Introduction
Cervical cancer screening has become one of the cornerstones of preventative screening in the gynecological world. George Papanicolaou invented this screening event, hence the name "Pap" smear, and was first used in 1943. The test collects cervical cells near the cervical transitional (transformation) zone and determines if any of them have precancerous changes. Since 1943, few classification systems have been put in place to detail the different types of collected cells; the current system followed in the United States is the 2014 Bethesda System for Reporting Cervical Cytology.[1]
Guidelines for Pap smear testing frequency vary between the United States Preventative Service Task Force and the American College of Obstetricians and Gynecologists but are recommended for women between 21 and 65. Screening is not recommended for those younger than 21. The prevalence of abnormal Pap smears is around 3.8%. At least 50 million Pap smears are performed yearly.[2] In 2019, there were an estimated 13,000 women diagnosed with cervical cancer and 4000 women who died from cervical cancer.[3]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Pap smears are the screening tool to assess cellular changes within the cervix. Documentation exists for varying levels of sensitivity and specificity for the test.[4] Because the test is not 100% sensitive, it is important to conduct pap smears routinely.[5][6] From a societal lens, there are racial disparities in the timeliness of cervical cancer diagnosis. The localized diagnosis of cervical cancer is 47% in White and 36% in Black individuals. The regionalized diagnosis of cervical cancer is 35% in White and 41% in Black populations.[3] There is a decrease in the early detection of cervical cancer in Black women, which results in detection when the disease has further progressed.
Causes
The primary cause of abnormal pap smears is associated with infection by human papillomavirus (HPV). HPV serotypes 16/18 are the most common strains that cause cervical cancer.[7] Both of these serotypes appear in 70% of cervical cancer cases. Lower-risk HPV serotypes include serotypes 6 and 11. Smoking has also been shown to increase the risk of cervical cancer.[8] The carcinogens in the smoke disseminate throughout the body and are identifiable in cervical mucus. These carcinogens can alter the oncogene balance within these cells, resulting in cancerous growth. Research also shows that women who have a high number of full-term pregnancies are at an increased risk of developing cervical cancer.[9] Women who take oral contraception for prolonged periods have a temporary increase in the risk of acquiring cervical cancer.[10] Additionally, patients who have human immunodeficiency virus or are immunocompromised have an increased risk of acquiring HPV, which can lead to cervical cancer. Both of these reduce the ability of the immune system to clear the virus. From a more historical reference, children who had their mother take diethylstilbestrol during the pregnancy are at elevated risk of clear cell adenocarcinoma of the vagina and cervix.[11] DES was prescribed to pregnant mothers between 1938 and 1974 to help reduce the risks of premature labor; it is no longer prescribed.
