 Sonography Fetal Assessment, Protocols, and Interpretation
Sonography Fetal Assessment, Protocols, and Interpretation
Introduction
Fetal ultrasonography is an essential element in the evaluation of anomalies and fetal well-being throughout pregnancy. The increasing incidence of morbid obesity, hypertension, and gestational diabetes within the reproductive age group places this high-risk population at increased adverse fetal events such as stillbirth and fetal anomalies. In every trimester, there are specific maternal and fetal indications that require additional fetal screening and assessment. [1]
Each fetal scan has been standardized to include the minimal imaging criteria and components required by the society guidelines of American College of Radiology (ACR), Society of Radiologists in Ultrasound (SRU), American College of Obstetrics and Gynecology (ACOG), and American Institute of Ultrasound in Medicine (AIUM), in support by Society of Maternal-Fetal Medicine (SMFM). Although the ultrasound components are standardized, the terminology for the ultrasounds often differs between societies and the Current Procedural Terminology (CPT) descriptions, leading to a long history of misunderstanding amongst clinicians and missed opportunities for fetal assessment. [2]
The above-aforementioned societies agree on the classification of fetal ultrasounds as either standard, specialized, or limited examinations to try and mitigate the ongoing confusion. The standard, specialized, and limited ultrasound criteria can be applied to each trimester. Each examination has specific indications based on the trimester, which must be met before performing the exam. [2][1]
The standard second-trimester scan, also known as a “level I,” is a simple fetal anatomic survey examination performed in low-risk pregnancies. The specialized second-trimester anatomy ultrasound, also known as “level II,” “detailed,” or “targeted” examination, is performed when abnormalities are suspected on the standard anatomy examination or in pregnancies at high risk for anatomic abnormalities. Other types of specialized examinations include a fetal echocardiogram, fetal doppler ultrasound, cervical length measurement, and biophysical profile. Finally, a limited ultrasound is performed to answer a specific clinical question in any trimester that may aid in the diagnosis and treatment. A limited ultrasound is usually performed in an acute setting when time is restricted or a follow-up to assess specific fetal components.[2][1]
Fetal ultrasonography is a standard and routine modality performed in every pregnancy. However, the differences in approach, assessment protocols, timing, and frequency of the examinations are individualized based on the gestational age and clinical scenario. The goal of more frequent examinations in the high-risk population is to detect abnormalities in the early stage when further intervention may still be feasible. Traditionally, a comprehensive fetal anatomic survey has been performed in the mid-second trimester to assess anatomic anomalies. Owning to improvement and advancement in ultrasonography, abnormalities can now be detected in the late first trimester. Early identification of fetal anomalies allows the patient to pursue diagnostic testing, genetic counseling, and adequate time to make an informed decision. [3][4]
Given the broad nature of this topic, the purpose of this article is to review the indications and protocols for a standard versus specialized or “detailed” fetal ultrasound by each trimester. By recognizing the indications and understanding the differences in the fetal components assessed, clinicians will be able to correctly identify the most optimal examination based on gestational age for each patient and improve clinical outcomes.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The gestational sac is the first sign of a developing pregnancy, usually identifiable at approximately five weeks gestation. The sac is a round fluid collection that at times is surrounded by two echogenic rings representing the layers of decidua, also known as the double decidual sac sign. When the gestational sac is located on one side of the endometrium and surrounded by an echogenic area, this is known as the intradecidual sign. The absence of these signs does not rule out an intrauterine pregnancy. Visualization of any round or oval fluid collection within the mid-uterus likely represents an intrauterine pregnancy. However, a gestational sac must be distinguished from a “pseudogestational sac” in cases of a suspected ectopic pregnancy. The fluid from the ectopic pregnancy collects in the uterus and mimics a gestational sac. These collections usually contain irregular borders or debris. [5][6]
