelae of neck rejuvenation. Facial plastic surgery clinics of North America. 2014 May:22(2):317-20. doi: 10.1016/j.fsc.2014.01.007. Epub [PubMed PMID: 24745390]
Ellenbogen R. Pseudo-paralysis of the mandibular branch of the facial nerve after platysmal face-lift operation. Plastic and reconstructive surgery. 1979 Mar:63(3):364-8 [PubMed PMID: 419214]
Level 3 (low-level) evidenceJones BM, Grover R. Avoiding hematoma in cervicofacial rhytidectomy: a personal 8-year quest. Reviewing 910 patients. Plastic and reconstructive surgery. 2004 Jan:113(1):381-7; discussion 388-90 [PubMed PMID: 14707663]
Level 2 (mid-level) evidencede Chalain T, Nahai F. Amputation neuromas of the great auricular nerve after rhytidectomy. Annals of plastic surgery. 1995 Sep:35(3):297-9 [PubMed PMID: 7503525]
Level 3 (low-level) evidence
