Anatomy, Shoulder and Upper Limb, Median Nerve
Anatomy, Shoulder and Upper Limb, Median Nerve
Introduction
The innervation of the upper limb is divided into anterior (ventral) divisions that supply the anterior muscles (such as biceps brachii, brachialis, pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis and profundus, and pronator quadratus). These muscles are innervated by C5-T1 spinal nerves.
The spinal cord is divided into white columns (myelinated axons) and gray horns (cell bodies of motor neurons). The sensory neurons have their cell bodies in the posterior (dorsal) root ganglia. They have a peripheral process that innervates the organs of sensation in the skin and a central process that connects the posterior root ganglia to the spinal cord posterior (dorsal) columns for sensory function. The cell bodies for motor function lie in the anterior (ventral) gray horns. The posterior roots serve sensation. The anterior roots are motor in function. The posterior and anterior roots join to form the mixed spinal nerve. Those that serve the upper limb are derived from spinal cord segments C5-T1. The entirety of the spinal cord gives off eight cervical, twelve thoracic, five lumbar, five sacral, and one coccygeal mixed spinal nerve.
The mixed spinal nerves join to form the brachial plexus (Latin brachium = arm). The mixed spinal nerves give off posterior and anterior branches. The anterior branches from C5-T1 are termed roots of the brachial plexus. Those from C5 and C6 join to form the superior trunk. Those from C7 form the middle trunk. Those from C8 and T1 form the superior trunk. The posterior nerves are involved in the innervation of the paraspinal muscles.
Each trunk then divides into anterior and posterior divisions. The anterior divisions from C5, C6, and C7 join to form the lateral cord. Those from the anterior divisions of C8 and T1 form the medial cord. The posterior divisions of C5-T1 join to form the posterior cord.
The median nerve is one of the five terminal divisions of the brachial plexus. The convergence of the lateral and the medial cords form this nerve, and it has contributions from all anterior rami of C5-T1.[1][2][3][4]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The median nerve predominantly provides motor innervation to the flexor muscles of the forearm and hand. The median nerve also provides sensory innervation to the dorsal aspect (nail bed) of the distal first two digits of the hand, the palmar aspect of the thumb, index, middle, and half of the ring finger, the palm, as well as the medial aspect of the forearm.
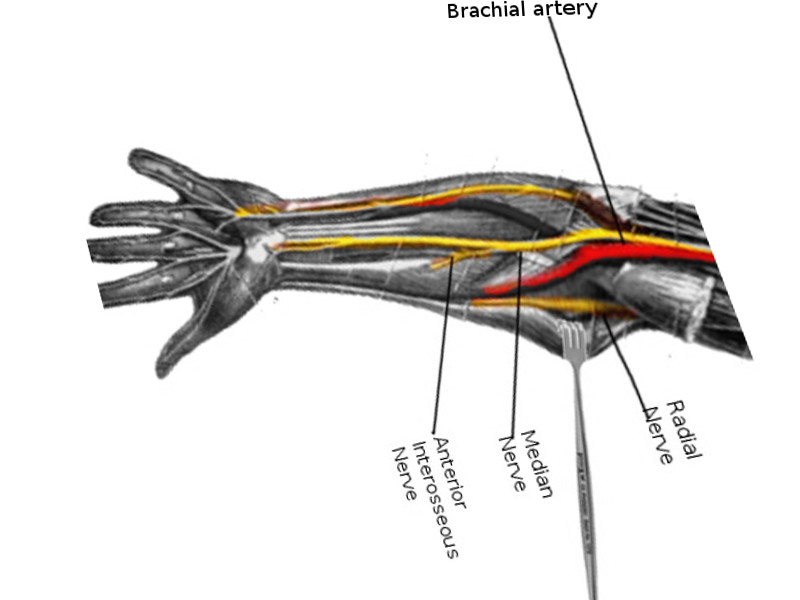
Nerves
After the convergence of the lateral and medial cords within the axilla, the median nerve travels distally along the median bicipital groove in a neurovascular bundle with the brachial artery. As it descends on the arm, it travels over the brachial artery and then under the bicipital aponeurosis (a sheath of connective tissue that inserts the biceps brachii to the proximal forearm), creating the cubital fossa. Above this point, the median nerve provides no muscular or cutaneous innervation. It does, however, provide sympathetic innervation to the brachial artery and its more distal branches (radial and ulnar arteries).[3][5][6]
At the level of the elbow, as the median nerve courses under the bicipital aponeurosis, it provides innervation to several proximal muscle bellies of the forearm, including the pronator teres, flexor carpi radialis, flexor digitorum superficialis (sublimis), and palmaris longus muscles. As the nerve emerges from the bicipital aponeurosis, it passes through the convergence point of the superficial and deep heads of the pronator teres. Compression at this point can lead to pronator syndrome, described below. The median nerve makes its final pass underneath the sublime ridge, a sheath of connective tissue formed by the convergence of the medial and lateral heads of the flexor digitorum superficialis (sublimis) (FDS), before emerging to give off two branches, the anterior interosseous nerve and the median nerve proper.