The yolk sac is a thin-walled circular structure that develops within the gestational sac, usually after 5.5 weeks of gestation, and usually resolves by 12 weeks. The yolk sac provides nutrition and gas exchange to the developing embryo. The embryo, typically visible at approximately six weeks gestation, is connected to the yolk sac at the midgut via the yolk stalk. The embryo’s first distinguishable structure is the flickering cardiac activity that should develop by a crown-rump length of 7 mm in a normal pregnancy. The presence of a gestational sac with a yolk sac or an embryo is required for a definitive diagnosis of pregnancy.[7] [5]
By 11 weeks gestation, organogenesis is complete, and most fetal anomalies have already formed by this period. Fetal anomalies are present in 2 to 3% of pregnancies, and traditionally a comprehensive fetal anatomic survey has been performed in the mid-second trimester to assess these anomalies. Due to improvement and advancement in ultrasonography, these anomalies can now be seen in the late first trimester. The common malformations of neural tube defects (anencephaly, myelomeningoceles), cystic hygromas, abdominal wall defects, limb abnormalities, and holoprosencephaly can be seen 50% of the time in singleton pregnancies at this early gestational period. Additionally, markers of aneuploidy such as hypoplastic nasal bone, abnormal cardiac findings, abnormal ductus venosus flow can be seen. However, brain structures (cavum septum pellucidum or corpus callosum) or diaphragmatic hernias are not fully developed at this stage and must be evaluated in the mid-second trimester. It is important to note that the early appearance of developing organ structures can be mistaken as anomalies to the untrained eye. For example, before 13 weeks, there is a physiological bowel herniation into the base of the umbilical cord and can be mistaken as an abdominal wall defect if specialized training is not completed before the interpretation of a late first-trimester anatomy scan.[4][3][5]
In addition to a comprehensive fetal anatomic evaluation, evaluation of the placenta, including location, texture, and cord insertion, is assessed. If placenta accreta spectrum (PAS) is suspected or a low-lying placenta is visualized on a transabdominal exam, a transvaginal approach for evaluating the placenta is recommended. Suspicion for PAS is based on clinical risks factors such as previous cesarean deliveries in addition to ultrasounds findings. In the first trimester, low implantation of the gestational sac could represent cesarean scar implantation and increase the risk of PAS. In the second and third trimesters, the presence of placenta previa in addition to placental findings of lacunae, disruption in the retroplacental hypoechoic zone, myometrial thinning, or uterovesical hypervascularity greatly increases the likelihood of PAS. The presence of placenta previa with suspicion for PAS markedly increases maternal and fetal mortality, and cesarean delivery is recommended. Detection allows for early multidisciplinary cesarean delivery planning at a tertiary care center where experienced and specialized surgeons are available.[8] [9]
Lastly, maternal pelvic anatomy(uterus, cervix, ovaries, adnexa) is assessed. Evaluation for abnormalities such as fibroids, adnexal masses, Mullerian duct anomalies is evaluated in the first trimester and mid-second trimester scans. The presence of ultrasound abnormalities or clinical indications can lead to additional specialized ultrasound examinations such as serial transvaginal cervical lengths or limited follow-up imaging.[1]
Indications
Standard First-Trimester Ultrasound Examination
As outlined by the AIUM-ACR-ACOG-SMFM-SRU practice parameters, indications include confirmation of singleton/multiple gestation intrauterine pregnancy and chorionicity/amnionicity if applicable, confirmation of cardiac activity, estimation of gestational age, evaluation of suspected ectopic pregnancy, measurement of Nuchal Translucency (NT) for aneuploidy screening, vaginal bleeding, pelvic pain, suspected gestational trophoblastic disease, or maternal pelvic organ assessment.[1]
Detailed First-Trimester Anatomy Ultrasound Examination (Early Comprehensive Fetal Anatomy Ultrasound)
This specialized diagnostic examination is an indication-driven examination for women at increased risk of fetal and/or placental anomalies performed between 12 weeks and 0 days to 13 weeks and six days either transabdominally or combined with the transvaginal approach. Indications include a previous child with an anomaly, increased Nuchal Translucency >3 mm, a suspected fetal anomaly in the current pregnancy, advanced maternal age, pregestational diabetes mellitus, maternal obesity, IVF pregnancy, teratogen exposure, congenital infection exposures, multifetal gestation, positive maternal serum screening tests, abnormal placental implantation. The best time to perform an early anatomy scan is after 13 weeks. With great emphasis, this ultrasound does not replace a detailed second-trimester anatomic survey, which should always be performed.[4][10]