Anatomical Pathology
Cervical cancer screening requires acquiring cervical cells in the transitional zone in the cervix. The transitional zone is also called the squamocolumnar junction because it is the joining process of the ectocervix and the endocervix. The ectocervix is comprised of non-keratinized stratified squamous epithelium, while the endocervix is simple columnar epithelium. The simple columnar cells also have glandular cells that secrete mucus.
The anatomic pathology for cervical cytology mainly arises from the 2 cell types found in the transitional zone: epithelial and glandular. Epithelial cell pathology is graded in an ascending fashion:
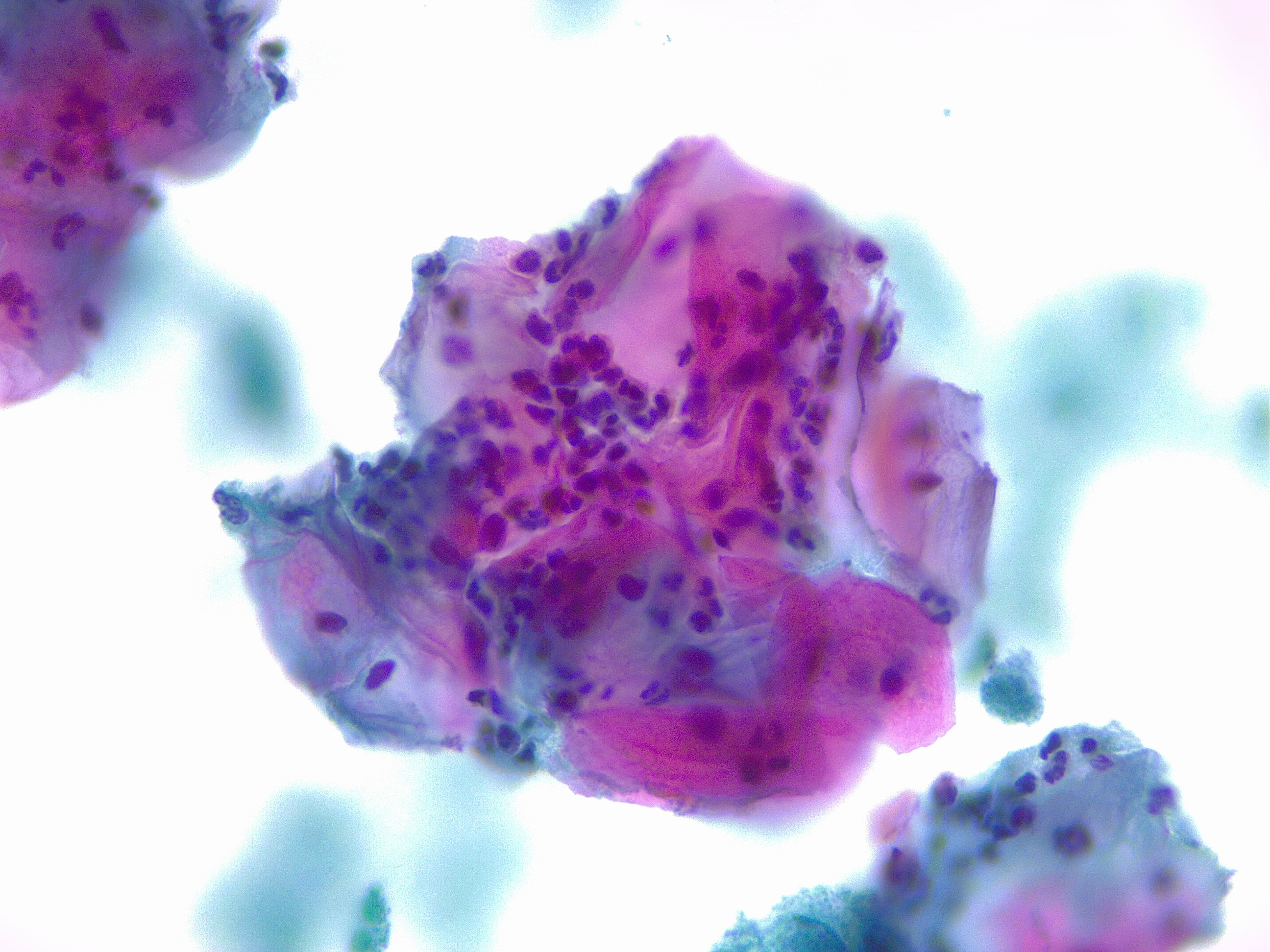
- Atypical squamous cells of undetermined significance: This is the most common abnormal pap smear diagnosis.[12] This diagnosis usually correlates with an HPV infection. This diagnosis can reflect precancerous changes in the cells but can also be caused by inflammation or as a response to trauma (see Image. Squamous Cells, Acute Inflammation).
- Atypical squamous cells- not excluding high-grade intraepithelial lesions: This diagnosis is exceedingly rare and requires colposcopy to assume that there truly are no high-grade intraepithelial lesions.
If the pathologist can determine that there is a morphological change within the cells, the following is the nomenclature used:
- Low-grade squamous intraepithelial lesions: This definition covers the spectrum of changes in squamous cells that can potentially progress to squamous cell carcinoma. This finding is highly suggestive of an HPV infection. This nomenclature includes cervical intraepithelial neoplasia (CIN) 1 and mild dysplasia. While this finding is present in 2% of all pap smears, the regression rate of low-grade squamous intraepithelial lesions (LSIL) in 2 years is over 85%.[13] Less than a quarter of LSIL findings will progress to higher-grade lesions.
- High-grade squamous intraepithelial lesions: This definition is a general title for abnormalities in squamous cells with a serious concern of progressing to cervical cancer. This finding is highly suggestive of an HPV infection. This title includes the historical terminology of CIN2, CIN3, moderate dysplasia, severe dysplasia, and carcinoma in situ.[14]
- Squamous cell carcinoma: This is rarely diagnosed on a pap smear.[15] This condition only occurs with a significant progression of cervical cancer.