As the median nerve proper descends the forearm, it travels deep to the flexor digitorum superficialis but superficial to the flexor digitorum profundus (FDP). The anterior interosseous nerve (AIN) passes deeper than the median nerve proper, just anterior to the interosseous membrane. In the forearm, the median nerve proper supplies innervation to the pronator teres, palmaris longus, and the flexor digitorum superficialis, However, the AIN provides innervation to the FDP, flexor pollicis longus, and pronator quadratus. By the end of its course in the forearm, the median nerve and all of its branches innervate all of the flexor muscles of the forearm except for the ulnar half of the flexor digitorum profundus and the flexor carpi ulnaris.
Approximately 5 cm above the flexor retinaculum,
the muscle belly of the FDS ends and becomes a tendinous sheath, and the median nerve anatomically lies between this tendon and that of the flexor carpi radialis just before diving into the carpal tunnel. At a variable point before the wrist, the median nerve gives off the palmar cutaneous branch, which passes over the flexor retinaculum and strictly provides sensory innervation to the palm and the base of the thenar eminence.
At its narrowest, the carpal tunnel’s cross-sectional area is less than 2 square centimeters. The median nerve passes directly beneath the flexor retinaculum sheath alongside nine other muscular tendons. This high-traffic area is a prime spot for compression, and in fact, of all the entrapment neuropathies, carpal tunnel syndrome (described below) has been reported to be the most common.
After emerging from the carpal tunnel, the median nerve transverses below the palmar aponeurosis and immediately gives off the thenar recurrent motor branch, which supplies the thenar muscles of the hand: flexor pollicis brevis, abductor pollicis brevis, and opponens pollicis. The last contribution of the median nerve to the thumb is from the anterior interosseous nerve, which travels outside of the carpal tunnel and supplies the flexor pollicis longus.
At the palmar aponeurosis, the median nerve splits into radial and ulnar divisions, which further separate into the common palmar digital branches. These digital branches innervate the first two lumbrical muscles and provide sensation to the palmar side of the thumb, index finger, middle finger, and the radial half of the ring finger. The median nerve also exclusively supplies sensory innervation to the dorsal surface of the index and middle fingers and the lateral half of the ring finger past the proximal interphalangeal joint (i.e., over the nailbeds).
Muscles
The muscles innervated by the median nerve can be divided into four layers of the anterior compartment of the forearm. The first layer arises from the medial epicondyle and contains three muscles: the pronator teres, flexor radialis longus, and palmaris longus. The second layer contains the flexor digitorum superficialis, whose tendons insert into the middle phalanx of the four fingers. Thus it is a flexor of the fingers at the proximal interphalangeal joint. The first and second layers are innervated by the median nerve proper.
The muscles of the third layer are the lateral half of the flexor digitorum profundus that innervates the index and ring fingers, the flexor pollicis longus, and the pronator quadratus. These are innervated by the anterior interosseous nerve, which has no sensory branches.
Sensory innervation: None of the sensory nerves that serve the forearm crosses the wrist (with the exception of the palmar branch of the median nerve). The sensory distribution of the median nerve in the hand consists of the palmar surfaces of part of the thumb, the index finger, the middle finger, and the lateral half of the ring finger. The rest of the sensory innervation of the hand is provided by the ulnar nerve (medial hand and medial half of the ring finger and all the little finger). The ulnar nerve also provides sensation to the medial dorsal surface through the dorsal branch of the ulnar nerve. The superficial branch of the radial nerve completes the innervation of the dorsal surface of the hand by way of the superficial branch of the radial nerve.
