Introduction
The menisci are 2 crescent-shaped structures in the knee that act as shock absorbers between the femur and tibia, dissipating stress and dispersing compressive loads.[1] They are fibrocartilaginous structures, mainly composed of type I collagen, whose functions include force transmission, increased joint congruency, and secondary stabilization of the knee.[1] The medial meniscus is typically C-shaped and intimately in contact with the surrounding capsule. The lateral meniscus is more circular in shape and has increased mobility due to fewer capsular attachments.[1]
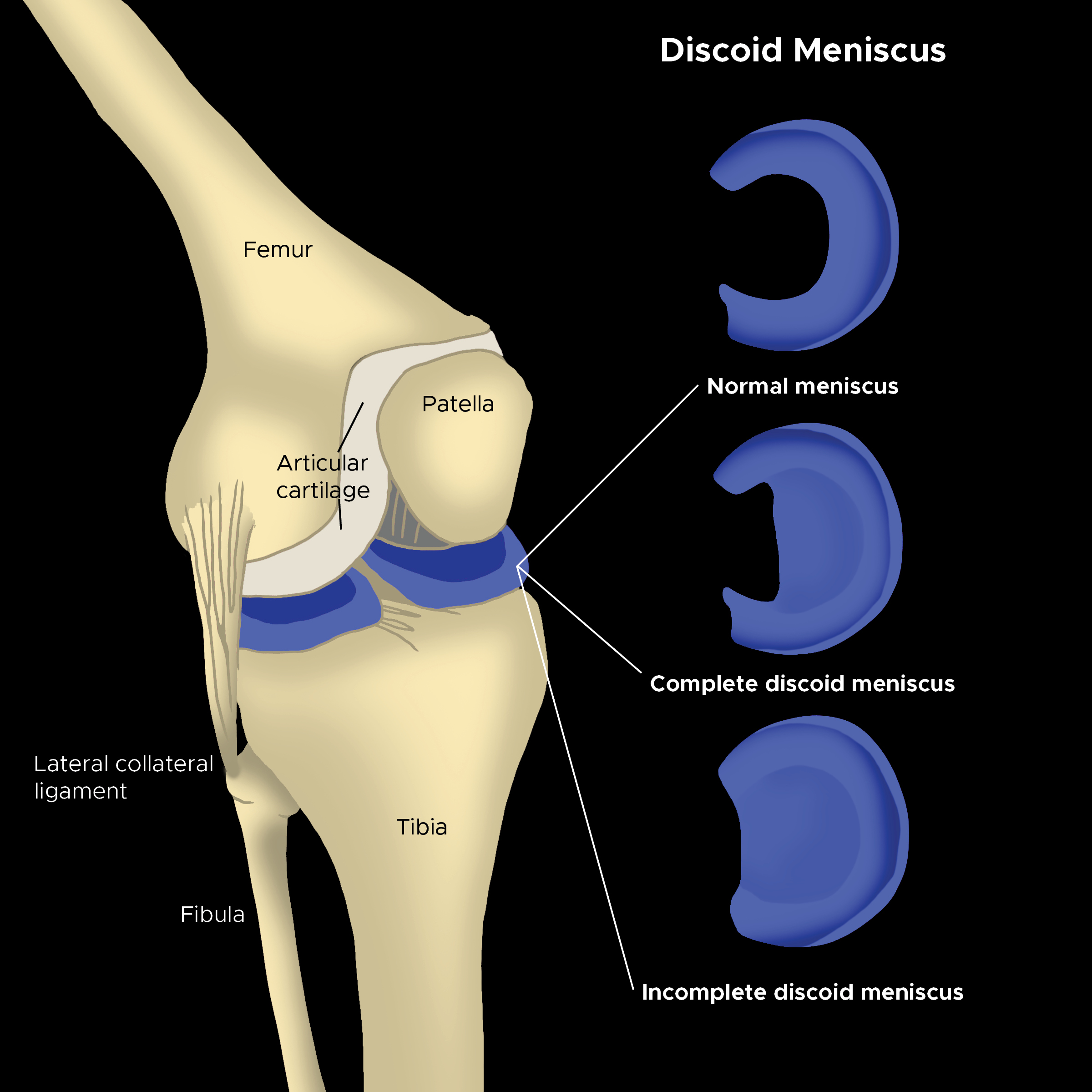
A discoid meniscus is an anatomical variant of the normal crescent-shaped meniscus. It is often thicker and is disc- or saucer-shaped.[2] These variants are more commonly susceptible to injury compared with a normally shaped meniscus.[2] When these variants are present and symptomatic, they can often lead to pain and a popping sensation within the knee, commonly referred to as “popping knee syndrome." Three types of discoid menisci have been well described in the literature based on the pattern of the meniscus: complete, incomplete, and Wrisberg variant.[3] Management consists of observation versus arthroscopic saucerization with or without meniscal repair based on the morphology and patient presentation.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Discoid meniscus has been suggested to be congenital. Much debate and several hypotheses have been presented about whether it is a true morphological variant or a structural variant. Aside from its morphological characteristics, noticeable biological behaviors have been reported with the discoid meniscus (eg, peripheral rim instability). Compared with a normal lateral meniscus, the discoid lateral meniscus (DLM) demonstrated greater instability of the anterior and posterior horns, but not the midbody, in patients who underwent surgery for a medial meniscus pathology.[4] This peripheral rim instability of the DLM could be the precipitant of more tears in this variant.
