Introduction
The term “ptosis” is derived from the Greek word falling and refers to drooping of a body part. Blepharoptosis is upper eyelid drooping with the eyes in the primary position of gaze.
The shape of one's eyes along with the position of the eyelids, shape, and position of the eyebrow determines one's identity. Hence, drooping of the eyelids may produce a functional or a cosmetic deficit.
Ptosis can occur in all age groups and is the result of various factors. One must remember that when a patient presents with complaints of drooping, it is a mere symptom and not the diagnosis. A thorough evaluation is of utmost importance to determine the cause.
Ptosis can classify as true ptosis or pseudoptosis. True ptosis is further classified based on the age of presentation into congenital ptosis and acquired ptosis.[1]
Acquired adult ptosis is further classified based upon the etiological factors as
- Aponeurotic ptosis
- Neurogenic ptosis
- Myogenic ptosis
- Mechanical ptosis
- Traumatic ptosis
Aponeurotic ptosis
Aponeurotic ptosis is the most prevalent form of adult ptosis and usually presents in the 5th or 6th decade of life. It is also known as involutional ptosis. However, it can occur in young individuals following trauma, recent eyelid swelling, ocular surgery or prolonged use of contact lenses. The pathogenesis of aponeurotic ptosis is most often due to dehiscence or disinsertion of the levator aponeurosis.[2] In involutional cases, true dehiscence is sometimes absent, and ptosis occurs due to stretching or thinning of the aponeurosis. Rarely the levator muscle shows fatty infiltration.
Characteristic features of this type of ptosis are that patients have a good levator function with a high lid crease, affected eyelid appears lower on down gaze and a thin upper eyelid with redundant skin.
Neurogenic ptosis
Neurogenic ptosis results from any condition which disrupts the innervation of either the levator muscle or muller’s muscle. The varieties most commonly encountered by an ophthalmologist are 3rd cranial nerve palsy and Horner syndrome.
Third cranial nerve palsy
Lesions along the oculomotor nerve present with ptosis and restriction of adduction, elevation and depression movements of the eyeball. Pupillary involvement may or may not be present. Bell's phenomenon is usually poor. Pupil-involving third nerve palsy is considered a neurological as it is most often due to a posterior communicating artery aneurysm compressing the nerve. Pupil-sparing third nerve palsy is most often due to an ischemic vascular cause and usually resolves spontaneously in 3 months. Other causes include inflammation, trauma or tumors along the course of the nerve. Lesions of the superior orbital fissure, orbital apex, or cavernous sinus, present in combination with other cranial nerve palsies.
Treatment is challenging as the patients have a poor or absent Bell’s phenomenon placing them at high risk of developing exposure keratopathy post-surgery. Ideally, strabismus surgery is done first to correct the deviation followed by ptosis correction via the frontalis sling technique with planned under-correction.
Horner syndrome (Oculosympathetic paresis)
Horner syndrome consists of mild ptosis, pupillary miosis, apparent enophthalmos, and anhidrosis. It occurs due to interruption of the sympathetic nerve supply to the muller’s muscle and dilator pupillae muscle.
Pupillary anisocoria can be well demonstrated in dim illumination. Patients with Horner’s syndrome occurring during childhood also have iris heterochromia due to decreased melanin production in melanocytes which is controlled by the sympathetic pathway.
The diagnosis of Horner syndrome is often made clinically. Pharmacological tests using 4% cocaine, 1% hydroxyamphetamine or 2.5% phenylephrine help confirm the diagnosis.
Myogenic ptosis
Myogenic ptosis arises due to an abnormality in the levator muscle itself. These patients usually present with reduced levator action along with restricted extraocular motility and facial expression.
Myasthenia gravis
Myasthenia gravis is an autoimmune disorder characterized by the presence of antibodies to acetylcholine receptors located at the neuromuscular endplates of voluntary muscles.[3] This leads to decreased action of acetylcholine which results in muscle weakness and fatigue. Myasthenia may be generalized or localized to the eye (ocular myasthenia). The most common presenting feature is variable ptosis associated with diplopia. Symptoms may be unilateral or bilateral. Patients with myasthenia initially have a good levator function. Prolonged upgaze will cause a worsening of ptosis in these patients due to muscle fatigue.
Cogan lid twitch sign: Rapid saccadic eye movements from downgaze to primary position results in rapid upshoot of the lid followed by a gradual drop to the primary position.
Other tests which help confirm the diagnosis include ice test, serum acetylcholine receptor antibody assay, single fiber electromyography, and repetitive nerve stimulation test.
Treatment of such patients involves administration of acetylcholinesterase drugs, oral steroids or immunosuppressants. In patients with severe ptosis, ptosis correction with planned under-correction may be an option.
Myotonic dystrophy
Myotonic dystrophy is an autosomal dominant disorder which presents with gradually progressing ptosis and external ophthalmoplegia. The pathologic process is a failure of muscle to relax after contraction. It also involves muscles of facial expression, neck, and limbs.
