Definition/Introduction
Collaboration has become an essential competency in the national and global plan for quality improvement. There is a need to transform a culture of avoidance and isolation that continues to cause medical errors and lower patient outcomes. A necessary strategy is to improve interrelationships and interactions between health care providers (HCP) and their teams in the clinical setting.
Collaboration is a function of evidenced-based care in managing the complexity of patient care. As an academic and professional requirement, its full potential in patient care management should attain full realization. Implementation will reverse the increasing disparities in patient outcomes stemming from inadequate knowledge, skills, and thinking. As a vital element of patient safety and quality services, collaboration should be measured and monitored for effectiveness. For the determination of satisfactory benchmarks, performance should be intentional and routinely conducted by all HCP's in the clinical setting. For this reason, HCP's must train to perform collaboratively as a clinical competency.
The conceptual framework for collaboration is interprofessional.[1] The concept provides structural, functional and analytical elements that define collaboration as a clinical competency. Interprofessionality embodies processes for building relationships, communication, and other problem-solving strategies for patient safety. Interprofessional education (IPE) is a field of study for interprofessional collaboration.
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
IPE is a structured curriculum to establish competencies in collaboration. The TeamSTEPPS® 2.0 curriculum was developed by the Agency of Health Research and Quality (AHRQ) to promote collaboration as a clinical competency.[2] Based on 25 years of research, the curriculum, which originated from the US Department of Defense (DoD), was adopted by AHRQ. TeamSTEPPS® is designed to address three specific components of collaboration and teamwork: (1) performance, (2) knowledge and (3) attitudes. As shown in Figure 1, the TeamSTEPPS® model connects these three components to the essentials of leadership, situation monitoring, mutual support, and communication. This IPE curriculum is designed to shift the attitudes and behavior of HCP's towards collaboration and teamwork as a means of quality improvement.[3][4]
Figure 1: TeamSTEPPS Instructional Framework (King et al., 2008)
Clinical Significance
Communication is a multifunctional event transmitting messages of information, emotions, and attitude to other people. The significance of communication in the clinical setting is its quality to improve patient outcomes.[5] Quality is measurable in the timing, ease, organization and clarity in the acts of communication. These acts should be non-threatening and comprehensible to facilitate responses that are goal-directed in achieving specific patient outcomes.[6] Limitations give rise to ineffective communication, which is a detriment to patient safety and outcomes.[7] Communication errors are a major cause of adverse events in the clinical setting.[8]
Communication is an essential element of collaboration. TeamSTEPPS as an IPE program develops HCP in the art of communication and establishes skill sets as a standard of practice.[9] From this structured learning experience, HCP's are better prepared to collaborate and use communication skills as a clinical competency.[10]
IPE is purposeful to expand collaboration and its elements as an essential requirement for clinical practice. From this perspective, the interprofessional collaboration will advance cooperation in education, healthcare practice, research, and policy-making for continuous quality improvement in patient care services.
Media
(Click Image to Enlarge)
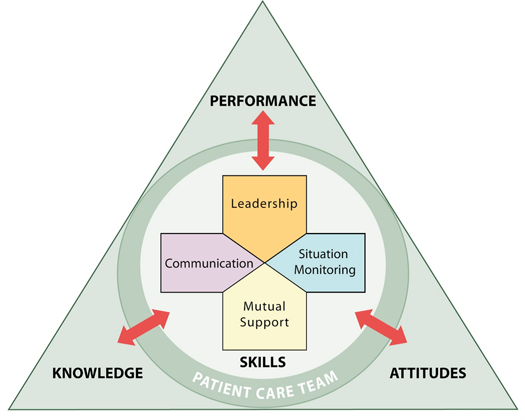
TeamStepps teaching model Contributed by King, H.B., Battles, J., Baker, D.P., Alonso, A., Salas, E., Webster, J., Toomey, L., & Salisbury, M. (2008). TeamSTEPPS: Team Strategies and Tools to Enhance Performance and Patient Safety. In K. Hendrickson, J.B. Battles, M.A. Keyes, et al. (Eds.) Advances in patient safety: New directions and alternative approaches (Vol. 3: Performance and tools). Rockville (MD): Agency for Healthcare Research and Quality. Retrieved from (http://www.ahrq.gov/downloads/pub/advances2/vol3/advances-king_1.pdf)
References
Arsever S, Tchernin E. [Interprofessionality in primary care medicine : overview and challenges for Switzerland]. Revue medicale suisse. 2018 Sep 26:14(620):1700-1703 [PubMed PMID: 30255996]
Level 3 (low-level) evidenceParker AL, Forsythe LL, Kohlmorgen IK. TeamSTEPPS(®) : An evidence-based approach to reduce clinical errors threatening safety in outpatient settings: An integrative review. Journal of healthcare risk management : the journal of the American Society for Healthcare Risk Management. 2019 Apr:38(4):19-31. doi: 10.1002/jhrm.21352. Epub 2018 Sep 13 [PubMed PMID: 30212604]
Beiler J, Opper K, Weiss M. Integrating Research and Quality Improvement Using TeamSTEPPS: A Health Team Communication Project to Improve Hospital Discharge. Clinical nurse specialist CNS. 2019 Jan/Feb:33(1):22-32. doi: 10.1097/NUR.0000000000000417. Epub [PubMed PMID: 30499846]
Level 2 (mid-level) evidenceZhu X, Baloh J, Ward MM, Stewart GL. Deliberation Makes a Difference: Preparation Strategies for TeamSTEPPS Implementation in Small and Rural Hospitals. Medical care research and review : MCRR. 2016 Jun:73(3):283-307. doi: 10.1177/1077558715607349. Epub 2015 Oct 1 [PubMed PMID: 26429835]
Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: family rounds in the intensive care unit. American journal of critical care : an official publication, American Association of Critical-Care Nurses. 2010 Sep:19(5):421-30. doi: 10.4037/ajcc2010656. Epub [PubMed PMID: 20810417]
Level 3 (low-level) evidenceOrt A, Fahr A. Using efficacy cues in persuasive health communication is more effective than employing threats - An experimental study of a vaccination intervention against Ebola. British journal of health psychology. 2018 Sep:23(3):665-684. doi: 10.1111/bjhp.12310. Epub 2018 Apr 10 [PubMed PMID: 29635864]
Dittman K, Hughes S. Increased Nursing Participation in Multidisciplinary Rounds to Enhance Communication, Patient Safety, and Parent Satisfaction. Critical care nursing clinics of North America. 2018 Dec:30(4):445-455.e4. doi: 10.1016/j.cnc.2018.07.002. Epub [PubMed PMID: 30447805]
Rodziewicz TL, Houseman B, Hipskind JE. Medical Error Reduction and Prevention. StatPearls. 2023 Jan:(): [PubMed PMID: 29763131]
Fischhoff B. Evaluating science communication. Proceedings of the National Academy of Sciences of the United States of America. 2019 Apr 16:116(16):7670-7675. doi: 10.1073/pnas.1805863115. Epub 2018 Nov 26 [PubMed PMID: 30478063]
Kiersma ME, Chen AMH, Yehle KS, Cailor S, Plake KS. Evaluation of a nursing and pharmacy student educational activity promoting interprofessional learning. Currents in pharmacy teaching & learning. 2018 Sep:10(9):1237-1242. doi: 10.1016/j.cptl.2018.06.008. Epub 2018 Jun 28 [PubMed PMID: 30497627]