Standard Second-Trimester Anatomy Ultrasound Examination
This routine anatomy ultrasound is performed between 18 to 22 weeks in every pregnancy to assess fetal anatomy, screen for anomalies, evaluate the placental location and maternal pelvic anatomy, and estimate gestational age (if not performed with an earlier scan). The standard anatomical ultrasound is performed in low-risk pregnancies who otherwise do not have indications for a detailed anatomy scan, as outlined below.[1]
Detailed Second Trimester Anatomy Ultrasound Examination
According to the AIUM-ACR-ACOG-SMFM-SRU practice parameters, this scan is an indication-driven examination and is not intended to be performed in all pregnancies. The indications include a previous child with an anomaly, increased Nuchal Translucency >3 mm, a suspected fetal anomaly in current pregnancy, advanced maternal age, pregestational diabetes mellitus, early gestational diabetes before 24 weeks, maternal obesity, IVF pregnancy, teratogen exposure, congenital infection exposures, multifetal gestation, positive maternal serum screening tests, abnormal placental implantation, parental chromosomal/genetic carrier, aneuploidy marker on previous ultrasound, alloimmunization, oligohydramnios, polyhydramnios, maternal drug use.[11]
Specialized Third Trimester Ultrasound Examination
Third-trimester ultrasounds are indication-driven examinations. Examples of types of specialized ultrasounds include the biophysical profile, additional biometric measurements follow-ups (every 3 to 4 weeks), doppler ultrasounds in the setting of growth restrictions. Indications include fetal growth restriction or suspected macrosomia, multifetal gestation, twin-twin transfusion syndrome screening (every two weeks), a significant discrepancy between the uterine size and clinical dates, evaluation of fetal well-being, evaluation of prelabour rupture of membranes, preterm labor, vaginal bleeding, suspected placental abruption, follow-up evaluation for placental appearance for suspected placenta previa, vasa previa, PAS, suspected fetal death, suspected amniotic fluid abnormalities.[1][12]
Contraindications
The absolute contraindication to performing fetal ultrasonography is patient refusal. Ultrasonography is generally safe during pregnancy and should only be used when indicated with the physician’s order under the ALARA (as low as reasonably achievable) principle. M-mode imaging should be used for documentation of cardiac activity, and pulse doppler is discouraged if it will not add valuable information to the examination.[4]
Equipment
Most examinations are performed with gray-scale real-time scanners using a transabdominal or transvaginal approach. The approach is influenced by gestational age, maternal habitus, and fetal positioning. Abdominal curvilinear transducer with 3 to 5 MHz provides enough penetration to achieve adequate resolution. Additionally, high-frequency probes (9 to 12 MHz) are used for the transvaginal approach.[4] [13]
Personnel
According to the AIUM's accreditation policies, sonographers are required to be credentialed in their practicing specialty. Ultrasound examinations are supervised by a licensed medical provider who meets the training specialty guidelines, and a qualified physician should be readily available to interpret the ultrasound examination. [3]
Additionally, according to "Training Guidelines for Physicians Who Evaluate and Interpret Diagnostic Obstetric Ultrasound Examinations," physicians and sonographers who read and perform Early Comprehensive Fetal Anatomy Ultrasounds should undergo specialized training at a teaching facility that will allow the adequate experience to become proficient. Performance of early comprehensive fetal anatomy ultrasounds should be done within referral centers with specialized expertise in reading and counseling patients on findings.[3]
Preparation
Before starting any ultrasound examination, the sonographer should confirm the correct patient, the scan to be performed, and the reason for the scan. For transabdominal ultrasounds, the patient should ideally have a full bladder for resolution enhancement of surrounding structures. For a transvaginal approach, the bladder should be empty for optimal visualization. [13]
Technique or Treatment
The Detailed First-Trimester Anatomy Ultrasound Examination is a relatively new recommendation by the AIUM-ACR-ACOG-SMFM-SRU practice parameter that has yet to be adopted as the standard of care in those who meet indications. Techniques and imaging parameters will be discussed in this section. A combined transabdominal and transvaginal approach may be needed to visualize all structures fully.
