Introduction
Weber's syndrome was described first by the German-born English physician Hermann Weber in a 52-year-old male who had developed left-sided third nerve palsy with right-sided hemiplegia caused by an acute bleed in the left cerebral peduncle.[1]
Weber syndrome, classically described as a midbrain stroke syndrome and superior alternating hemiplegia, involves oculomotor fascicles in the interpeduncular cisterns and cerebral peduncle, thereby causing ipsilateral third nerve palsy with contralateral hemiparesis. It most commonly results from the occlusion of a branch of the posterior cerebral artery.
The oculomotor(third cranial) nerve has two main motor nuclei, the main motor nucleus, and the accessory parasympathetic nucleus. The main motor nucleus is located in the tectum portion of the midbrain at the level of the superior colliculus and supplies all the extraocular muscles except the lateral rectus and the superior oblique muscles[2], and the levator palpebrae superioris. The accessory parasympathetic nucleus, also known as the Edinger Westphal nucleus, is situated posterior to the main motor nucleus and its postganglionic fibers pass through the short ciliary nerves to supply the constrictor pupillae of the iris and the ciliary muscles.
The nerve fascicles then travel forward and lateral through the red nucleus and converge at the interpeduncular fossa before exiting the midbrain. As the nucleus and fascicles are spread over a large area of the midbrain, lesions in the midbrain can present with either partial or complete third nerve palsy. The lesions in lower midbrain affect the extraocular muscles but spare the pupils, while lesions affecting both upper and middle parts of the midbrain are associated with pupillary dilatation.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
A lesion in the ventromedial portion of midbrain leads to Weber syndrome. The midbrain receives its blood supply from the paramedian mesencephalic branches (basilar), peduncular perforating branches (posterior cerebral artery) as well as from the superior cerebellar artery, and the choroidal arteries.[3]
Isolated infarctions of the paramedian mesencephalic and the peduncular perforating branches are the most common cause of Weber syndrome.[4] Less common etiologies include hemorrhage, aneurysms, tumors, and demyelinating diseases. [4]
Antecedent history of hypertension, diabetes, hypercholesterolemia is often associated with Weber syndrome, like other strokes.
In one case series, isolated midbrain infarction was seen in only 7.6% of the cases and most were associated with the concurrent infraction in other vascular territories of the vertebrobasilar system.[3]The causes for the midbrain infarction were categorized in the decreasing order of frequency into[3]
- Cardioembolism
- Insitu thrombosis
- Large artery to artery embolism and
- Intrinsic perforator branch disease (lacunar infarct)
Epidemiology
The incidence of isolated midbrain infarction causing Weber syndrome is not known mostly it occurs in conjunction with infarction in other areas of the vertebrobasilar system. One study found an isolated midbrain infarction occurring in only 0.7% of patients with posterior circulation strokes.[3]
History and Physical
Patients with weber syndrome present with drooping of the eyelid, diplopia associated with contralateral partial or complete weakness of upper limb and lower limb. The presence of crossed deficits, either sensory or motor, along with occasional association with ataxia (involvement of the red nucleus) and parkinsonian rigidity (involvement of the substansia nigra) are the characteristic neurological findings in this syndrome.[4]
On neurological examination, higher mental functions are usually normal and not commonly affected in an isolated Weber syndrome. Ptosis may be present, and on opening the affected eye, the eye is mostly shifted downwards and outwards, due to the unopposed action of superior oblique and lateral rectus muscles.
Dilated unresponsive pupils may occur if both upper and middle midbrain are affected, pupils may be spared if only lower midbrain is affected by the inciting insult. Contralateral ataxia and sometimes parkinsonian type of rigidity may be seen associated with the weakness.
Khalil et al. reported the association of Weber syndrome with vertical gaze palsy owing to the involvement of the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF) in the midbrain, dorsal to the red nucleus.[5]
The fascicular arrangement of the midbrain oculomotor nerve is speculated to be a pupillary component, extraocular movement, and eyelid elevation in that rostrocaudal order.[6]
Evaluation
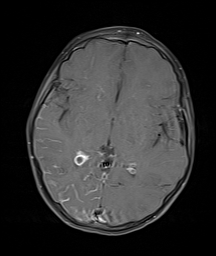
As with each case of suspected stroke, the patient should first have a thorough neurologic examination and a measure of the National Institute of Health Stroke Scale (NIHSS) score. [7] The emergent diagnosis is made by an urgent Computerised Tomography (CT) of the brain, since it is fast and more readily available in most centers. However, since there can be the propagation of the stroke to other vascular territories within the vertebrobasilar system, other additional radiological modalities such as Magnetic Resonance Imaging (MRI) along with stroke sequences, angiographic and the perfusion studies may also need to be done.