Epidemiology
The actual incidence of discoid meniscus is unknown. Sometimes, it is an incidental finding in asymptomatic patients.[3] According to many studies, the reported incidence of DLM is approximately 3% to 5% in the United States. In Asian countries, the reported incidence of DLM is much higher, with studies reporting an incidence of 10.6% in Korea and up to 13% in Japan.[2][5][6][7] On the contrary, a discoid medial meniscus is extremely rare, with literature suggesting an incidence of 0.1% to 0.3%.[2]
Up to 25% of cases of discoid meniscus have been reported to be bilateral at presentation. The incidence of bilateral DLM is also higher in Asia, up to 79% to 97% on MRI and arthroscopy of patients with symptomatic DLM in one knee.[8][9] Hence, in patients with unilateral symptomatic DLM, it is advisable to further investigate the contralateral knee. This association was reported to be 89.5% in the asymptomatic contralateral knee on arthroscopy, and 84.2% of those were identical in shape.[10]
Pathophysiology
Cadaveric fetal studies have demonstrated the existence of the discoid-shaped meniscus early in gestational development. From the second to the third trimester, it undergoes morphological development.[11][12]
The abnormal shape and composition of the discoid meniscus are thought to predispose the structure to injury.[2] Partial or full tears can occur with or without a traumatic event. Discoid meniscus tears are most often horizontal, whereas the majority of normal meniscus tears occur in a longitudinal or radial pattern.[13] The discoid meniscus, with its abnormal collagen formation, undergoes mucoid degeneration that weakens its integrity in the presence of repetitive microtrauma.[3]
Due to the abnormal size and shape of the discoid meniscus, a knee with a discoid meniscus will have abnormal biomechanics, especially in the gait cycle. A significant difference in the biomechanics of knees with torn DLM was reported when compared to knees with a torn normal lateral meniscus. The maximum lateral tibial translation was reduced by 2 mm and the maximum internal tibial rotation was reduced by 2 degrees in the torn DLM group compared with knees with a normal lateral meniscus injury.[14] In another study, sagittal and axial plane knee excursion was reported to be smaller in patients with symptomatic DLM. This was especially highlighted during the heel strike and midstance phases of the gait cycle.[15]
Histopathology
Histological examination of a discoid meniscus has shown decreased, disorganized, and degenerative collagen fibers compared with a normal meniscus.[2][3] In the discoid meniscus, the thickness of the meniscus is increased and has abnormal vascularity.[2] Poor vascularity of the inner area of the discoid meniscus has been reported.[16] Another study reported significantly low vascularity of the central area of a completed DLM compared with the intercondylar areas.[17] Other studies compared complete versus incomplete DLM and demonstrated poorer vascularity of the central areas of the incomplete DML compared with the intercondylar areas of the complete DLM.[18] It is suggested that a variety of these factors are associated with an increased risk of meniscal tears in the presence of a discoid meniscus.[2] Moreover, these factors could have consequences on the healing potential after saucerisation and repair of either a complete or incomplete DLM. This is due to the fact that the preserved tissue margin would have compromised vascularity.
In a normal meniscus, collagen fibrils are arranged in only 2 primary orientations. The majority of the fibers are circumferentially arranged, whereas the surface fibers are radially arranged.[19] In a discoid meniscus, the collagen fiber system is reported to be disorganized in children, adolescents, and adults.[16][20] In the discoid meniscus, polarizing filter microscope studies classified the DLM into seven symmetrical layers, each with a distinct orientation.[21] There is a central layer in the axial plane that is further subdivided into four zones according to the collagen fiber arrangements. In the anterior and posterior zones, the collagen fibers are radially arranged, which is suitable for anchoring the 2 meniscal ends to the tibial roots. The middle zone has medial and lateral components, the medial one with irregularly arranged collagen fibrils and the lateral one with circularly arranged fibrils parallel to the long axis of the meniscus. This collagen fibril orientation is ideal for resistance to hoop stresses, therefore, the periphery of the meniscus must be preserved in DLM surgery.[21]
History and Physical
In a greater proportion of patients, DLM presents without demonstrating any symptoms.[22] Although tears of the discoid meniscus can be asymptomatic, symptoms may only arise in cases of instability or tears.[23] Symptomatic discoid meniscus most commonly presents with anterior and lateral knee pain and effusion with or without mechanical symptoms (eg, clicking, locking, and giving way), which are most evident in extension. Additionally, the loss of flexion or extension and quadriceps wasting may be seen.[24][25][24]
The discoid meniscus has classically been referred to as “snapping knee syndrome,” where a clunk may be heard at terminal flexion. This is typically related to the unstable Wrisberg variant, with no posterior meniscotibial attachments.[26] This popping sensation is not always present but is often more common with activity and may be associated with pain, limited range of motion, and effusion.[24] The onset of symptoms may be traumatic or atraumatic in nature. Mechanical symptoms include catching, locking, and clicking and are not necessarily related to instability.[27]