Fetal Biometry
The techniques for assessing fetal biometry via crown-rump length or biparietal diameter (BPD) and head circumference (HC) are standard and are unchanged from AIUM-ACR-ACOG-SMFM practice parameters. [10][14]
Fetal Head
Sagittal and axial planes are used for the evaluation of the fetal head structures. The skull should be oval with calvarial ossification and no bulges. The choroid plexus should be visible on each side of the falx cerebri in the transventricular plane. In the transthalamic plane, the thalami, cerebral peduncles, third ventricle, and aqueduct of Sylvius are visualized. Angling toward the posterior fossa in the axial plane allows for visualization of the fourth ventricle. The thalami, midbrain, brain stem, fourth ventricle, and future cisterna magna should also be visualized in this plane. [10][15]
Potential abnormalities: Within the midsagittal view, signs of early spina bifida are seen if the future cisterna magna appears abnormal or the fourth ventricle is absent or compressed. Posterior displacement of the aqueduct of Sylvius is also a marker for spina bifida. Enlargement of the fourth ventricle can be associated with the Dandy-Walker continuum. Anencephaly-acrania sequence, alobar holoprosencephaly, and large cephaloceles can also be detected during this period. [10] [16][17][18][15]
Limitations: The cavum septum pellucidum and corpus callosum are not visible in the late first trimester. [10]
Face and Profile
The forehead, nasal bridge, nasal bone, maxilla, and mandible should be seen in the midsagittal and views. The forehead should not be protruding or flattened, and there should be a contiguous nose to upper lip contour without maxillary protuberance or gap. The nasal bones, premaxillary processes, primary palate, and mandible can be identified by the retronasal triangle. The coronal plane is used to visualize the orbits, lenses, and upper lip integrity. [10]
Potential abnormalities: A maxillary gap is suspicious for a cleft palate. The absence of the mandibular gap is suspicious for micrognathia. [19][20]
Neck
In an axial or coronal view, the neck should be evaluated for abnormal fluid collections, cystic hygroma, or dilated jugular lymphatic sacs. The midsagittal plane is used to evaluate the nuchal translucency. Precise measurement is only required if the nuchal translucency (NT) appears enlarged or is a part of a screening for aneuploidy. There are established guidelines for the measurement of nuchal translucency to reduce false-negative and false-positive values. Guidelines for NT measurement are outlined by the AIUM-ACR-ACOG-SMFM-SRU Practice Parameter. [1]
Thorax and Heart
The required structures in the axial view are cardiac position and axis, 4-chamber view without and with color Doppler, 3-vessel and trachea view with color Doppler, symmetric lungs, and diaphragm demarcation. In the coronal and sagittal view, diaphragm demarcation should also be visualized. Though color Doppler should be limited during the first trimester, color flow is essential for the visualization of the heart structures at this gestation age. Output display standard should be monitored to keep the thermal index for bone <0.7. [10] [13]
In the axial view, the lungs should be symmetric, and the ribs should appear of normal ossification and length. The heart should be one-third the size of the chest. The four-chamber view with color Doppler should show equal-sized ventricles, with defined ventricular septum, atria, and demonstration of mitral and tricuspid flow. The three-vessel and trachea view with color Doppler should show transverse aortic arch/isthmus merging with the pulmonary trunk/ductus arteriosus. There should be antegrade flow to the left side of the trachea. In patients with suspected cardiac abnormalities, longitudinal aortic and ductal arches with pulsed wave Doppler flow may be performed.[10] [21][22]