Treatment / Management
The immediate management is similar to other patients with stroke with an emphasis on the airway, breathing, and circulation along with quick and complete neurological assessment.
The patients with an isolated Weber syndrome are mostly neurologically stable. However, scenarios wherein the large infarction and there is a risk of the propagation of the disease process, thrombolytic therapy may be justified.[3] Neurosurgical management is only warranted in
- Cases with massive posterior circulation infarction, wherein there is need of emergent posterior fossa decompression
- External ventricular drain placement in cases of evolving hydrocephalus
- As an adjunct to surgical management for tumors and aneurysm causing Weber syndrome.
Apart from these, supportive care is most important, including early mobilization, bladder bowel care, and nutritional support.
Differential Diagnosis
Other midbrain syndromes are Benedikt, Claude's and Nothnagel syndrome.
Benedikt syndrome, also called Paramedian midbrain syndrome, is also caused by an insult in the tegmentum of the midbrain and cerebellum. It is characterized by the presence of oculomotor nerve palsy and cerebellar ataxia including tremor and involuntary choreoathetotic movements.
Claude's syndrome is similar to Weber syndrome in that it presents with ipsilateral oculomotor nerve palsy with contralateral hemiparesis but also includes contralateral ataxia. It occurs due to the involvement of oculomotor nerve, red nucleus and brachium conjunctivum.
Another famously described Weber syndrome is the Sturge-Weber syndrome (SWS), also called encephalotrigeminal angiomatosis, which is a neurocutaneous syndrome with angiomas involving the leptomeninges and skin of the face, typically ophthalmic (V1) and maxillary (V2) distribution areas of the trigeminal nerve. The hallmark of SWS is a facial cutaneous venous dilation, also referred to as a nevus flammeus or port-wine stain (PWS).
Yet another Weber syndrome is the Klippel-Trenaunay-Weber syndrome (KTWS), characterized by a triad of port-wine stain, varicose veins, and bony and soft tissue hypertrophy involving an extremity.
Prognosis
Prognosis depends on the etiology of Weber syndrome. Early detection, timely management, effective supportive therapy to prevent complications and precautionary measures to prevent recurrence of similar stroke are the most important factor determining the neurological outcome in these patients.
Complications
Weber syndrome is ten times more likely to occur in conjunction with pontine infarction. It has been to be involved as a middle territory syndrome of the posterior circulation in as many as 50% of patients.[3] There is the risk of massive posterior circulation infarction with tonsillar herniation, and eventual death. There may be evolving hydrocephalus as well.
After recovery from the acute event, early mobilization is advised strictly to avoid secondary complications like contractures, bedsores, aspiration pneumonia, deep vein thrombosis, pulmonary embolism and secondary infections such as pneumonia and urinary tract infections. Early dysphagia screening and if any swallowing difficulty is present, Nasogastric feeding needs to be initiated. Early physiotherapy to recover motor power, prevent spasticity, and thereby improving the quality of life is of paramount importance.[8]
Postoperative and Rehabilitation Care
Passive full range-of-motion exercises for paralyzed limbs should be started as early as possible( Within 24 hours, if possible). They should be referred to a physiotherapist or dedicated stroke rehabilitation team.
The clinical presentation, rather than the location of the stroke, should determine the rehabilitation focus for brainstem stroke patients.[9]
As with any other stroke patients, other rehabilitative measures are also undertaken. Standard heparin (5000 units subcutaneous b.d.) or LMW heparin in order to prevent deep vein thrombosis and pulmonary embolism is advocated in bedridden patients.
Early bladder training with the removal of the indwelling catheters, laxatives, and stool softeners are also essential measures to be taken into considerations.