In addition to the epithelial cells, the pathologist can identify abnormal glandular cells, which are graded in an ascending fashion:
- Atypical glandular cells: This cell type can be found in the endocervix and can also appear in other parts of the reproductive tract, like the endometrium. It is diagnosed in 0.3% of all Pap smears. Atypical glandular cells (AGC) identify cells that have progressed beyond temporary inflammatory changes but have not mutated as much to be diagnosed as adenocarcinoma.[16] AGC divides into 2 main areas that are either "undetermined significance" or "undetermined significance with a squamous abnormality." Squamous abnormalities can be found in 31% of AGC diagnoses and are more likely to appear in patients under the age of 35.[17] ACG is also divided based on the suspected origin of the glandular cells. A diagnosis of AGC increases the risk of cancers throughout a woman's reproductive tract.
- Atypical glandular cells favor endocervical origin: This diagnosis is least likely to have associated endometrial cancer.[18]
- Atypical glandular cells favor endometrial origin: This diagnosis is most likely to have associated endometrial cancer.[18]
- Atypical glandular cells not otherwise specified: This diagnosis is in the middle, having an association with endometrial cancer.[18]
- Endocervical adenocarcinoma in situ: This diagnosis has become more frequent over the previous decades. The prevalence is 11.2 per 100,000 and is most likely to be diagnosed in patients between the age of 30 to 40.[19] Endocervical adenocarcinoma in situ (AIS) usually correlates with a squamous lesion. Like the other abnormal Pap smear findings, high-risk serotypes of HPV are a risk factor.
- Adenocarcinoma: This diagnosis is the invasive version of AIS, which can be found in the transition zone but is more commonly present within the cervical canal. This condition also derives from the glandular cells of the endometrium.[20] There has been an increase in this diagnosis even though there has been a reduction in cervical squamous carcinoma cases.
- Adenocarcinoma malignum: A rare cervical disease that is diagnosable with a pap smear. This disease usually arises in the endocervical region and is often misdiagnosed as a benign lesion.[21] Cytologic features include significant cytoplasm with ovoid nuclei.[22] Histologically, the cells are in a honeycomb pattern. The mucinous glands secrete copious fluid leading to symptomatic vaginal discharge.
Less commonly, abnormal Pap smears can arise from other histological subtypes. Cervical cancer can arise from a neuroendocrine origin, with the 2 main subtypes being large and small cell. Other types of tumors that can cause cervical cancer include sarcoma, lymphoma, and melanoma.
Clinical Pathology
Abnormal Pap smears can present without any symptoms; it is important to ask about bleeding between periods, changes in the menstrual cycle, abnormal vaginal discharge, and dyspareunia. An increase in either unexplained bleeding or menstrual bleeding should raise concerns to evaluate the possibility of cervical cancer. Bleeding in postmenopausal women is especially concerning for neoplasms. If the patient has a more advanced case of cervical cancer, she can experience pelvic pain and dysuria.
Biochemical and Genetic Pathology
The most common etiology of abnormal pap smears is due to HPV infections. HPV is an enveloped, circular, double-stranded deoxyribonucleic acid virus. The high-risk HPV serotypes are 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68 because they make the oncoproteins E6 and E7.[23][24] Both of these oncoproteins result in the immortalization of the infected cervical cells. E6 binds to the intracellular transformation-related protein (p)53, causing it to degrade. The p53 protein is primarily utilized in the apoptotic pathway to upregulate the transcription of p53 upregulated modulator of apoptosis, PUMA, and phorbol-12-myristate-13-acetate-induced protein 1, NOXA, leading to cell death. E7 focuses on activating the cell cycle, allowing for replication.
In non-infected cells, one of the ways the cell cycle becomes arrested in G1 is with the binding of Rb to E2F. E2F is a transcriptional activator needed to progress the cell into the S phase but cannot when bound to Rb. In the high-risk strains of HPV, E7 binds to Rb, causing E2F to be released.[25] With E2F unbound from Rb, the infected cells are signaled to begin the S phase. Genetically, BRCA mutations play a role in the susceptibility of developing cervical cancer. BRCA stands for the breast cancer gene, and its translational product is a tumor suppressor protein. BRCA1 and 2 are integral in many pathways but are especially important for deoxyribonucleic acid (DNA) repair. When there are double-stranded DNA breaks, these proteins help with homologous recombination repair. Without these proteins, there is genomic instability that can lead to neoplastic changes.[26]
Morphology
The morphological changes recognized in abnormal Pap smears include multinucleation, hyperchromasia, and perinuclear cytoplasmic vacuolization. The nuclei of the cells can also become enlarged around three times greater than the normal cell nucleus. Other nucleic features include higher levels of keratinization but an absence of nucleoli. These changes that squamous cells undergo are categorized as koilocytosis.