Presentation of the symptomatic discoid meniscus is often influenced by the type of discoid meniscus, the presence of tear or instability, and patient age.[28]The majority of presentations occur during adolescence.[27] Younger children can present with spontaneous intermittent clunking at terminal flexion, whereas older children usually present with acute tear symptoms of the DLM.[29][30]
A comprehensive knee examination should be completed, including visual inspection, palpation, range of motion assessment, neurovascular evaluation, ligamentous stability testing, and meniscus-specific special testing.[2] Special tests specific to meniscal pathology should include medial or lateral joint-line palpation to assess tenderness; these include McMurray’s test, Apley’s compression test, and Thessaly’s test. Due to the high rate of bilateral pathology in cases of symptomatic DLM, assessment of the contralateral knee is mandatory.[31] The overall sensitivity of clinical examination in diagnosing DLM is about 88.9%.[23]
Evaluation
Evaluation of a discoid meniscus is prompted by pain or mechanical symptoms, although this can also be an incidental finding on x-ray or MRI in the setting of acute trauma.[2]
Plain Radiographs
These x-rays may be normal; however, there are well-documented radiologic features present in patients with a discoid meniscus.[2] Common findings include widened joint space in the affected compartment (up to 11 mm), squaring of the lateral femoral condyle, cupping of the lateral tibial plateau, and hypoplastic lateral tibial spine.[3][32][3]
MRI
The most valuable imaging modality for diagnosing DLM in symptomatic knees is the MRI. Findings on MRI include the “bow-tie sign,” which is three or more consecutive 5-mm thick sagittal images showing meniscal continuity, an abnormally thick or flattened meniscus on the sagittal cut, and thick/flat meniscal tissue that extends over the entirety of the involved compartment on coronal views.[2][33] In the coronal images, 2 measures have been reported to be diagnostic of DLM: a maximal meniscus width greater than 15 mm between the periphery and the free margin, and a ratio of minimum meniscus width to maximum tibia width of more than 20%.[34][35]
The challenge presents in cases of incomplete DLM, which shows up in the MRI as a near-normal meniscus appearance. The Wrisberg variant may demonstrate a hyperintense signal between the meniscus and the capsule on T2 images or anterior subluxation of the posterior horn of the lateral meniscus.[36]
MRI is also a useful diagnostic tool to evaluate for meniscal tearing and displacement of the tear and may aid in preoperative surgical planning.[2] Imaging findings should be correlated to the patient’s history and physical exam, as an incomplete discoid meniscus can appear normal on MRI.[2] Additionally, symptomatic intrasubstance pathologies may be detected on MRI that cannot be viewed by arthroscopy.[2][37]
Treatment / Management
An asymptomatic discoid meniscus that is incidentally diagnosed does not require formal surgical treatment; the patient may be observed, but regular follow-up is recommended. For cases that become symptomatic, first-line treatment is conservative management. However, the prolonged duration of symptoms before partial meniscectomy has been reported to be an independent risk factor for progression to high-grade osteoarthritis.[38]
Surgical Treatment
Surgical treatment is indicated for a symptomatic discoid meniscus that is causing pain and/or mechanical symptoms. Although an intact discoid meniscus can be symptomatic, symptoms are more likely due to a tear. Patients with occasional symptoms should be treated symptomatically, whereas persistent symptoms, severe symptoms, or a locked knee indicates surgical intervention. The objectives of operative intervention include an anatomically normal-looking meniscus and stability, as recent literature suggests anterior horn instability.
Partial or Total Meniscectomy
Historically, a partial or total meniscectomy was the first line of surgical management for a symptomatic discoid meniscus. However, the sequala of this management is the consistent development of osteoarthritic changes in the long term.[39][40][41] Meanwhile, in an era of meniscal preservation, arthroscopic saucerisation became more commonly performed.(B2)
Arthroscopic Saucerization
Arthroscopic saucerization is considered a type of partial meniscectomy.[42] This procedure reshapes the meniscus to a more anatomic crescent morphology to enhance its function and shock absorption capacity.[3] It is also important during saucerization to preserve the peripheral rim to maintain hoop stresses and meniscus stability while reducing the chances of retearing.[3] A balance should be maintained when performing saucerization, as large remaining peripheral tissue increases the chances of retear, whereas a small amount of remaining meniscal tissue increases the risk of degenerative changes.[43][44][45][43](B2)
It is well documented that the lateral meniscus has roughly twice the amount of excursion compared with the medial meniscus.[46] In cases of type C Wrisberg variant discoid meniscus, the lateral meniscus is even more hypermobile than normal, thus likely requiring arthroscopic meniscal fixation if symptomatic during saucerization to improve stability.[2]
Postoperatively, weight-bearing is at the discretion of the surgeon. Physical therapy is frequently prescribed for muscle strengthening, increasing range of motion, edema control, balance, and coordination.
Discoid Meniscus With a Tear
The chances of tearing are higher in a discoid meniscus due to abnormalities in the morphology, microarchitecture, vascularity, and the occasional lack of peripheral anchorage.[13] A discoid meniscus can be structurally compromised in 1 of 2 scenarios: peripheral rim detachment or peripheral body or intrasubstance tear.