Abdomen and Pelvis
The axial plane at the levels of the stomach, kidneys, and bladder are evaluated. The orientation of the abdomen should contain the stomach on the left and the liver on the right side, with the portal vein going away from the stomach. The umbilical cord insertion into the anterior abdominal wall is evaluated. It is important to note that physiologic herniation of the bowel into the umbilical cord base is seen before 13 weeks and is not associated with anomalies. The bladder should contain fluid. If the kidneys are not visualized in the coronal view, renal artery power or color Doppler imaging is recommended. [23][10]
Potential Abnormalities: Cystic collections within the abdomen or enlarged bladder >7 mm could indicate aneuploidy or urinary tract obstruction. [10][24]
Spine and Extremities
Three long bones should be identified in each extremity. Feet and hands should be documented. Detailed assessment of fingers/toes is required if an abnormality is suspected. The spine is evaluated in the longitudinal and axial planes with attention to scoliosis or irregularity. If skeletal dysplasia is suspected, calvarial shape, thorax, ribs, the scapula should be evaluated. [25][10]
Limitation: The distal spine is not completely ossified at this gestational period. [10]
Placenta, Uterus, and Adnexa
The placental position relative to the lower uterine segment, umbilical cord insertion, and echotexture must be evaluated. If there is suspicion for PAS, a transvaginal approach with a partially full bladder should be performed with color Doppler and myometrial thinning, bladder wall interface; uterine vesicular vascularity abnormalities should be documented. Leiomyomata size, location, and number should be documented. Ovaries, adnexa, and the cul-de-sac should be visualized. Any Mullerian duct anomalies should be documented. [10][26][27]
The components of a Standard Second-Trimester Anatomy Examination and Detailed Second Trimester Anatomy Examination are summarized in the tables at the end of this article. A detailed, comprehensive anatomy scan includes all of the components of the standard anatomy scan with additional specific components guided by the initial indication for the scan. Also, specific ultrasound findings during the standard anatomy scan can direct additional detailed anatomic evaluation as determined by the reading physician. Therefore, not all of the components listed in the detailed description may be indicated in every detailed anatomic scan. Clinical judgment is warranted.[11]
Complications
There are no major risks or complications to the fetus or mother undergoing a transabdominal ultrasound. A potential complication in the transvaginal approach is the possibility of inadvertently inserting the probe through the cervical os, causing a hemorrhage in the setting of an unknown placenta previa or vasa previa. However, this risk is very low if the scan provider or sonographer is properly credentialed and trained in the technique. Taking precautions by starting each examination with the transabdominal approach to locate the placenta can avoid this possible risk.
Clinical Significance