Mechanisms
A Pap smear is collected with a brush inserted into the cervical os. It is important to have the brush extend beyond the visualized portion to increase the chance of successfully collecting cells from the transition zone. A similar tool to the brush is a spatula or broom. The 2 mechanisms for analyzing the collected cells are liquid-based cytology (thin prep, sure path) and conventional cytology. There are 2 subtypes of this cytology.[27] One allows for the collection device to be broken off and kept with the sample that is to be analyzed. Another requires the aggravation of the collection tool since the tool does not go with the sample to be analyzed.
Liquid-based cytology preserves the cells in a buffered alcoholic solution. It has been suggested that liquid-based can better identify glandular pathology. The conventional cytology method directly transfers the cells collected from the brush onto a slide. This transfer is why this technique is called a pap smear. When transferring the specimen onto the slide, it is important to minimize drying artifacts due to prolonged contact with the air. According to the American College of Obstetricians and Gynecologists (ACOG), both the liquid-based and conventional techniques are equally effective at screening for cervical cancer.
Clinicopathologic Correlations
Abnormal pap smear findings for ACG in the setting of patients with HPV serotype 16/18 are at increased risk for AIS and should have more careful screening. When there is AIS with concomitant LSIL, the physician should progress the workup as if it is an AIS diagnosis.
Clinical Significance
The Papanicolaou smear is an effective screening test that detects cervical cancer as well as cellular changes that have the potential to develop into cervical cancer. Any diagnosis of an atypical pap smear results in more frequent and/or further testing. Below are the current recommendations from ACOG for each abnormal result.
- Atypical squamous cells of undetermined significance, ASC-US: This management plan depends on the age of the patient. For patients between 21 and 24, repeat Pap smear in 1 year if the status of the HPV is positive or unknown. It is also acceptable to perform a reflex HPV test on the same pap smear sample. HPV status will determine future pap smear frequencies. If HPV is negative, then the patient is recommended for follow-up in 3 years. If the follow-up Pap smear continues to show ASC-US, then an additional Pap smear in 1 year is recommended. For patients between 25 and 29, screening is still the same if they have negative HPV. However, if they have positive HPV, colposcopy is recommended instead of waiting one year for a follow-up pap smear. If at the follow-up pap smear, ASC-US is still present, the next step is colposcopy. For patients between 30 to 65 years of age, there is a more significant concern for the progression of cervical cancer. If ASC-US is documented on a pap smear and they are HPV negative, they will follow the same process as the other age groups. If HPV status is positive or unknown, then a repeat pap smear is recommended within four months.
- LSIL: Repeat Pap smear in 1 year.
- Atypical squamous cells, ASC-H: Further test the patient immediately with colposcopy.
- HSIL: Further test the patient immediately with colposcopy.
- AGC: Further testing can include endocervical sampling and an endometrial biopsy to source the location of the cells. It is essential to ask for pointed family history at this time. The patient should have her HPV status evaluated.
- AIS: Immediate diagnostic excision procedure along with an endocervical and endometrial biopsy. The diagnostic excision will help confirm diagnosis as well as understand the extent of the invasion.
- Squamous cell carcinoma: Immediate excision and further workup are necessary.
Guidelines for recommendations can vary when looking at different societies and groups.