Peripheral Rim Detachment
In this scenario, peripheral rim detachment and instability are due to the absence of the meniscotibial capsular attachment. This instability can be anterior, middle, or posterior based on the location of meniscotibial capsular detachment. There are various predictive factors of the resulting instability based on the detachment site. Anterior instability is more common in females and presents with clicking symptoms and central meniscal displacement of the anterior meniscus. Middle instability is predicted more with flexion deformity of more than 10 degrees and peripheral tear of the meniscal midbody. Posterior instability is predicted more with a central displacement of the posterior meniscus margin and peripheral tears of the anterior and midbody of the meniscus.[47]
Several well-known meniscal repair methods, such as inside-out, outside-in, or all-inside techniques, can help meniscocapular reduction and stability. More recent techniques of meniscal preservation, such as meniscopexy have been adopted and demonstrated to provide symptomatic relief in unstable peripheral rim.[48]
An anterolateral arthrotomy is performed in a meniscopexy for a discoid lateral meniscus. The anterior horn of the meniscus is then secured with sutures, retrieved from the subluxated position, and fixed to the tibia. This technique has been shown to provide clinical improvement and normalization of the meniscus morphology at a median follow-up of 4.5 years.[49]
Other stabilization techniques involve using an all-suture anchor to stabilize the peripheral rim and centralize the extruded lateral meniscus or performing saucerization of the discoid portion, leaving an intact peripheral rim of 10 mm.[50] In cases of rim instability, stabilization with an all-suture anchor is performed, in which sutures are shuttled through the meniscus and tied insitu to prevent lateral subluxation.[51] The literature has also described the preservation of the whole meniscal tissue without any reshaping or saucerization. In these cases, inside-out vertical mattress-stacked sutures were performed and augmented with fibrin clots.[52]
Peripheral Body or Intrasubstance tear
Horizontal cleavage tear with central meniscal mucoid degeneration is the most common type of tear in DLM compared with longitudinal and radial tears.[53] Horizontal tears can be managed by reshaping to symmetrical superior and inferior leaflets, which can be repaired by all-inside techniques or inside-out sutures.[54] Biological augmentation of meniscal repair with rasping, trephination, microfracture, or fibrin clots has been demonstrated to enhance healing when an isolated meniscal repair is performed.[55](B3)
Posterolateral Loss Type Tear
These are peripheral tears at the meniscocapsular junction, either in the anterior or posterior horns or mid-body. Meniscal preservation with these types of tears is challenging and often results in subtotal meniscectomy.[56] A repair technique with augmentation using the central portion of the discoid meniscus has been reported in the literature.[57]
Differential Diagnosis
A symptomatic discoid meniscus commonly presents with knee pain, catching, locking, clicking, effusion, and limited range of motion.[2] A detailed physical exam of the affected and unaffected knee and obtaining appropriate imaging studies are important. The following conditions should be considered in the differential diagnosis:
- Meniscus tear
- Anterior cruciate ligament tear
- Posterior cruciate ligament tear
- Medial collateral ligament tear
- Lateral collateral ligament tear
- Posterior lateral corner injury
- Patella or quadriceps tendonitis
- Patellofemoral pain
- Fracture
Staging
Watanabe Classification
This system was proposed by Watanabe and Ikeuchi in 1969. Despite being the most commonly used classification, it does not guide management or prognosis. The DLMs are classified into three types:
- Type I (complete/stable): A disc-shaped meniscus that completely covers the lateral tibial plateau, with normal posterior meniscotibial attachments
- Type II (incomplete/stable): Covers up to 80% of the lateral tibial plateau; semilunar in shape with normal posterior meniscotibial attachments
- Type III (Wrisberg variant/unstable): More normal shape compared with types I and II; normal posterior meniscal attachment (coronary ligament) is missing; only the Wrisberg ligament remains as a connection to the posterior horn of the lateral meniscus, making it an unstable variant [3][24]
Good et al Classification
Hypermobility due to peripheral rim instability was reported in almost 28% of symptomatic DLMs and could be either anterior or posterior regardless of the type of discoid meniscus.[58] Good et al classified the DLMs into complete and incomplete, and further subclassified them as stable or unstable. Based on the location, instability is categorized as either anterior or posterior. The presence of tears in the meniscus body is taken into account in their classification. This classification is more useful in formulating management plans.
Ahn et al Classification
This is an MRI-based classification. It depends on the degree of meniscal shift due to peripheral capsular detachment and serves as guidance for deciding on the treatment strategy in symptomatic DLMs.[56] Ahn et al classified the DLMs as no shift (no capsular detachment), anterior and central shift (posterior horn detachment), posterior and central shift (anterior horn detachment), and central shift (posterolateral detachment with a displacement of the whole meniscus). Thickening of the Wrisberg ligament and a high degree of femoral attachment on MRI were reported to be positively correlated with posterior and central shift type of peripheral detachment[59]
Prognosis
Partial meniscectomy with or without meniscus repair for symptomatic discoid meniscus has reported good to excellent clinical outcomes in the current literature. Multiple studies with 5 years of follow-up report favorable results in about 85% of cases.[2]
Partial meniscectomy has been shown to be favorable compared with total or subtotal meniscectomy.[60] After total meniscectomy, the increased contact pressures without adequate meniscus to function as a shock absorber is likely to increase the risk of degenerative joint disease.[60]
Complications
Articular Cartilage Injuries
injuries to the knee articular cartilage can be present in patients with symptomatic DLM. Certain risk factors are predictive of articular cartilage involvement, such as a longer duration of symptoms (more than 6 months), a high degree of activity, and an asymmetrical shape of the DLM.[61][62] The preoperative history of longer symptom duration and the complaint of extension block were reported to have the highest sensitivity (71.4%) and specificity (75%) in predicting articular cartilage injury in cases of symptomatic DLM at the time of surgery.[63]
Osteochondritis Dissecans
Postoperatively, a potential unique complication to saucerization of the meniscus is an osteochondritis dissecans (OCD) lesion of the lateral femoral condyle. Repeated impaction of the chondral surface after partial meniscectomy is thought to predispose a patient to this issue, and clinicians should be aware of this potential outcome.[2]
Postoperative and Rehabilitation Care
There is no universal rehabilitation program following operative intervention for discoid meniscus.