Screening for fetal anomalies is performed in the first and second trimester by a nuchal translucency screening, maternal serum cell-free DNA, or serum quad screen testing. When the screening test results are abnormal or suspicious for aneuploidy, diagnostic karyotyping is offered, in addition to a detailed anatomic ultrasound, evaluation to look for structural anomalies, which can be performed in the late first trimester. Findings of cystic hygroma, short femur, coarctation of the aorta, hypoplastic left heart, renal anomalies, cardiac defects, abdominal wall hernias are highly suspicious for aneuploidy, especially when combined and should prompt further diagnostic testing. [4] [3]
Diagnostic testing is outside of the scope of this topic but includes chorionic villus sampling performed between 10 to 13 weeks gestation and amniocentesis, which is optimally performed between 15 to 20 weeks of gestation. Depending on the state law, if a genetic abnormality incompatible with life is diagnosed before the third trimester, patients may have more reproductive options. Diagnosing major fetal abnormalities that will require immediate postnatal surgical intervention decreases morbidity and mortality when a multidisciplinary approach is taken to facilitate proper care and resources.[4]
Abnormalities in screening tests are not always associated with aneuploidy but can be markers of adverse pregnancy outcomes. For example, enlarged NT is associated with miscarriage, intrauterine death, or congenital heart defects. The risk of adverse outcomes is proportional to the degree of NT enlargement. An increased thickness above 3.0 mm (or above 99th percentile for crown-rump length) is directly proportional to an increased risk for aneuploidy (Down syndrome and Turner syndrome) and structural abnormalities unrelated related to aneuploidy. Congenital heart disease is the most commonly associated malformation in fetuses with euploid karyotypes. Genetic counseling, invasive genetic testing, detailed fetal anatomy scan, and fetal echocardiogram are recommended, and they should be cautiously monitored throughout the antenatal period.[28][29]
Enhancing Healthcare Team Outcomes
To optimize clinical outcomes, fetal ultrasonography is an essential component in the early detection of fetal anomalies. Beginning with the initial prenatal visit, properly identifying risk factors or exposures by the obstetrician, midwife, or nurse practitioner is important for early ultrasonography evaluation. Communication between the ultrasonographer, obstetrician, and Maternal-Fetal Medicine specialist is vital in diagnosing any major fetal anomalies or maternal complications requiring early intervention or transfer to a tertiary care center equipped with resources to safely handle the management and care of both mother and fetus. [Level 5]
Media
(Click Image to Enlarge)
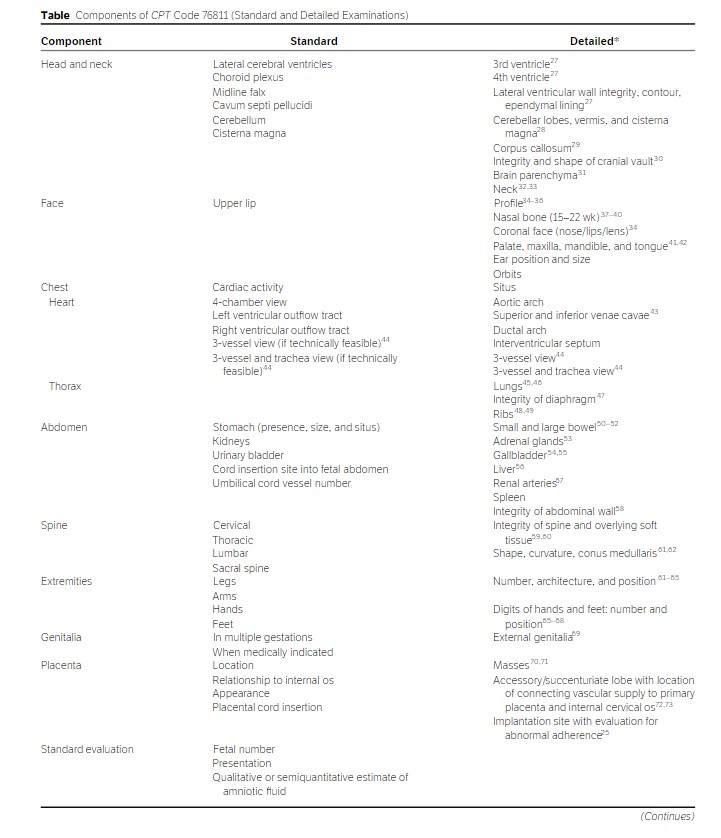
Components of CPT Code 76811 (Standard and Detailed Examinations) (2019), AIUM Practice Parameter for the Performance of Detailed Second- and Third-Trimester Diagnostic Obstetric Ultrasound Examinations. J Ultrasound Med, 38: 3093-3100. https://doi.org/10.1002/jum.15163. Used with Permission from John Wiley and Sons.
(Click Image to Enlarge)
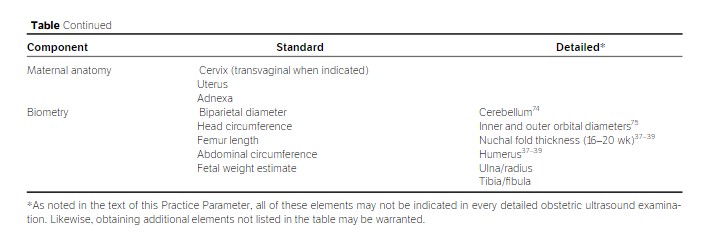
Components of CPT Code 76811 (Standard and Detailed Examinations) (2019), AIUM Practice Parameter for the Performance of Detailed Second- and Third-Trimester Diagnostic Obstetric Ultrasound Examinations. J Ultrasound Med, 38: 3093-3100. https://doi.org/10.1002/jum.15163. Used with Permission from John Wiley and Sons.