Ocular examination in these patients also shows pupillary light-near dissociation, chromatic cataracts (Christmas tree cataract), and retinal pigmentary degeneration. Males develop a frontal pattern of balding and testicular atrophy.
Chronic progressive external ophthalmoplegia (CPEO)
CPEO is a mitochondrial myopathy causing bilateral symmetrical involvement of the extraocular muscles. Manifestations begin in childhood or adolescent age and progress slowly during adulthood. Bilateral symmetrical involvement is the first symptom followed by bilateral ophthalmoplegia. Due to the symmetric involvement of extraocular muscles, patients often do not complain of diplopia. As the muscles of facial expression are involved, patients develop an expressionless face (Hutchinson's face)
Diagnosis is confirmed by muscle biopsy which shows ragged red fibers due to enlarged mitochondria.
Kearns-Sayre syndrome: A variant of CPEO which shows retinal pigmentary degeneration, cardiac conduction defects, complete heart block, ataxia, neuropathy, endocrine dysfunction, and occurs in young adults.
There is no treatment to date for CPEO. Ptosis surgery to clear the visual axis can be done in severe cases keeping in mind the high risk of exposure keratopathy.
Oculopharyngeal muscular dystrophy
This autosomal dominant disorder manifests in the 4 to 5 decade of life with bilateral ptosis, progressive external ophthalmoplegia, dysphagia, dysarthria, facial muscle weakness, and proximal limb weakness.
Mechanical ptosis
Ptosis secondary to any tumor producing an increased weight on the lids, cicatrization or scarring of the conjunctiva, and blepharochalasis.
Traumatic ptosis
Ptosis occurs due to direct or indirect trauma to the levator muscle. Penetrating injuries involving the levator can be repaired immediately. However, ptosis secondary to blunt trauma may resolve spontaneously over time. Ptosis which does not improve after 6 months can have surgical repair.
Pseudoptosis
It is not true ptosis but apparent ptosis due to abnormalities in structures other than the levator muscle. Causes include dermatochalasis, brow ptosis, hypotropia, microphthalmos, anophthalmos, phthisis bulbi, and contralateral eyelid retraction.
It is very important to distinguish true ptosis from a pseudoptosis before embarking upon any surgical correction for drooping.
Clinical presentation
Patients usually complain of
- Drooping of eyelids
- Feeling of heaviness in the eyes
- Visual obscuration due to drooping
- Cosmetic complaints
Assessment
A thorough history taking and clinical examination help determine the etiology of ptosis and plan appropriate treatment.
History
History taking should include the age of onset of ptosis, progression, duration, and any aggravating or relieving factors. Any associated symptoms such as diplopia, diurnal variation, pain, lid swelling, dysphagia or muscle weakness help provide a provisional diagnosis.
Predisposing factors such as trauma, ocular or eyelid surgery, contact lens use, and botulinum toxin injection should be carefully ruled out. A family history of ptosis should be looked for to rule out hereditary disorders. In patients where the history is inconclusive, assessment of old photographs gives an idea about the time of onset.
Any systemic illness, mental health issues, and medication history require documentation. Patients on blood thinners such as aspirin should be advised to stop medications 1 week before surgery.
Clinical examination
Clinical examination starts from the moment the patient walks into the doctor's clinic. It is essential to look for any facial asymmetry, frontalis overaction, chin up or head tilt posture.
Ocular examination
- Visual acuity and refraction
- Cover test to look for any hypotropia and rule out any component of pseudoptosis
- Extraocular motility disturbance and any aberrant eyelid movements
- Pupillary examination to look for Horner syndrome or 3rd cranial nerve palsy
- Examination to look for any giant papillary conjunctivitis or symblepharon
- Corneal sensation and dry eye evaluation as they can predispose to post-operative keratopathy.
- Fundus examination for features of retinal pigmentary degeneration
Specific examination of ptosis
Lid measurements should be done positioning the face in the frontal plane, negating the action of frontalis muscle with the thumb, and eyes in the primary position of gaze. The examiner should be seated at the eye level of the patient to avoid parallax error.
1. Palpebral fissure height (PFH): It is the vertical palpebral aperture height between the upper and lower eyelid margin in the pupillary plane with eyes in the primary position of gaze. Average PFH is around 10mm.
2. Marginal reflex distance 1 (MRD 1): MRD 1 is the distance between the upper lid margin and the corneal light reflex. Normal MRD 1 is 4-5mm. The difference in MRD 1 between the two eyes helps classify ptosis as mild, moderate or severe in patients presenting with unilateral ptosis.
The difference in MRD 1 between two eyes:
- 2mm – Mild ptosis
- 3mm – Moderate ptosis
- 4mm – Severe ptosis
3. Marginal reflex distance 2 (MRD 2): MRD 2 is the distance between the corneal light reflex and lower eyelid margin. Normally MRD 1 + MRD 2 = PFH.