Isolated Saucerization or Meniscectomy
Following an isolated saucerization or meniscectomy, immediate weight-bearing and a full range of motion (ROM) can be permitted. The initial physiotherapy regimen should be focused on swelling reduction by icing, followed by quadriceps strengthening exercises at 2 weeks postoperatively. At 8 weeks postoperatively, full ROM and strength should have been achieved, and progressive return to sports and recreational activities should ensue.[64]
Combined Saucerization With Meniscal Repair
Patients who undergo combined saucerization with meniscal repair should be rehabilitated initially with protected weighted-bearing and ROM restrictions. This should be followed by progressive weight-bearing and ROM, aiming to achieve full ROM and full weight-bearing at 6 to 8 weeks. There is no set time for return to sports in these children, and this is guided on a case-by-case basis. Usually, it takes 3 to 4 months until full ROM and full strength is achieved.[64]
Deterrence and Patient Education
If a discoid meniscus is diagnosed incidentally in the absence of symptoms, no formal treatment is indicated. However, if a discoid meniscus is causing mechanical or painful symptoms, surgery is warranted. There should be a thorough discussion of the risks and benefits of operative and nonoperative management with patients (and their legal guardians if they are underage), so they can make an informed decision. The outcomes after surgery in young patients are good to excellent.
Enhancing Healthcare Team Outcomes
The diagnosis and management of discoid meniscus are handled by an interprofessional team that includes a primary care provider, nurse practitioner, sports physician, orthopedic surgeon, radiologist, and a physical therapist. All personnel are essential in optimizing patient outcomes.[65]
Media
(Click Image to Enlarge)
References
Farrell C, Shamrock AG, Black AC, Kiel J. Anatomy, Bony Pelvis and Lower Limb: Medial Meniscus. StatPearls. 2024 Jan:(): [PubMed PMID: 30725961]
Kim JG, Han SW, Lee DH. Diagnosis and Treatment of Discoid Meniscus. Knee surgery & related research. 2016 Dec 1:28(4):255-262. doi: 10.5792/ksrr.16.050. Epub [PubMed PMID: 27894171]
Kramer DE, Micheli LJ. Meniscal tears and discoid meniscus in children: diagnosis and treatment. The Journal of the American Academy of Orthopaedic Surgeons. 2009 Nov:17(11):698-707 [PubMed PMID: 19880680]
Kim JH, Bin SI, Lee BS, Kim JM, Kim NK, Lee CR. Does discoid lateral meniscus have inborn peripheral rim instability? Comparison between intact discoid lateral meniscus and normal lateral meniscus. Archives of orthopaedic and trauma surgery. 2018 Dec:138(12):1725-1730. doi: 10.1007/s00402-018-2987-9. Epub 2018 Jul 5 [PubMed PMID: 29974190]
Fukuta S, Masaki K, Korai F. Prevalence of abnormal findings in magnetic resonance images of asymptomatic knees. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2002:7(3):287-91 [PubMed PMID: 12077651]
Jordan MR. Lateral Meniscal Variants: Evaluation and Treatment. The Journal of the American Academy of Orthopaedic Surgeons. 1996 Jul:4(4):191-200 [PubMed PMID: 10795054]
Kim SJ, Lee YT, Kim DW. Intraarticular anatomic variants associated with discoid meniscus in Koreans. Clinical orthopaedics and related research. 1998 Nov:(356):202-7 [PubMed PMID: 9917685]
Ahn JH, Lee SH, Yoo JC, Lee HJ, Lee JS. Bilateral discoid lateral meniscus in knees: evaluation of the contralateral knee in patients with symptomatic discoid lateral meniscus. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2010 Oct:26(10):1348-56. doi: 10.1016/j.arthro.2010.02.008. Epub 2010 Aug 21 [PubMed PMID: 20729026]
Bae JH, Lim HC, Hwang DH, Song JK, Byun JS, Nha KW. Incidence of bilateral discoid lateral meniscus in an Asian population: an arthroscopic assessment of contralateral knees. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012 Jul:28(7):936-41. doi: 10.1016/j.arthro.2011.12.003. Epub 2012 Feb 24 [PubMed PMID: 22365266]
Level 2 (mid-level) evidenceChung JY, Roh JH, Kim JH, Kim JJ, Min BH. Bilateral occurrence and morphologic analysis of complete discoid lateral meniscus. Yonsei medical journal. 2015 May:56(3):753-9. doi: 10.3349/ymj.2015.56.3.753. Epub [PubMed PMID: 25837182]
Aydın Kabakçı AD,Büyükmumcu M,Akın D,Bilge O, Morphological structure and variations of fetal lateral meniscus: the significance in convenient diagnosis and treatment. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2019 Jan 17; [PubMed PMID: 30656371]