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
AIUM-ACR-ACOG-SMFM-SRU Practice Parameter for the Performance of Standard Diagnostic Obstetric Ultrasound Examinations. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2018 Nov; [PubMed PMID: 30308091]
Copel JA, Obstetric ultrasound terminology. Seminars in perinatology. 2013 Oct; [PubMed PMID: 24176151]
Mei JY,Afshar Y,Platt LD, First-Trimester Ultrasound. Obstetrics and gynecology clinics of North America. 2019 Dec; [PubMed PMID: 31677757]
Nevo O,Brown R,Glanc P,Lim K, No. 352-Technical Update: The Role of Early Comprehensive Fetal Anatomy Ultrasound Examination. Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC. 2017 Dec; [PubMed PMID: 29197487]
Doubilet PM, Ultrasound evaluation of the first trimester. Radiologic clinics of North America. 2014 Nov; [PubMed PMID: 25444100]
Doubilet PM, Benson CB. Double sac sign and intradecidual sign in early pregnancy: interobserver reliability and frequency of occurrence. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2013 Jul:32(7):1207-14. doi: 10.7863/ultra.32.7.1207. Epub [PubMed PMID: 23804343]
Donovan MF,Bordoni B, Embryology, Yolk Sac StatPearls. 2021 Jan; [PubMed PMID: 32310425]
Shainker SA,Coleman B,Timor-Tritsch IE,Bhide A,Bromley B,Cahill AG,Gandhi M,Hecht JL,Johnson KM,Levine D,Mastrobattista J,Philips J,Platt LD,Shamshirsaz AA,Shipp TD,Silver RM,Simpson LL,Copel JA,Abuhamad A,Society for Maternal-Fetal Medicine. Electronic address: pubs@smfm.org., Special Report of the Society for Maternal-Fetal Medicine Placenta Accreta Spectrum Ultrasound Marker Task Force: Consensus on definition of markers and approach to the ultrasound examination in pregnancies at risk for placenta accreta spectrum. American journal of obstetrics and gynecology. 2021 Jan; [PubMed PMID: 33386103]
Level 3 (low-level) evidenceSilver RM,Branch DW, Placenta Accreta Spectrum. The New England journal of medicine. 2018 Apr 19; [PubMed PMID: 29669225]
AIUM Practice Parameter for the Performance of Detailed Diagnostic Obstetric Ultrasound Examinations Between 12 Weeks 0 Days and 13 Weeks 6 Days. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2021 May; [PubMed PMID: 32852128]
AIUM Practice Parameter for the Performance of Detailed Second- and Third-Trimester Diagnostic Obstetric Ultrasound Examinations. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2019 Dec; [PubMed PMID: 31736130]
Bahtiyar MO,Emery SP,Dashe JS,Wilkins-Haug LE,Johnson A,Paek BW,Moon-Grady AJ,Skupski DW,O'Brien BM,Harman CR,Simpson LL,North American Fetal Therapy Network., The North American Fetal Therapy Network consensus statement: prenatal surveillance of uncomplicated monochorionic gestations. Obstetrics and gynecology. 2015 Jan; [PubMed PMID: 25560113]
Level 3 (low-level) evidenceAIUM Practice Parameter for the Performance of Limited Obstetric Ultrasound Examinations by Advanced Clinical Providers. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2018 Jul; [PubMed PMID: 30133848]
Lee WA,Nelson G,Grogan SP, Sonography 1st Trimester Assessment, Protocols, And Interpretation StatPearls. 2021 Jan; [PubMed PMID: 34424643]
Volpe P,Contro E,Fanelli T,Muto B,Pilu G,Gentile M, Appearance of fetal posterior fossa at 11-14 weeks in fetuses with Dandy-Walker malformation or chromosomal anomalies. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2016 Jun [PubMed PMID: 25914043]