4. Levator action: It is the amount of excursion measured with a millimeter scale when the eyelid moves from extreme downgaze to extreme upgaze with frontalis action negated. Normal levator action is greater than 15mm. It is the single most important measurement in a patient with ptosis as its value determines the choice of surgical procedure.
Grading of levator action[4]
- Less than 4 mm – Poor
- 5 to 9 mm – Fair
- 9 to 11 mm – Good
- Greater than 12 mm – Excellent
In patients with poor levator action (less than 4mm), frontalis sling surgery is the preferred procedure.
5. Margin crease distance (MCD): It is the distance between the lid margin and skin crease in downgaze. Normal MCD is 7 to 8mm in men and 8 to 10 mm in women. In congenital ptosis, MCD is usually absent or faint, whereas in aponeurotic ptosis MCD is higher than normal.
During surgery, it is very important to reform the crease identical to the contralateral eye to maintain symmetry and achieve good cosmesis.
6. Bell’s phenomenon: This is another very important factor to be considered before ptosis correction. The patient is asked to close the eyes gently, and an attempt is made to open them. In patients with poor bell’s, ptosis correction should be avoided or undercorrected to avoid the risk of post-operative exposure keratopathy.
7. Assess presence of lagophthalmos and lid lag on downgaze which if present will worsen post-surgery.
8. Any brow ptosis or dermatochalasis if present should be documented. In involutional ptosis, blepharoplasty procedure is often combined with ptosis repair.
9. Hering test: In patients with unilateral ptosis, the ptotic lid is gently elevated manually, and the contralateral eyelid observed. Due to Hering's law of equal innervation, the contralateral eyelid may drop (See-saw effect). It is important to demonstrate this to the patient preoperatively and warn them about the possibility of requiring ptosis surgery in the contralateral eye. In such cases, a planned under-correction may be the treatment.
10. Phenylephrine test: It is a useful test in patients with mild ptosis or ptosis due to Horner syndrome; instill 2.5% phenylephrine drops in the superior fornix. Ptosis measurements are repeated after 10 minutes. Patients in whom the ptotic lid elevates due to stimulation of Muller's muscle are ideal candidates for posterior approach ptosis correction (conjunctival – mullerectomy surgery).
11. Tests to rule out myasthenia gravis:
Fatigue test: The patient maintains fixation in upgaze for 30 seconds. In patients with myasthenia, the eyelid gradually drops down due to muscle fatigue.
Ice test: An ice pack is placed over the closed ptotic eyelid for 2 minutes. Ptotic measurements are repeated after 2 minutes. Improvement in PFH by 2mm or more is considered positive for myasthenia. This is because cooling improves neuromuscular transmission.
12. Hertel exophthalmometry: A Hertel reading helps rule out any proptosis or enophthalmos and thus excludes pseudoptosis.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The opening located between the upper and lower eyelid is elliptical and termed the palpebral fissure. The upper eyelid curvature is maximum at a point just nasal to the mid pupillary point, which is an important point to mark before surgery to get the best cosmetic results. The upper lid covers 1 to 2mm of the superior limbus, while the lower lid lies at the lower limbus.
Structures forming the eyelid[5]
- Skin and subcutaneous tissue
- Orbicularis oculi
- Orbital septum
- Preaponeurotic fat pad
- Tarsal plate
- Levator aponeurosis and Muller’s muscle
- Conjunctiva
Skin
The eyelid skin is the thinnest layer of skin in the entire body. The eyelid crease forms due to attachment of levator aponeurosis to the skin.
Orbicularis oculi
It is a circular muscle and consists of three parts namely: preseptal, pretarsal, and orbital orbicularis. Contraction is responsible for gentle and forced closure of the eyelid.
Orbital septum
It is a multi-layered structure of thin fibrous connective tissue. The septum inserts superiorly to the periosteum over the superior orbital rim. Inferiorly it merges with the fibers of levator aponeurosis above the superior tarsal border.[5]
In ptosis surgery, the septum is opened to gain access to the levator muscle. Care should be taken to separate septal attachments to the levator muscle to avoid post-operative lid retraction.
Preaponeurotic fat pad
The fat pad is posterior to the septum and anterior to the levator. This pad of fat can be identified intraoperatively by applying pressure over the globe which causes it to prolapse forward. It helps in identifying the levator muscle which lies immediately posterior to it.
Tarsal plate
Tarsal plate forms the structural skeleton of the eyelid and is made up of dense connective tissue. The vertical height is 10 to 12 mm in the upper eyelid and 4 to 5 mm in the lower lid. The tarsal plates contain the Meibomian glands, the orifices of which open posterior to the grey line.
Levator Palpebrae superioris muscle (LPS)
LPS is the main elevator of the eyelid. It originates at the orbital apex from the periosteum over the lesser wing of sphenoid. It travels forward below the roof of the orbit. At the superior orbital rim, it changes direction from horizontal to vertical and forms the tendinous sheath called levator aponeurosis. At this transition, lies the Whitnall’s ligament which is seen as a dense white band of connective tissue and acts as a pulley. It lies 10 to 12 mm above the tarsal plate.