Media
(Click Image to Enlarge)
References
Nayar R, Wilbur DC. The Pap test and Bethesda 2014. Cancer cytopathology. 2015 May:123(5):271-81. doi: 10.1002/cncy.21521. Epub 2015 May 1 [PubMed PMID: 25931431]
Kurman RJ, Henson DE, Herbst AL, Noller KL, Schiffman MH. Interim guidelines for management of abnormal cervical cytology. The 1992 National Cancer Institute Workshop. JAMA. 1994 Jun 15:271(23):1866-9 [PubMed PMID: 8196145]
Level 1 (high-level) evidenceSiegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA: a cancer journal for clinicians. 2019 Jan:69(1):7-34. doi: 10.3322/caac.21551. Epub 2019 Jan 8 [PubMed PMID: 30620402]
Sørbye SW, Suhrke P, Revå BW, Berland J, Maurseth RJ, Al-Shibli K. Accuracy of cervical cytology: comparison of diagnoses of 100 Pap smears read by four pathologists at three hospitals in Norway. BMC clinical pathology. 2017:17():18. doi: 10.1186/s12907-017-0058-8. Epub 2017 Aug 29 [PubMed PMID: 28860942]
Koonmee S, Bychkov A, Shuangshoti S, Bhummichitra K, Himakhun W, Karalak A, Rangdaeng S. False-Negative Rate of Papanicolaou Testing: A National Survey from the Thai Society of Cytology. Acta cytologica. 2017:61(6):434-440. doi: 10.1159/000478770. Epub 2017 Jul 25 [PubMed PMID: 28738387]
Level 3 (low-level) evidenceCastillo M, Astudillo A, Clavero O, Velasco J, Ibáñez R, de Sanjosé S. Poor Cervical Cancer Screening Attendance and False Negatives. A Call for Organized Screening. PloS one. 2016:11(8):e0161403. doi: 10.1371/journal.pone.0161403. Epub 2016 Aug 22 [PubMed PMID: 27547971]
Wentzensen N, Arbyn M. HPV-based cervical cancer screening- facts, fiction, and misperceptions. Preventive medicine. 2017 May:98():33-35. doi: 10.1016/j.ypmed.2016.12.040. Epub 2017 Feb 6 [PubMed PMID: 28279260]
Chatzistamatiou K, Moysiadis T, Vryzas D, Chatzaki E, Kaufmann AM, Koch I, Soutschek E, Boecher O, Tsertanidou A, Maglaveras N, Jansen-Duerr P, Agorastos T. Cigarette Smoking Promotes Infection of Cervical Cells by High-Risk Human Papillomaviruses, but not Subsequent E7 Oncoprotein Expression. International journal of molecular sciences. 2018 Jan 31:19(2):. doi: 10.3390/ijms19020422. Epub 2018 Jan 31 [PubMed PMID: 29385075]
Roura E, Travier N, Waterboer T, de Sanjosé S, Bosch FX, Pawlita M, Pala V, Weiderpass E, Margall N, Dillner J, Gram IT, Tjønneland A, Munk C, Palli D, Khaw KT, Overvad K, Clavel-Chapelon F, Mesrine S, Fournier A, Fortner RT, Ose J, Steffen A, Trichopoulou A, Lagiou P, Orfanos P, Masala G, Tumino R, Sacerdote C, Polidoro S, Mattiello A, Lund E, Peeters PH, Bueno-de-Mesquita HB, Quirós JR, Sánchez MJ, Navarro C, Barricarte A, Larrañaga N, Ekström J, Lindquist D, Idahl A, Travis RC, Merritt MA, Gunter MJ, Rinaldi S, Tommasino M, Franceschi S, Riboli E, Castellsagué X. The Influence of Hormonal Factors on the Risk of Developing Cervical Cancer and Pre-Cancer: Results from the EPIC Cohort. PloS one. 2016:11(1):e0147029. doi: 10.1371/journal.pone.0147029. Epub 2016 Jan 25 [PubMed PMID: 26808155]
Marks M, Gravitt PE, Gupta SB, Liaw KL, Kim E, Tadesse A, Phongnarisorn C, Wootipoom V, Yuenyao P, Vipupinyo C, Rugpao S, Sriplienchan S, Celentano DD. The association of hormonal contraceptive use and HPV prevalence. International journal of cancer. 2011 Jun 15:128(12):2962-70. doi: 10.1002/ijc.25628. Epub 2010 Oct 26 [PubMed PMID: 20734390]
Conlon JL. Diethylstilbestrol: Potential health risks for women exposed in utero and their offspring. JAAPA : official journal of the American Academy of Physician Assistants. 2017 Feb:30(2):49-52. doi: 10.1097/01.JAA.0000511800.91372.34. Epub [PubMed PMID: 28098674]
Garrett LA, McCann CK. Abnormal cytology in 2012: management of atypical squamous cells, low-grade intraepithelial neoplasia, and high-grade intraepithelial neoplasia. Clinical obstetrics and gynecology. 2013 Mar:56(1):25-34. doi: 10.1097/GRF.0b013e3182833eed. Epub [PubMed PMID: 23337842]