Surgical Considerations
A Monteggia Fracture (radial head dislocation with a concurrent proximal ulna fracture) places the anterior interosseous branch of the median nerve at risk over the site of the ulna fracture, where it can be stretched or compressed, resulting in traction or compression neuropathy. Posterior interosseous nerve palsy is also possible secondary to entrapment, stretching, scarring, displacement, or direct trauma. Open reduction and internal fixation of the ulna fracture will concurrently reduce the stress on the nerve and have been associated with a return to baseline function of the nerve.[7][8]
Carpal tunnel syndrome is a common pathology of the median nerve as it passes beneath the narrow flexor retinaculum (transverse carpal ligament) of the wrist. Overuse of the tendons can lead to inflammation and compression of the median nerve as it passes through, causing significant pain and weakness in the affected hand. Numbness and/or pain will be present in the first three and a half digits of the affected hand, and typically this is worse at night. Weakness is usually present in the thenar eminence if severe. Lifestyle risk factors for the development of carpal tunnel syndrome include repetitive tasks (such as typing, computer work, or writing), weight gain, pregnancy, and overuse of the hands (mechanics, carpenters, cashiers). Hypothyroidism, diabetes, arthritis, or previous injury can also predispose to carpal tunnel syndrome. Conservative measures of treatment include bracing, splinting, occupational therapy, and over-the-counter (OTC) anti-inflammatory medications. If these fail to resolve symptoms, surgical intervention with a carpal tunnel release may be warranted.[9]
Pronator syndrome is a median nerve compression injury similar to carpal tunnel syndrome. However, the pain is localized to the anterior proximal forearm due to compression of the nerve by the muscle bellies of the pronator teres muscle. Patients will complain of paresthesia in the distribution of the median nerve. However, there will also be numbness over the palm. The risk factors for pronator syndrome are similar to those of carpal tunnel syndrome (repetitive tasks). However, there has not been substantial literature to support surgical decompression to provide symptomatic relief. Most patients (50% to 70%) will recover with conservative therapy, including rest, ice, immobilization, nonsteroidal anti-inflammatory medications, and occupational therapy.[10]
Clinical Significance
Median neuropathies can be divided into proximal (high) and distal (low) median neuropathies.
High Median Neuropathy[11][12]
On physical exam, inspect the thenar eminence for atrophy. Assess light touch sensation over the lateral three and one-half digits. The pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis are innervated directly by the median nerve proper. Lesions of these muscles will result in weakness in pronation (pronator teres) and significant weakness in flexion of the forearm at the elbow (flexor carpi radialis and flexor digitorum superficialis). One can hold the patient's hand and test the ability to flex the fingers. Because the flexor digitorum superficialis tendons insert onto the sides of the fingers, weakness in the ability to flex the fingers at the proximal interphalangeal joint will occur in a high median neuropathy.
The anterior interosseous branch can be tested by asking the patient to make the “okay” sign with the thumb and index finger. A pinch instead of a circle indicates an anterior interosseous nerve palsy. Additionally, asking the patient to place the hand flat on the bed and then ask the patient to raise the thumb off the bed is a way to assess the distal aspects of the nerve by assessing both the opposition and abduction of the thumb. This is part of the findings in a high median neuropathy.[13][14][15][16]
If there is suspicion for median nerve pathology above the level of the elbow, ask the patient to make a fist. If there is a lesion at this level, then the flexor digitorum superficialis (FDS) function will be affected, resulting in impairment of flexion of all four fingers at the proximal interphalangeal joint. Loss of the anterior interosseus nerve will cause loss of flexion at the distal interphalangeal joint of the index and middle digits. When attempting to make a fist, the index and middle fingers will remain extended. This is commonly referred to as the “hand of benediction” or "preacher's hand." However, in clinical practice, an anatomic variation of the ulnar nerve typically allows flexion of the middle finger at the proximal interphalangeal (PIP) joint, and therefore a “pointer finger” (pointing with the index finger) is a more appropriate description of the observed finding. This is part of a high median neuropathy.
A supracondylar humeral fracture can damage the entire nerve, resulting in high median neuropathy.
Median nerve injury at the elbow or forearm can cause a single-palmar crease appearance due to the combined inability to flex the index finger and distal phalanx of the thumb, weak flexion of the middle finger, and defective opposition of the thumb. This is part of a high median neuropathy.