Murlimanju BV, Nair N, Ray B, Pai MM, Amin S, Pai SR. Morphological variants of lateral meniscus of the knee: a cadaveric study in South Indian human fetuses. Anatomical science international. 2011 Jun:86(2):63-8. doi: 10.1007/s12565-010-0088-0. Epub 2010 Jun 15 [PubMed PMID: 20549581]
Good CR, Green DW, Griffith MH, Valen AW, Widmann RF, Rodeo SA. Arthroscopic treatment of symptomatic discoid meniscus in children: classification, technique, and results. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2007 Feb:23(2):157-63 [PubMed PMID: 17276223]
Lin Z, Huang W, Ma L, Chen L, Huang Z, Zeng X, Xia H, Zhang Y. Kinematic features in patients with lateral discoid meniscus injury during walking. Scientific reports. 2018 Mar 22:8(1):5053. doi: 10.1038/s41598-018-22935-0. Epub 2018 Mar 22 [PubMed PMID: 29567979]
Harato K, Sakurai A, Kudo Y, Nagura T, Masumoto K, Otani T, Niki Y. Three-dimensional knee kinematics in patients with a discoid lateral meniscus during gait. The Knee. 2016 Aug:23(4):622-6. doi: 10.1016/j.knee.2015.10.007. Epub 2016 Mar 12 [PubMed PMID: 26979382]
Bisicchia S, Botti F, Tudisco C. Discoid lateral meniscus in children and adolescents: a histological study. Journal of experimental orthopaedics. 2018 Sep 24:5(1):39. doi: 10.1186/s40634-018-0153-5. Epub 2018 Sep 24 [PubMed PMID: 30251229]
Furumatsu T, Maehara A, Okazaki Y, Ozaki T. Intercondylar and central regions of complete discoid lateral meniscus have different cell and matrix organizations. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2018 Sep:23(5):811-818. doi: 10.1016/j.jos.2018.05.006. Epub 2018 Jun 22 [PubMed PMID: 29937131]
Inoue H, Furumatsu T, Maehara A, Tanaka T, Ozaki T. Histological and biological comparisons between complete and incomplete discoid lateral meniscus. Connective tissue research. 2016 Sep:57(5):408-16. doi: 10.1080/03008207.2016.1195827. Epub 2016 Jun 7 [PubMed PMID: 27267748]
Aspden RM, Yarker YE, Hukins DW. Collagen orientations in the meniscus of the knee joint. Journal of anatomy. 1985 May:140 ( Pt 3)(Pt 3):371-80 [PubMed PMID: 4066476]
Level 3 (low-level) evidencePapadopoulos A, Kirkos JM, Kapetanos GA. Histomorphologic study of discoid meniscus. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2009 Mar:25(3):262-8. doi: 10.1016/j.arthro.2008.10.006. Epub 2008 Dec 5 [PubMed PMID: 19245988]
Cui JH, Min BH. Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2007 Jun:23(6):635-41 [PubMed PMID: 17560478]
Kelly BT, Green DW. Discoid lateral meniscus in children. Current opinion in pediatrics. 2002 Feb:14(1):54-61 [PubMed PMID: 11880735]
Level 3 (low-level) evidenceKocher MS, DiCanzio J, Zurakowski D, Micheli LJ. Diagnostic performance of clinical examination and selective magnetic resonance imaging in the evaluation of intraarticular knee disorders in children and adolescents. The American journal of sports medicine. 2001 May-Jun:29(3):292-6 [PubMed PMID: 11394597]
Level 2 (mid-level) evidenceKushare I, Klingele K, Samora W. Discoid Meniscus: Diagnosis and Management. The Orthopedic clinics of North America. 2015 Oct:46(4):533-40. doi: 10.1016/j.ocl.2015.06.007. Epub 2015 Aug 6 [PubMed PMID: 26410641]
Mutlu S, Mutlu H, Mutlu B, Guler O, Duymus TM. Symptoms of discoid lateral menisci. Journal of orthopaedics. 2014 Dec:11(4):180-2. doi: 10.1016/j.jor.2014.06.005. Epub 2014 Jul 18 [PubMed PMID: 25561753]
Wong T, Wang CJ. Functional analysis on the treatment of torn discoid lateral meniscus. The Knee. 2011 Dec:18(6):369-72. doi: 10.1016/j.knee.2010.07.002. Epub 2010 Aug 8 [PubMed PMID: 20692839]
Level 2 (mid-level) evidenceFrancavilla ML, Restrepo R, Zamora KW, Sarode V, Swirsky SM, Mintz D. Meniscal pathology in children: differences and similarities with the adult meniscus. Pediatric radiology. 2014 Aug:44(8):910-25; quiz 907-9. doi: 10.1007/s00247-014-3022-0. Epub 2014 Jul 25 [PubMed PMID: 25060615]
Tapasvi S, Shekhar A, Eriksson K. Discoid lateral meniscus: current concepts. Journal of ISAKOS : joint disorders & orthopaedic sports medicine. 2021 Jan:6(1):14-21. doi: 10.1136/jisakos-2017-000162. Epub 2020 Sep 16 [PubMed PMID: 33833041]
Andrish JT. Meniscal Injuries in Children and Adolescents: Diagnosis and Management. The Journal of the American Academy of Orthopaedic Surgeons. 1996 Oct:4(5):231-237 [PubMed PMID: 10795058]