The levator aponeurosis has several insertions. Anteriorly, it inserts into the upper lid skin forming the lid crease. Inferiorly, it inserts onto the anterior surface of the superior one-third of the tarsus. Posteriorly, it has attachments to the superior conjunctival fornix. Medially and laterally, it forms the medial and lateral horns which then insert into the posterior lacrimal crest and Whitnall’s tubercle along with the canthal tendons.[6]
The levator receives nerve supply by the superior division of the oculomotor nerve.
Muller’s muscle
It is a sympathetically innervated smooth muscle. It originates from the under surface of the levator aponeurosis at the level of the Whitnall ligament and inserts into the superior border of the tarsus. It contributes to 2 mm of eyelid elevation.
Conjunctiva
It is the innermost layer of the eyelid formed by non-keratinizing squamous epithelium. It continues over the anterior surface of the globe. It contains goblet cells, the secretions of which hour of utmost importance in keeping the eyes moist.
Indications
Most patients undergoing ptosis correction seek surgery due to visual obscuration and loss of peripheral field of vision caused by the drooping eyelid. Heaviness in the eyelids is another common concern. A significant proportion seeks surgery for cosmetic concern as the drooping eyelid creates a tired-looking appearance.
Contraindications
- Severe dry eye
- Patients suffering from myogenic ptosis like chronic progressive external ophthalmoplegia - in these patients, if ptosis correction is planned, a conservative surgery should be the choice to clear the visual axis
- Poor Bell’s phenomenon
- Ptosis associated with oculomotor nerve palsy
- Myasthenia gravis: These patients should be treated medically first with anticholinesterase agents
Equipment
A basic oculoplasty instrument set, local anesthetic containing epinephrine, a skin marking pen and measuring scale is all that is needed to perform a successful ptosis surgery.
Preparation
A thorough pre-operative evaluation which includes a detailed history and meticulous clinical investigation helps improve the surgical success of ptosis surgery.
Patient counseling and consent
A patient should clear explanation about the goals of surgery, including the surgical technique used, incision size, and nature of postoperative scar. The surgeon should show the patient pre- and post-operative photographs of other patients, so they know what to expect. Patients undergoing a conservative approach should be shown in the clinic, the amount of lid lift. Patients need to understand about the possibility of overcorrection, under-correction, lid contour asymmetry, post-operative lagophthalmos, dry eyes, exposure keratopathy, wound infection, recurrence of drooping post-surgery and informed consent obtained.
Pre-operative photographs
Clinical photographs are taken with flash in the following gazes:
- Straight gaze
- Closed eyelids
- Downgaze
- Upgaze
- Oblique view
Pictures are then taken two months post-surgery in the same positions for comparison.
Technique or Treatment
A brief history of ptosis surgery:
Early treatments for ptosis involved excision of the excess skin on the upper eyelid. The earliest description of suspension of the eyelid to the brow with absorbable catgut sutures was made by Dransart in 1880. This was modified by Pagenstecher who suspended the eyelid skin to the brow with silk sutures. Wright (1922) and Crawford (1956) attempted the use of the fascia lata as a sling, by attaching it to the tarsal plate and anchoring it to the frontalis muscle.[7] Other autologous materials that were tried are palmaris tendon and temporalis fascia. Subsequently, nonabsorbable sutures have also been tried as a sling. Tillet and Tillet (1966) recommended the use of silicone rod slings.[8] They have claimed that the better elasticity provided by their modified silicone rods lead to a significant reduction in the lagophthalmos associated with ptosis.
Levator resection, initially carried out through the conjunctival route, was introduced by Bowman in 1857, and later developed by Blaskovics (1909). It was further improved by Berke and Illif. Berke (1959) is credited with evolving the levator function technique to decide the intraoperative lid height which is a useful guide during surgery.[9]
Everbush (1883) and Wolf (1896) popularized the anterior or skin approach for ptosis correction. In their opinion, it is a more efficient approach to the identification of the levator aponeurosis, and a larger area of the aponeurosis can be excised using this approach. Also, as the anatomy is easier to understand, it is easier to perform for novice surgeons.
Fasanella and Servat in 1961 described a simple vertical lid shortening procedure for correcting mild ptosis.[10] Putterman (1972) further improved the technique by excising the Müller’s muscle alone without damaging the tarsal plate.[11]
Correction of ptosis is essentially surgical with few exceptions. The techniques most commonly used in adult ptosis are Levator repair (Anterior approach) and Muller’s muscle-conjunctival resection (Posterior approach). Frontalis sling is seldom used in adult patients. However, it is the preferred technique for myogenic and neurogenic ptosis where the risk of exposure keratopathy is high and sling surgery can be easily reversed in such scenarios.