Consultations
The holistic care approach needs to be implemented with the consultation of the
- Physiotherapist & Rehabilitation unit
- Neurosurgeon
- Internal medicine( for risk factor management)
Deterrence and Patient Education
Transient ischemic attack (TIA) in the posterior circulation are easily missed. Thrombolytic therapy is also delayed in patients with these strokes with prolonged door to needle time. Moreover, there is a three-fold risk of recurrent stroke, in cases of vertebrobasilar stenosis. Therefore, it is prudent for increasing awareness of the salient early features of posterior circulation strokes in patients. These patients need to be urgently evaluated and managed for preventing life-threatening complications. These patients need to be referred early to stroke units for the probable early thrombolysis.
Pearls and Other Issues
The time window for treatment for basilar occlusion have been extended to 24 hours since the white matter fibers forming a major component of the brainstem are more tolerant of ischemic insult. Moreover, abundant collaterals also help in minimizing neuronal death.
Emergency posterior fossa decompression may be life-saving in few patients with massive brainstem infarction.
Enhancing Healthcare Team Outcomes
The use and education about the FAST acronym (face drooping, arm weakness, speech difficulty, time to call emergency services) have been supported widely.[10] Calling EMS (by dialing 9-1-1 in the United States) when a stroke is suspected must be emphasized because the use of EMS is associated with faster arrival to the emergency department (ED) and higher rates of treatment with reperfusion therapies.
A quick and detailed examination on arrival to the ED, early imaging and communication to stroke team( for thrombolysis, if feasible) is to be followed religiously.
Nursing care is extremely important in early recovery and rehabilitation of such patients, in the form of early mobilization, optimum positioning, nutritional support, assisted physiotherapy and preventions of secondary complications.
Media
(Click Image to Enlarge)
References
Silverman IE, Liu GT, Volpe NJ, Galetta SL. The crossed paralyses. The original brain-stem syndromes of Millard-Gubler, Foville, Weber, and Raymond-Cestan. Archives of neurology. 1995 Jun:52(6):635-8 [PubMed PMID: 7763214]
Nadeau SE,Trobe JD, Pupil sparing in oculomotor palsy: a brief review. Annals of neurology. 1983 Feb; [PubMed PMID: 6830173]
Level 3 (low-level) evidenceMartin PJ,Chang HM,Wityk R,Caplan LR, Midbrain infarction: associations and aetiologies in the New England Medical Center Posterior Circulation Registry. Journal of neurology, neurosurgery, and psychiatry. 1998 Mar [PubMed PMID: 9527158]
Ruchalski K,Hathout GM, A medley of midbrain maladies: a brief review of midbrain anatomy and syndromology for radiologists. Radiology research and practice. 2012; [PubMed PMID: 22693668]
Khalil M,Malik TG,Farooq K, Weber's syndrome with vertical gaze palsy. Journal of the College of Physicians and Surgeons--Pakistan : JCPSP. 2009 Oct; [PubMed PMID: 19811724]
Level 3 (low-level) evidenceSaeki N,Murai H,Mine S,Yamaura A, Fascicular arrangement within the oculomotor nerve MRI analysis of a midbrain infarct. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2000 May [PubMed PMID: 10833630]
Level 3 (low-level) evidenceBai QK,Zhao ZG,Lu LJ,Shen J,Zhang JY,Sui HJ,Xie XH,Chen J,Yang J,Chen CR, Treating ischaemic stroke with intravenous tPA beyond 4.5 hours under the guidance of a MRI DWI/T2WI mismatch was safe and effective. Stroke and vascular neurology. 2019 Mar; [PubMed PMID: 31105973]
Nouh A,Remke J,Ruland S, Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Frontiers in neurology. 2014 [PubMed PMID: 24778625]
Teasell R, Foley N, Doherty T, Finestone H. Clinical characteristics of patients with brainstem strokes admitted to a rehabilitation unit. Archives of physical medicine and rehabilitation. 2002 Jul:83(7):1013-6 [PubMed PMID: 12098164]
Level 2 (mid-level) evidenceHasan TF,Rabinstein AA,Middlebrooks EH,Haranhalli N,Silliman SL,Meschia JF,Tawk RG, Diagnosis and Management of Acute Ischemic Stroke. Mayo Clinic proceedings. 2018 Apr; [PubMed PMID: 29622098]