Carter CW, Hoellwarth J, Weiss JM. Clinical outcomes as a function of meniscal stability in the discoid meniscus: a preliminary report. Journal of pediatric orthopedics. 2012 Jan-Feb:32(1):9-14. doi: 10.1097/BPO.0b013e31823d8338. Epub [PubMed PMID: 22173381]
Level 2 (mid-level) evidencePatel NM, Cody SR, Ganley TJ. Symptomatic bilateral discoid menisci in children: a comparison with unilaterally symptomatic patients. Journal of pediatric orthopedics. 2012 Jan-Feb:32(1):5-8. doi: 10.1097/BPO.0b013e31823d3500. Epub [PubMed PMID: 22173380]
Level 2 (mid-level) evidenceRao PS, Rao SK, Paul R. Clinical, radiologic, and arthroscopic assessment of discoid lateral meniscus. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2001 Mar:17(3):275-277 [PubMed PMID: 11239348]
Silverman JM, Mink JH, Deutsch AL. Discoid menisci of the knee: MR imaging appearance. Radiology. 1989 Nov:173(2):351-4 [PubMed PMID: 2798867]
Araki Y, Ashikaga R, Fujii K, Ishida O, Hamada M, Ueda J, Tsukaguchi I. MR imaging of meniscal tears with discoid lateral meniscus. European journal of radiology. 1998 May:27(2):153-60 [PubMed PMID: 9639142]
Samoto N, Kozuma M, Tokuhisa T, Kobayashi K. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magnetic resonance imaging. 2002 Jan:20(1):59-64 [PubMed PMID: 11973030]
Singh K, Helms CA, Jacobs MT, Higgins LD. MRI appearance of Wrisberg variant of discoid lateral meniscus. AJR. American journal of roentgenology. 2006 Aug:187(2):384-7 [PubMed PMID: 16861542]
Hamada M, Shino K, Kawano K, Araki Y, Matsui Y, Doi T. Usefulness of magnetic resonance imaging for detecting intrasubstance tear and/or degeneration of lateral discoid meniscus. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 1994 Dec:10(6):645-53 [PubMed PMID: 7880357]
Level 3 (low-level) evidenceAhn JH, Kang DM, Choi KJ. Risk factors for radiographic progression of osteoarthritis after partial meniscectomy of discoid lateral meniscus tear. Orthopaedics & traumatology, surgery & research : OTSR. 2017 Dec:103(8):1183-1188. doi: 10.1016/j.otsr.2017.09.013. Epub 2017 Oct 5 [PubMed PMID: 28987527]
Washington ER 3rd, Root L, Liener UC. Discoid lateral meniscus in children. Long-term follow-up after excision. The Journal of bone and joint surgery. American volume. 1995 Sep:77(9):1357-61 [PubMed PMID: 7673286]
Level 2 (mid-level) evidenceManzione M, Pizzutillo PD, Peoples AB, Schweizer PA. Meniscectomy in children: a long-term follow-up study. The American journal of sports medicine. 1983 May-Jun:11(3):111-5 [PubMed PMID: 6688155]
Medlar RC, Mandiberg JJ, Lyne ED. Meniscectomies in children. Report of long-term results (mean, 8.3 years) of 26 children. The American journal of sports medicine. 1980 Mar-Apr:8(2):87-92 [PubMed PMID: 6892670]
Fujikawa K, Iseki F, Mikura Y. Partial resection of the discoid meniscus in the child's knee. The Journal of bone and joint surgery. British volume. 1981:63-B(3):391-5 [PubMed PMID: 7263752]
Level 3 (low-level) evidenceAtay OA, Doral MN, Leblebicioğlu G, Tetik O, Aydingöz U. Management of discoid lateral meniscus tears: observations in 34 knees. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2003 Apr:19(4):346-52 [PubMed PMID: 12671616]
Level 2 (mid-level) evidenceHayashi LK, Yamaga H, Ida K, Miura T. Arthroscopic meniscectomy for discoid lateral meniscus in children. The Journal of bone and joint surgery. American volume. 1988 Dec:70(10):1495-500 [PubMed PMID: 3198675]
Yamasaki S, Hashimoto Y, Takigami J, Terai S, Takahashi S, Nakamura H. Risk Factors Associated With Knee Joint Degeneration After Arthroscopic Reshaping for Juvenile Discoid Lateral Meniscus. The American journal of sports medicine. 2017 Mar:45(3):570-577. doi: 10.1177/0363546516668623. Epub 2016 Oct 22 [PubMed PMID: 28272930]
Bryceland JK, Powell AJ, Nunn T. Knee Menisci. Cartilage. 2017 Apr:8(2):99-104. doi: 10.1177/1947603516654945. Epub 2016 Jul 7 [PubMed PMID: 28345407]
Kang MS, Kim JM, Park SS, Bin SI. Prediction of the Peripheral Rim Instability of the Discoid Lateral Meniscus in Children by Using Preoperative Clinicoradiological Factors. Journal of pediatric orthopedics. 2019 Nov/Dec:39(10):e761-e768. doi: 10.1097/BPO.0000000000001370. Epub [PubMed PMID: 30950939]
Gilbert RE, Gallacher PD, Roberts AP. Meniscopexy (anterior horn transfer) for discoid lateral menisci. Annals of the Royal College of Surgeons of England. 2010 Apr:92(3):257 [PubMed PMID: 20412677]