Low Median Neuropathy
Low median neuropathies consist of carpal tunnel syndrome, which has been discussed above, and median recurrent neuropathy. Lesion of the recurrent branch of the median nerve denervates the flexor pollicis brevis, opponens pollicis, and abductor pollicis brevis. The recurrent branch of the median nerve is located rather superficially at about the middle of the thenar muscle mass. Dishwashers washing dishes may damage the recurrent branch of the median nerve with a superficial cut, typically on a knife or a piece of broken glass. An unsuspecting emergency room physician may examine sensory function over the hand and note no loss of sensation. He may then use a piece of surgical tape or place a stitch to close the wound. The patient will return weeks later because of loss of motor function to the thumb and severe thenar muscle atrophy. This is medical malpractice because the physician did not realize that the recurrent branch of the median nerve has no sensory function. It is mandatory in the physical examination of such a patient to have the patient touch the pads of the thumb and little finger together in performing the opposition test. If the patient were asked to do so, he would have been unable to oppose the thumb. it would immediately have been obvious that he had suffered a median recurrent neuropathy.
Loss of innervation to the thumb causes the loss of the muscle mass of the thumb. This is sometimes termed the “ape hand” (even though most apes have opposable thumbs).
At the elbow, the median nerve lies medial to the brachial artery. If one needs to sample arterial blood gas levels by arterial puncture, it is common to use the radial artery due to its easy availability. However, one should perform the Allen test to determine whether the anastomosis between the radial artery and ulnar artery is sufficient for the ulna artery to supply blood to the thumb and index finger because the puncture may cause thrombosis of the radial artery. If the Allen test demonstrates inadequate perfusion by the radial artery, then the brachial artery can be sampled. The anatomical position of the radial artery to the median nerve now becomes of paramount concern in order to avoid damaging the median nerve. One first obtains a good localization of the radial artery with a pulse if possible. Sonography can yield superior results and should be used if available. It is then critical not to puncture the area medial to the brachial artery to avoid damaging the median nerve.
Injection nerve palsy is an iatrogenic condition caused when an intramuscular injection is placed in proximity to, or directly into, a nerve, thereby leading to axonal and myelin degeneration. The agent can penetrate the endoneurium, resulting in edema in the space surrounding an individual nerve fiber, ultimately leading to nerve damage and even nerve death. This will be extremely painful for the patient, and motor function will typically be more severely affected than sensory function. The most toxic agents are thought to be: penicillin, chlorpromazine, meperidine, dimenhydrinate, tetanus toxoid, procaine, and hydrocortisone.[17]
Other Issues
The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
I am a military service member. This work was prepared as part of my official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a United States Government work as a work prepared by a military service member or employee of the United States Government as part of that person’s official duties.
Media
(Click Image to Enlarge)
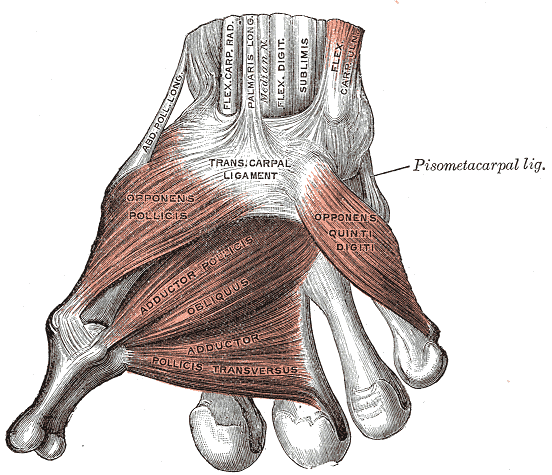
Muscles of the Thumb, Ligaments of the Wrist, Abductor pollicis longus, Flexor Carpal Radialis, Palmaris Longus, Median Nerve, Flexor Digitorum sublimis, Flex Carpal ulnaris, Transcarpal Ligament, Opponens Pollicis, Adductor Pollicis obliques, Adductor pollicis transversus, Opponens quinti digiti
Henry Vandyke Carter, Public domain, via Wikimedia Commons
References