Levator Aponeurosis Advancement procedure
It is the procedure of choice for aponeurotic and involutional ptosis which is caused by dehiscence, disinsertion or thinning of the levator aponeurosis. The procedure can be combined with an upper eyelid blepharoplasty in patients with associated dermatochalasis.
Skin markings
The upper eyelid crease is marked prior to infiltration of local anesthetic in order to maintain symmetry between the two eyes. Skin markings should be done with the patient in sitting posture and eyes in primary gaze. In patients with a preexisting faint eyelid crease, the same crease can be marked. Patients with unilateral ptosis presenting with a raised or absent lid crease, markings are made based on the contralateral normal eyelid crease. However, in patients with bilateral ptosis, the lid crease is marked at 8-10mm along the papillary plane and tapered to 5-6mm medially and laterally.
Anesthesia
Local anesthetic infiltration is done with 2% lidocaine containing 1 to 100000 epinephrine. Epinephrine causes vasoconstriction and thus prevents the spread of the drug and helps in hemostasis. 1 to 1.5ml of local anesthetic is infiltrated along the skin marking. Excessive infiltration is avoided to prevent complete paralysis of the levator which makes it difficult to assess the lid position during surgery. Additional IV sedation with monitored anesthetic care can be given to reduce anxiety but over sedation should be avoided.
Surgical steps
Routine cleaning and draping of the face are done. It is important to keep both eyes exposed to assess the lid position during surgery.
Lid crease incision is made with a 15 blade. Unipolar cautery or CO2 laser can also be used to make the lid crease incision which helps in hemostasis.
Dissection is then done to open the orbicularis oculi muscle along the entire length of the incision which exposes the orbital septum below. Orbicularis oculi muscle if hypertrophied can be partially excised along the incision.
Dissection is done inferiorly in the sub orbicularis oculi plane to expose the upper part of the tarsal plate. Excessive dissection up to the lid margin is avoided as it causes post-operative lash ptosis.
The orbital septum is now opened. Orbital septum is identified by applying pressure gently over the globe which causes the pre-aponeurotic fat pad to bulge forward. The septum is carefully incised over the prolapsed fat using Westcott scissors and the dissection carried medially and laterally to open the entire septum. Care should be taken to open the septum slightly higher up on the lid to avoid any inadvertent damage to the aponeurosis below.
The preaponeurotic fat is gently separated from the underlying levator by blunt dissection and using cotton tip applicator. A Desmarre’s retractor is used to retract the fat, and all fibrous connections between the septum and levator must be released to avoid post-operative lid retraction.
The disinserted or dehisced aponeurosis is identified as a faint white line at the level where the septum fuses with the aponeurosis. In such cases, the muller’s muscle with the peripheral arterial arcade on its anterior surface can be seen above the superior border of the tarsal plate. In some patients, the aponeurosis may be thinned out or infiltrated with fat.
The levator is now advanced and re-attached to the upper one-third of the tarsus using a double-armed 5-0 vicryl or polyester suture.
A partial thickness suture is taken through the central part of the tarsus 2mm below the superior edge. The eyelid should be everted and checked to ensure that the suture has not passed through the entire thickness of the tarsus. This is important to avoid corneal abrasions. The suture is then passed through the disinserted edge or higher on the aponeurosis in a horizontal mattress fashion and a slip knot tied. The patient is asked to open eyes and lid position assessed both in the lying down and sitting posture. The level of suture placement on the aponeurosis may be increased or decreased to achieve the desired eyelid height and contour. Once the desired lid height is achieved the suture is tied and cut. Similar sutures are then passed medial and lateral to the central suture, lid contour and height assessed and permanent knots placed.
Eyelid crease forming sutures may be placed if required using two or three interrupted sutures using 6-0 ethilon which pass from the lower skin edge, a partial thickness bite is then taken through the levator aponeurosis and the needle is then passed through the upper skin edge and a permanent knot tied.
The wound is closed with interrupted 6-0 plain gut or ethilon sutures. Antibiotic ointment is applied over the wound. A temporary eye patch may be applied.
Post-operatively patient is advised to place ice compresses over the lids for the first 48 hours. Antibiotic ointment is applied over the wound and lubricating eye drops used frequently. Suture removal occurs 7 to 10 days post-operatively.
Muller’s muscle-conjunctival resection (MMCR)
This posterior approach technique is useful for patients presenting with mild ptosis and excellent levator function or ptosis secondary to Horner’s syndrome and anophthalmic socket. It is a modification of the Fasanella – Servat procedure where a bit of tarsus is removed along with conjunctiva and muller’s muscle. Prior to surgery, it is imperative to perform a 2.5% phenylephrine test and confirm elevation of the ptotic lid. If the ptotic lid elevates by 2mm, Dresner recommends 4mm of MMCR for every 1mm of ptosis correction.[12] However, this is variable and individualized based on each surgeon’s technique. Another prerequisite for surgery is to ensure adequacy of healthy conjunctiva in the superior fornix.