Johnson B, Heaver C, Gilbert R, Roberts A. Anterior meniscopexy: a meniscal sparing technique for the treatment of locking but intact discoid lateral meniscus. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2018 Apr:26(4):1158-1163. doi: 10.1007/s00167-017-4546-2. Epub 2017 Apr 27 [PubMed PMID: 28451708]
Koga H, Muneta T, Yagishita K, Watanabe T, Mochizuki T, Horie M, Nakamura T, Okawa A, Sekiya I. Arthroscopic centralization of an extruded lateral meniscus. Arthroscopy techniques. 2012 Dec:1(2):e209-12. doi: 10.1016/j.eats.2012.08.001. Epub 2012 Oct 22 [PubMed PMID: 23766997]
Ohnishi Y, Nakashima H, Suzuki H, Nakamura E, Sakai A, Uchida S. Arthroscopic treatment for symptomatic lateral discoid meniscus: The effects of different ages, groups and procedures on surgical outcomes. The Knee. 2018 Dec:25(6):1083-1090. doi: 10.1016/j.knee.2018.06.003. Epub 2018 Aug 13 [PubMed PMID: 30115588]
Kinugasa K, Hamada M, Yonetani Y, Matsuo T, Mae T, Nakata K, Horibe S. Discoid lateral meniscal repair without saucerization for adolescents with peripheral longitudinal tear. The Knee. 2019 Jun:26(3):803-808. doi: 10.1016/j.knee.2019.03.007. Epub 2019 May 7 [PubMed PMID: 31076246]
Elvey MH, Konan S, House CV, Patel RV. Horizontal cleavage tear of discoid medial meniscus diagnosed on MRI and treated with arthroscopic partial resection. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2011 Nov:19(11):1860-7. doi: 10.1007/s00167-011-1487-z. Epub 2011 Mar 29 [PubMed PMID: 21445591]
Level 3 (low-level) evidenceZuke WA, Cvetanovich GL, Go B, Forsythe B. Arthroscopic Saucerization and All-Inside Repair of a Delaminated Discoid Lateral Meniscus. Arthroscopy techniques. 2017 Aug:6(4):e1387-e1391. doi: 10.1016/j.eats.2017.05.018. Epub 2017 Aug 21 [PubMed PMID: 29354445]
Ghazi Zadeh L, Chevrier A, Farr J, Rodeo SA, Buschmann MD. Augmentation Techniques for Meniscus Repair. The journal of knee surgery. 2018 Jan:31(1):99-116. doi: 10.1055/s-0037-1602247. Epub 2017 May 2 [PubMed PMID: 28464195]
Ahn JH, Lee SH, Yoo JC, Lee YS, Ha HC. Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow-up. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2008 Aug:24(8):888-98. doi: 10.1016/j.arthro.2008.03.002. Epub 2008 May 5 [PubMed PMID: 18657737]
Kim SJ, Chang WH, Lee SK, Chung JH, Ryu KJ, Kim SG. Posterior Horn Repair Augmented With the Central Portion of Thickened Meniscus for Large Posterolateral Corner Loss Type of Discoid Lateral Meniscus. Arthroscopy techniques. 2019 Jan:8(1):e65-e73. doi: 10.1016/j.eats.2018.09.004. Epub 2018 Dec 24 [PubMed PMID: 30899653]
Klingele KE, Kocher MS, Hresko MT, Gerbino P, Micheli LJ. Discoid lateral meniscus: prevalence of peripheral rim instability. Journal of pediatric orthopedics. 2004 Jan-Feb:24(1):79-82 [PubMed PMID: 14676539]
Ahn JH, Wang JH, Kim DU, Lee DK, Kim JH. Does high location and thickness of the Wrisberg ligament affect discoid lateral meniscus tear type based on peripheral detachment? The Knee. 2017 Dec:24(6):1350-1358. doi: 10.1016/j.knee.2017.07.012. Epub 2017 Aug 17 [PubMed PMID: 28823807]
Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2015 May:31(5):867-73. doi: 10.1016/j.arthro.2014.12.012. Epub 2015 Feb 7 [PubMed PMID: 25665957]
Ding J, Zhao J, He Y, Huangfu X, Zeng B. Risk factors for articular cartilage lesions in symptomatic discoid lateral meniscus. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2009 Dec:25(12):1423-6. doi: 10.1016/j.arthro.2009.06.024. Epub [PubMed PMID: 19962069]
Level 2 (mid-level) evidenceFu D, Guo L, Yang L, Chen G, Duan X. Discoid lateral meniscus tears and concomitant articular cartilage lesions in the knee. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2014 Mar:30(3):311-8. doi: 10.1016/j.arthro.2013.11.029. Epub [PubMed PMID: 24581255]
Lau BC, Vashon T, Janghala A, Pandya NK. The Sensitivity and Specificity of Preoperative History, Physical Examination, and Magnetic Resonance Imaging to Predict Articular Cartilage Injuries in Symptomatic Discoid Lateral Meniscus. Journal of pediatric orthopedics. 2018 Oct:38(9):e501-e506. doi: 10.1097/BPO.0000000000001221. Epub [PubMed PMID: 30036288]
Kocher MS, Logan CA, Kramer DE. Discoid Lateral Meniscus in Children: Diagnosis, Management, and Outcomes. The Journal of the American Academy of Orthopaedic Surgeons. 2017 Nov:25(11):736-743. doi: 10.5435/JAAOS-D-15-00491. Epub [PubMed PMID: 29059110]
Peek GK, Campbell U. Interdisciplinary relationship dynamics. American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists. 2020 Mar 5:77(6):424-426. doi: 10.1093/ajhp/zxz353. Epub [PubMed PMID: 31961385]