Wertheimer A, Kiel J. Anatomy, Shoulder and Upper Limb, Forearm Anterior Interosseous Nerve. StatPearls. 2025 Jan:(): [PubMed PMID: 30335313]
Bains KNS, Lappin SL. Anatomy, Shoulder and Upper Limb, Elbow Cubital Fossa. StatPearls. 2025 Jan:(): [PubMed PMID: 29083694]
Seiler JG 3rd, Daruwalla JH, Payne SH, Faucher GK. Normal Palmar Anatomy and Variations That Impact Median Nerve Decompression. The Journal of the American Academy of Orthopaedic Surgeons. 2017 Sep:25(9):e194-e203. doi: 10.5435/JAAOS-D-16-00038. Epub [PubMed PMID: 28837460]
Raza K, Singh S, Rani N, Mishra R, Mehta K, Kaler S. Anomalous Innervation of the Median Nerve in the Arm in the Absence of the Musculocutaneous Nerve. Sultan Qaboos University medical journal. 2017 Feb:17(1):e106-e108. doi: 10.18295/squmj.2016.17.01.019. Epub 2017 Mar 30 [PubMed PMID: 28417038]
Doughty CT, Bowley MP. Entrapment Neuropathies of the Upper Extremity. The Medical clinics of North America. 2019 Mar:103(2):357-370. doi: 10.1016/j.mcna.2018.10.012. Epub [PubMed PMID: 30704687]
Ram S. "Carpal tunnel syndrome:" A bibliometric study of 35 years of research. Neurology India. 2019 Jan-Feb:67(Supplement):S55-S61. doi: 10.4103/0028-3886.250698. Epub [PubMed PMID: 30688235]
Zaremski JL, Wright TW, Herman DC. Humeral Stress Fracture With Median Nerve Injury in a Baseball Player: A Case Report and Discussion. Current sports medicine reports. 2018 Jun:17(6):183-186. doi: 10.1249/JSR.0000000000000489. Epub [PubMed PMID: 29889146]
Level 3 (low-level) evidenceVaquero-Picado A, González-Morán G, Moraleda L. Management of supracondylar fractures of the humerus in children. EFORT open reviews. 2018 Oct:3(10):526-540. doi: 10.1302/2058-5241.3.170049. Epub 2018 Oct 1 [PubMed PMID: 30662761]
Kortlever JTP, Becker SJE, Zhao M, Ring D. Borderline Nerve Conduction Velocities for Median Neuropathy at the Carpal Tunnel. The Journal of hand surgery. 2020 May:45(5):379-388.e1. doi: 10.1016/j.jhsa.2019.11.020. Epub 2020 Feb 20 [PubMed PMID: 32089378]
Dididze M, Tafti D, Sherman AL. Pronator Teres Syndrome. StatPearls. 2025 Jan:(): [PubMed PMID: 30252346]
Isaacs J, Ugwu-Oju O. High Median Nerve Injuries. Hand clinics. 2016 Aug:32(3):339-48. doi: 10.1016/j.hcl.2016.03.004. Epub 2016 May 2 [PubMed PMID: 27387077]
Morimoto D, Isu T, Kim K, Sugawara A, Isobe M, Morita A. Proximal Entrapment Neuropathy of the Median Nerve above the Elbow-Case Report. Journal of Nippon Medical School = Nippon Ika Daigaku zasshi. 2015:82(6):287-9. doi: 10.1272/jnms.82.287. Epub [PubMed PMID: 26823032]
Level 3 (low-level) evidenceKowalska B, Sudoł-Szopińska I. Ultrasound assessment on selected peripheral nerve pathologies. Part I: Entrapment neuropathies of the upper limb - excluding carpal tunnel syndrome. Journal of ultrasonography. 2012 Sep:12(50):307-18. doi: 10.15557/JoU.2012.0016. Epub 2012 Sep 30 [PubMed PMID: 26674101]
Keiner D, Tschabitscher M, Welschehold S, Oertel J. Anterior interosseous nerve compression syndrome: is there a role for endoscopy? Acta neurochirurgica. 2011 Nov:153(11):2225-9. doi: 10.1007/s00701-011-1091-5. Epub 2011 Jul 23 [PubMed PMID: 21786008]
Level 3 (low-level) evidenceLeclère FM, Bignion D, Franz T, Mathys L, Vögelin E. Endoscopically assisted nerve decompression of rare nerve compression syndromes at the upper extremity. Archives of orthopaedic and trauma surgery. 2013 Apr:133(4):575-82. doi: 10.1007/s00402-012-1668-3. Epub 2013 Feb 17 [PubMed PMID: 23417113]
Level 2 (mid-level) evidenceStrohl AB, Zelouf DS. Ulnar Tunnel Syndrome, Radial Tunnel Syndrome, Anterior Interosseous Nerve Syndrome, and Pronator Syndrome. The Journal of the American Academy of Orthopaedic Surgeons. 2017 Jan:25(1):e1-e10. doi: 10.5435/JAAOS-D-16-00010. Epub [PubMed PMID: 27902538]
Sriwong PT, Sirasaporn P, Foochareon C, Srichompoo K. Median neuropathy at the wrist in patients with systemic sclerosis: two-year follow-up study. Reumatologia. 2018:56(5):294-300. doi: 10.5114/reum.2018.79500. Epub 2018 Oct 31 [PubMed PMID: 30505011]