Ciavattini A, Clemente N, Tsiroglou D, Sopracordevole F, Serri M, Delli Carpini G, Papiccio M, Cattani P. Follow up in women with biopsy diagnosis of cervical low-grade squamous intraepithelial lesion (LSIL): how long should it be? Archives of gynecology and obstetrics. 2017 Apr:295(4):997-1003. doi: 10.1007/s00404-017-4335-7. Epub 2017 Mar 3 [PubMed PMID: 28255767]
Khieu M, Butler SL. High-Grade Squamous Intraepithelial Lesion of the Cervix. StatPearls. 2024 Jan:(): [PubMed PMID: 28613479]
Katki HA, Schiffman M, Castle PE, Fetterman B, Poitras NE, Lorey T, Cheung LC, Raine-Bennett T, Gage JC, Kinney WK. Benchmarking CIN 3+ risk as the basis for incorporating HPV and Pap cotesting into cervical screening and management guidelines. Journal of lower genital tract disease. 2013 Apr:17(5 Suppl 1):S28-35. doi: 10.1097/LGT.0b013e318285423c. Epub [PubMed PMID: 23519302]
Boyraz G, Basaran D, Salman MC, Ibrahimov A, Onder S, Akman O, Ozgul N, Yuce K. Histological Follow-Up in Patients with Atypical Glandular Cells on Pap Smears. Journal of cytology. 2017 Oct-Dec:34(4):203-207. doi: 10.4103/JOC.JOC_209_16. Epub [PubMed PMID: 29118475]
Geier CS, Wilson M, Creasman W. Clinical evaluation of atypical glandular cells of undetermined significance. American journal of obstetrics and gynecology. 2001 Jan:184(2):64-9 [PubMed PMID: 11174481]
Level 2 (mid-level) evidenceZhao C, Austin RM, Pan J, Barr N, Martin SE, Raza A, Cobb C. Clinical significance of atypical glandular cells in conventional pap smears in a large, high-risk U.S. west coast minority population. Acta cytologica. 2009 Mar-Apr:53(2):153-9 [PubMed PMID: 19365967]
Level 2 (mid-level) evidenceWang SS, Sherman ME, Hildesheim A, Lacey JV Jr, Devesa S. Cervical adenocarcinoma and squamous cell carcinoma incidence trends among white women and black women in the United States for 1976-2000. Cancer. 2004 Mar 1:100(5):1035-44 [PubMed PMID: 14983500]
Level 2 (mid-level) evidenceTakeuchi S. Biology and treatment of cervical adenocarcinoma. Chinese journal of cancer research = Chung-kuo yen cheng yen chiu. 2016 Apr:28(2):254-62. doi: 10.21147/j.issn.1000-9604.2016.02.11. Epub [PubMed PMID: 27198186]
Ki EY, Byun SW, Park JS, Lee SJ, Hur SY. Adenoma malignum of the uterine cervix: report of four cases. World journal of surgical oncology. 2013 Jul 26:11():168. doi: 10.1186/1477-7819-11-168. Epub 2013 Jul 26 [PubMed PMID: 23885647]
Level 3 (low-level) evidenceChang J, Zhang S, Zhou H, Liang JX, Lin ZQ. [Clinical analysis of minimal deviation adenocarcinoma of the cervix: a report of five cases]. Ai zheng = Aizheng = Chinese journal of cancer. 2008 Dec:27(12):1310-4 [PubMed PMID: 19080000]
Level 2 (mid-level) evidenceBalasubramaniam SD, Balakrishnan V, Oon CE, Kaur G. Key Molecular Events in Cervical Cancer Development. Medicina (Kaunas, Lithuania). 2019 Jul 17:55(7):. doi: 10.3390/medicina55070384. Epub 2019 Jul 17 [PubMed PMID: 31319555]
Yao YL, Tian QF, Cheng B, Cheng YF, Ye J, Lu WG. Human papillomavirus (HPV) E6/E7 mRNA detection in cervical exfoliated cells: a potential triage for HPV-positive women. Journal of Zhejiang University. Science. B. 2017 Mar.:18(3):256-262. doi: 10.1631/jzus.B1600288. Epub [PubMed PMID: 28271661]
Dick FA, Rubin SM. Molecular mechanisms underlying RB protein function. Nature reviews. Molecular cell biology. 2013 May:14(5):297-306. doi: 10.1038/nrm3567. Epub 2013 Apr 18 [PubMed PMID: 23594950]
Level 3 (low-level) evidenceMylavarapu S, Das A, Roy M. Role of BRCA Mutations in the Modulation of Response to Platinum Therapy. Frontiers in oncology. 2018:8():16. doi: 10.3389/fonc.2018.00016. Epub 2018 Feb 5 [PubMed PMID: 29459887]
Gibb RK, Martens MG. The impact of liquid-based cytology in decreasing the incidence of cervical cancer. Reviews in obstetrics & gynecology. 2011:4(Suppl 1):S2-S11 [PubMed PMID: 21617785]