Anesthesia
The upper eyelid is everted and 1-2ml of 2% lidocaine containing 1:100000 epinephrine is infiltrated above the superior border of the tarsus to produce ballooning of the conjunctiva. An additional lid crease infiltration and IV sedation under monitored anesthetic care may be given.
Surgical steps
Routine cleaning and draping of the face are performed. Both eyes are kept exposed to assess the lid position during surgery.
Eyelid traction sutures are taken with 5-0 mersilk sutures. The upper eyelid is everted using Desmarres retractor and held in position by clamping the traction sutures to surgical drapes over the forehead.
The conjunctiva is dried with gauze and markings are made above the superior tarsal border. Another marking is made superior to the first marking at a distance which is equal to half the desired MMCR (For a patient who requires 2mm of ptosis correction an 8mm of MMCR is required. In this case the superior conjunctival marking is made at 4mm from the superior tarsal marking).
Three 6-0 silk sutures are passed through the superior conjunctival markings. The sutures are passes such that they incorporate only the conjunctiva and Muller's muscle. Traction is applied to the sutures which causes separation of the conjunctiva and muller’s from the underlying levator aponeurosis. The Desmarres retractor is removed.
A Putterman mullerectomy clamp is then placed at the base of the tented tissue ensuring that the tarsus is not incorporated in the clamp.
A double-armed 6-0 plain cut or vicryl suture is then passed in a running horizontal mattress fashion below the clamp from one end to the other.
The clamped conjunctiva and Muller’s are then resected using a 15 blade, and the tissues cut using metal on metal contact between the blade and Putterman clamp.
The suture is then passed in the reverse direction from one end of the wound to the other in a running horizontal mattress fashion and a knot tied. Another technique is to pass the suture ends from the conjunctival side through the full thickness of the eyelid and exit on the skin side and secured. In such cases, suture removal occurs after 1 week.
Post-operatively patient is advised to place ice compresses over the lids for the first 48 hours. The patient should apply antibiotic ointment at bedtime for a week, and lubricating eye drops used frequently.
Frontalis sling surgery
Frontalis sling is commonly performed in patients with severe ptosis and poor levator action (less than 4mm). This procedure is often used in adults with myasthenia gravis, chronic progressive external ophthalmoplegia, IIIrd nerve palsies and other conditions that lead to a very weak levator function. It is the procedure of choice in severe congenital ptosis with poor levator action, but other indications for sling surgery include myogenic ptosis, neurogenic ptosis, blepharophimosis syndrome, and Marcus Gunn jaw-winking syndrome.
The frontalis muscle contributes about 2 to 3 mm of eyelid elevation. This action is utilized in frontalis sling surgery where the eyelid is suspended to the frontalis muscle to achieve eyelid elevation. Various materials are used for suspension which may be autogenous, allogenic or synthetic.
Autogenous materials include fascia lata, palmaris longus tendon, and temporalis fascia. Allogenic material consists of banked fascia lata. Synthetic materials include polypropylene (prolene), supramid nylon suture, mersilene mesh, and silicone.[13]
Among these, the most widely used are silicone rod and fascia lata with the latter being the gold standard material of choice.
There are two techniques of frontalis sling: Crawford technique and Fox pentagon. The Fox pentagon with fewer stab incisions is faster and easier to perform and is the technique most commonly followed.
Skin markings (Fox pentagon method)
It consists of 5 small incisions. Two eyelid markings are made 2mm from the lid margin at the medial and lateral limbus. These markings can be adjusted to get a good contour which can be determined using a forceps to raise the lids. Two eyebrow markings are made just above the eyebrows corresponding to the medial and lateral canthus. A central forehead incision is made in the pupillary plane slightly higher than the eyebrow markings.
Anesthesia
General anesthesia is the preferred choice for children; however, local anesthesia with intravenous sedation is better for adults. Local anesthetic infiltration is with 2% lidocaine containing 1 to 100000 epinephrine. The local anesthetic infiltrates along the skin marking, and pressure applied.
Surgical steps
Routine cleaning and draping of the face are p. Both eyes remain exposed to assess the lid position during surgery. The forehead is also kept exposed to pass the sling.
Stab incisions are made through the skin markings. The central forehead incision is widened to 3 to 5mm.
The sling loaded on a needle is passed from the central forehead incision and brought out through the medial eyebrow incision engaging the frontalis muscle. It is then passed from the medial eyebrow incision to the medial eyelid incision passing deep to the orbicularis oculi but anterior to the orbital septum and tarsal plate.
Next, it is passed from the medial to the lateral eyelid incision. Here the sling lies superficial to the tarsus. Care is necessary to avoid globe injury. This can be achieved by using a lid guard.
The sling is now passed in the reverse direction from the lateral eyelid incision to the lateral eyebrow and subsequently out through the central forehead incision. The lid height is now adjusted on the table and when the desired contour is achieved the sling is secured with a silicone sleeve and the excess sling material cut. The sling with the sleeve is then buried in a pocket created. The incisions are then sutured with 6-0 plain gut.