Syngelaki A,Hammami A,Bower S,Zidere V,Akolekar R,Nicolaides KH, Diagnosis of fetal non-chromosomal abnormalities on routine ultrasound examination at 11-13 weeks' gestation. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2019 Oct [PubMed PMID: 31408229]
Chen FC,Gerhardt J,Entezami M,Chaoui R,Henrich W, Detection of Spina Bifida by First Trimester Screening - Results of the Prospective Multicenter Berlin IT-Study. Ultraschall in der Medizin (Stuttgart, Germany : 1980). 2017 Apr; [PubMed PMID: 25876171]
Martinez-Ten P,Illescas T,Adiego B,Estevez M,Bermejo C,Wong AE,Sepulveda W, Non-visualization of choroid plexus of fourth ventricle as first-trimester predictor of posterior fossa anomalies and chromosomal defects. Ultrasound in obstetrics [PubMed PMID: 28236314]
Chaoui R,Orosz G,Heling KS,Sarut-Lopez A,Nicolaides KH, Maxillary gap at 11-13 weeks' gestation: marker of cleft lip and palate. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2015 Dec [PubMed PMID: 26277990]
Sepulveda W,Wong AE,Viñals F,Andreeva E,Adzehova N,Martinez-Ten P, Absent mandibular gap in the retronasal triangle view: a clue to the diagnosis of micrognathia in the first trimester. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2012 Feb [PubMed PMID: 22009662]
Persico N,Moratalla J,Lombardi CM,Zidere V,Allan L,Nicolaides KH, Fetal echocardiography at 11-13 weeks by transabdominal high-frequency ultrasound. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2011 Mar [PubMed PMID: 21229572]
Hutchinson D, McBrien A, Howley L, Yamamoto Y, Sekar P, Motan T, Jain V, Savard W, Hornberger LK. First-Trimester Fetal Echocardiography: Identification of Cardiac Structures for Screening from 6 to 13 Weeks' Gestational Age. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2017 Aug:30(8):763-772. doi: 10.1016/j.echo.2017.03.017. Epub 2017 May 13 [PubMed PMID: 28511860]
Bogers H,Baken L,Cohen-Overbeek TE,Koning AHJ,Willemsen SP,van der Spek PJ,Exalto N,Steegers EAP, Evaluation of First-Trimester Physiological Midgut Herniation Using Three-Dimensional Ultrasound. Fetal diagnosis and therapy. 2019; [PubMed PMID: 30110700]
Girard N,Viaris de Lesegno B,Bussière P,Egoroff C,Cordier AG,Benachi A, Prognosis of Isolated First-Trimester Fetal Megacystis with Spontaneous Resolution. Fetal diagnosis and therapy. 2017 [PubMed PMID: 28399525]
Khalil A,Pajkrt E,Chitty LS, Early prenatal diagnosis of skeletal anomalies. Prenatal diagnosis. 2011 Jan [PubMed PMID: 21210484]
Cali G,Forlani F,Foti F,Minneci G,Manzoli L,Flacco ME,Buca D,Liberati M,Scambia G,D'Antonio F, Diagnostic accuracy of first-trimester ultrasound in detecting abnormally invasive placenta in high-risk women with placenta previa. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2018 Aug [PubMed PMID: 29532529]
D'Antonio F,Timor-Tritsch IE,Palacios-Jaraquemada J,Monteagudo A,Buca D,Forlani F,Minneci G,Foti F,Manzoli L,Liberati M,Acharya G,Calì G, First-trimester detection of abnormally invasive placenta in high-risk women: systematic review and meta-analysis. Ultrasound in obstetrics [PubMed PMID: 28833750]
Level 1 (high-level) evidenceBilardo CM,Timmerman E,Pajkrt E,van Maarle M, Increased nuchal translucency in euploid fetuses--what should we be telling the parents? Prenatal diagnosis. 2010 Feb; [PubMed PMID: 20077440]
Ghi T,Huggon IC,Zosmer N,Nicolaides KH, Incidence of major structural cardiac defects associated with increased nuchal translucency but normal karyotype. Ultrasound in obstetrics [PubMed PMID: 11844199]