Frost suture may be taken through the lower eyelid to protect the cornea in the immediate post-operative period.
Post-operatively patient is advised to place ice compresses over the lids for the first 48 hours. The patient should apply antibiotic ointment at bedtime for a week, and lubricating eye drops used frequently. Frost suture removal is performed after 48 hours.
Complications
Undercorrection
This phenomenon may occur with any technique. In the immediate post-operative period, the lid appears undercorrected due to the lid edema. Patients may be reassured. However, if the under-correction persists then revision surgery may be required. The wound can be reopened and aponeurosis re-advanced.
Overcorrection
Overcorrection is more often encountered following advancement for aponeurotic/involutional ptosis. Mild overcorrection in the immediate postoperative period may be tackled with eyelid traction. The patient may be asked to look downward and pull on the eyelashes with the thumb and forefinger; this may be done for a few minutes 3 to 4 times a day. Severe overcorrection will require immediate revision. The wound can be reopened and the sutures cut. The levator is then placed at a more recessed position or secured to the tarsal plate using hang back sutures.
Lagophthalmos and exposure keratopathy
All patients are counseled pre-operatively about post-operative lagophthalmos and decreased blink rate. Management of lagophthalmos in the immediate post-operative period is with copious lubricants. A temporary frost suture may be applied. In cases where severe exposure keratopathy develops a revision surgery is done to lower the lid height.
Eyelid contour defects
Contour defects occur due to improper placement of sutures on the tarsus. Patients presenting with small contour defects usually settle down with time. Lid massage and eyelid traction exercises are advised. Persistent or severe contour abnormalities require revision surgery and proper placement of sutures on the tarsus.
Conjunctival prolapse
Extensive dissection between the conjunctiva and levator can disrupt the suspensory ligaments of the superior fornix and produce conjunctival prolapse. Mild prolapse can be treated conservatively with lubricants. Severe prolapse requires repositioning of the conjunctiva with pang sutures; suture is passed through the prolapsed conjunctiva and secured at the skin crease.
Eyelash ptosis
Excessive dissection of the orbicularis from the tarsus results in lash ptosis, which can be corrected by anterior lamella repositioning sutures.
Suture granuloma
Small granulomas can form at the suture site. They can be excised with Wescott scissors and the base cauterized. The suture causing the granuloma also requires removal.
Clinical Significance
Ptosis correction helps restore the field of vision and also improves the aesthetic appearance; it reverses the feeling of heaviness in the eye. Most patients feel and look younger thus improving their quality of life.
Enhancing Healthcare Team Outcomes
Adult ptosis is a common condition encountered in ophthalmic clinics by the ophthalmic nurse, optician, and the ophthalmologist. THese interprofessional entities need to collaborate in a team approach to patient care in ptosis cases. Oculoplastic and plastic surgeons perform ptosis correction. Practicing surgeons should be aware of the anatomy, etiology, examination and surgical techniques for ptosis correction. Surgeons should be well aware of what surgery to perform when and also when not to operate.
Media
(Click Image to Enlarge)
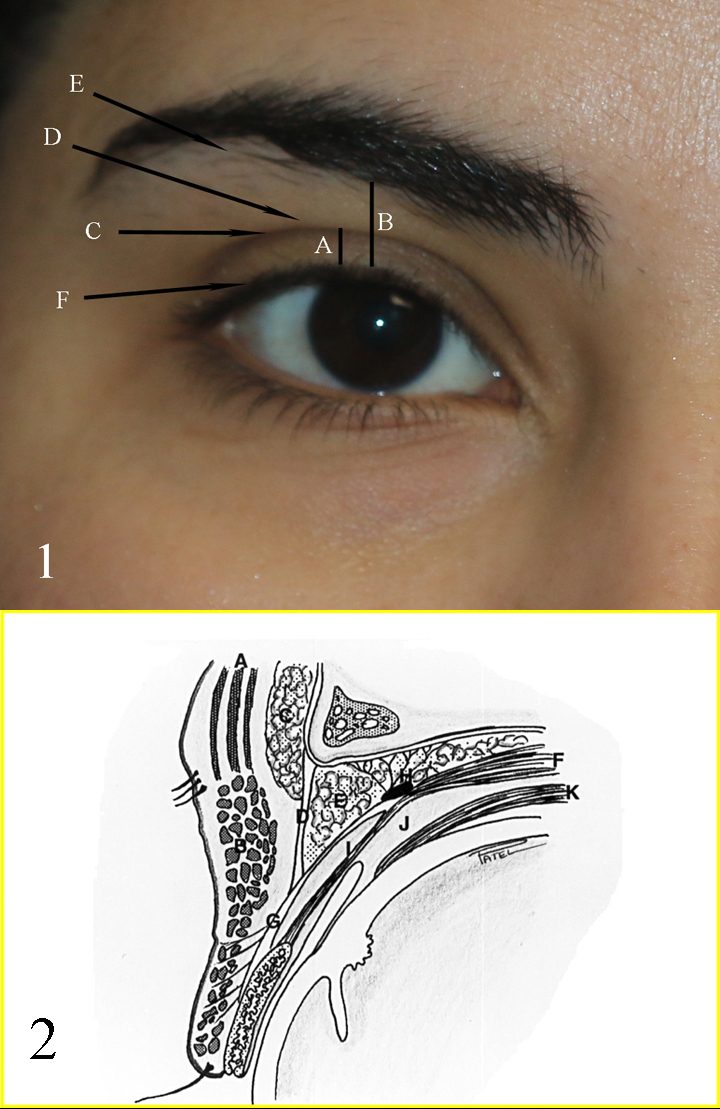
Fig 1: A: upper eyelid platform; B: Brow to Lid margin distance; C: Upper eyelid crease; D: Upper eyelid fold; E: Brow fatpad; F: Eyelid margin and eyelash curve Fig 2: A: Frontalis muscle; B: Orbicularis muscle; C: Brow fat pad; D: Orbital septum; E: Preaponeurotic fat pads; F: Levator muscle; G: Levator aponeurosis; H: Whitnall ligament; I: Muller muscle; J: Common sheath; K: Superior rectus muscle Contributed by Professor Bhupendra C. K. Patel MD, FRCS
(Click Image to Enlarge)

Normal eyelids in a young white woman. Note that the skin creases are not exactly symmetrical, which is normal. Note also that the maximal height of the upper eyelid is just medial to the center of the pupil, but if the patient is converging, it may seem more lateral. Note the fullness just above the upper eyelid crease, which creates a fold and a fullness in the upper lids and below the brows, which gives the youthful appearance. Contributed by Professor Bhupendra C. K. Patel MD, FRCS
(Click Video to Play)
References
Finsterer J. Ptosis: causes, presentation, and management. Aesthetic plastic surgery. 2003 May-Jun:27(3):193-204 [PubMed PMID: 12925861]
Dortzbach RK, Sutula FC. Involutional blepharoptosis. A histopathological study. Archives of ophthalmology (Chicago, Ill. : 1960). 1980 Nov:98(11):2045-9 [PubMed PMID: 7436841]
Elrod RD, Weinberg DA. Ocular myasthenia gravis. Ophthalmology clinics of North America. 2004 Sep:17(3):275-309; v [PubMed PMID: 15337189]
Anderson RL, Dixon RS. Aponeurotic ptosis surgery. Archives of ophthalmology (Chicago, Ill. : 1960). 1979 Jun:97(6):1123-8 [PubMed PMID: 375893]
Level 3 (low-level) evidenceKakizaki H, Malhotra R, Selva D. Upper eyelid anatomy: an update. Annals of plastic surgery. 2009 Sep:63(3):336-43. doi: 10.1097/SAP.0b013e31818b42f7. Epub [PubMed PMID: 19602949]
Ng SK, Chan W, Marcet MM, Kakizaki H, Selva D. Levator palpebrae superioris: an anatomical update. Orbit (Amsterdam, Netherlands). 2013 Feb:32(1):76-84. doi: 10.3109/01676830.2012.736602. Epub [PubMed PMID: 23387464]
CRAWFORD JS. Repair of ptosis using frontalis muscle and fascia lata. Transactions - American Academy of Ophthalmology and Otolaryngology. American Academy of Ophthalmology and Otolaryngology. 1956 Sep-Oct:60(5):672-8 [PubMed PMID: 13380883]
Tillett CW, Tillett GM. Silicone sling in the correction of ptosis. American journal of ophthalmology. 1966 Sep:62(3):521-3 [PubMed PMID: 5331721]
BERKE RN. Results of resection of the levator muscle through a skin incision in congenital ptosis. A.M.A. archives of ophthalmology. 1959 Feb:61(2):177-201 [PubMed PMID: 13616781]
FASANELLA RM, SERVAT J. Levator resection for minimal ptosis: another simplified operation. Archives of ophthalmology (Chicago, Ill. : 1960). 1961 Apr:65():493-6 [PubMed PMID: 13698293]
Putterman AM, Urist MJ. Müller muscle-conjunctiva resection. Technique for treatment of blepharoptosis. Archives of ophthalmology (Chicago, Ill. : 1960). 1975 Aug:93(8):619-23 [PubMed PMID: 1156223]
Dresner SC. Further modifications of the Müller's muscle-conjunctival resection procedure for blepharoptosis. Ophthalmic plastic and reconstructive surgery. 1991:7(2):114-22 [PubMed PMID: 1863563]
Takahashi Y, Leibovitch I, Kakizaki H. Frontalis suspension surgery in upper eyelid blepharoptosis. The open ophthalmology journal. 2010 Dec 14:4():91-7. doi: 10.2174/1874364101004010091. Epub 2010 Dec 14 [PubMed PMID: 21331314]