Introduction
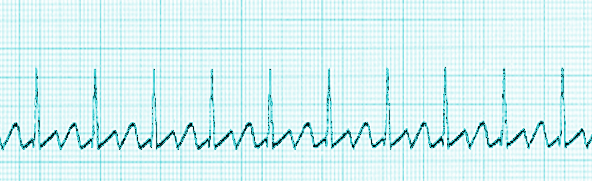
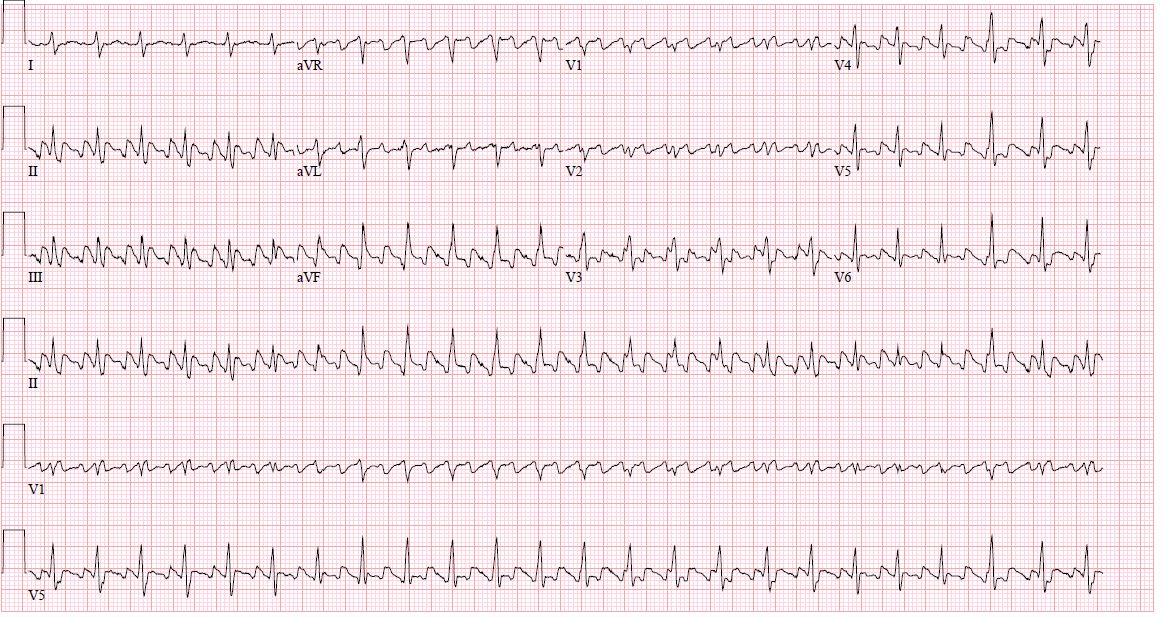
Supraventricular arrhythmias are a diverse group of atrial arrhythmias. Atrial fibrillation and atrial flutter are the most common of these atrial arrhythmias, and the other less common supraventricular arrhythmias are atrial tachycardias, atrioventricular reentrant tachycardia, atrioventricular nodal tachycardia, and others (see Image. Atrial Flutter, ECG). This topic summarizes the management of atrial flutter.
Atrial flutter is 1 of the most common arrhythmias. It is characterized by an abnormal cardiac rhythm that is fast, with an atrial rate of 300 beats/min and a ventricular rate that can be fixed or variable that can, causing palpitations, fatigue, syncope, and embolic phenomenon.[1]
Atrial flutter is a macro-reentrant tachycardia and, depending on the site of origin, can be a typical or atypical atrial flutter.[1] Electrocardiographic findings of atrial flutter are flutter waves without an isoelectric line between the QRS complex. The electrical axis of the flutter waves can help determine the atrial flutter's origin.
Typical or cavotricuspid isthmus (CTI) dependent is the most common type of atrial flutter; this rhythm originates in the right atrium at the level of the tricuspid valve annulus. Typical atrial flutter is seen in the electrocardiogram as continuous negative modulation in inferior leads (II, III, and AVF) and flat atrial deflections in leads I and aVL; this is due to the way of propagation and activation of the macro-reentrant circuit as described in the pathophysiology section.
The atypical atrial flutter is independent of the CTI, and the arrhythmia's origin can be in the right or left atrium. Less commonly, atrial activation can be clockwise; thus, electrocardiographic appearance is different; one cannot differentiate it easily from non-isthmus-dependent atrial flutter.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology behind atrial flutter is the presence of a re-entry mechanism for the initiation of the tachycardia. To have this electrical circuit, one must have the following elements:
- Areas with fast and slow velocities of conduction
- Different refractory periods
- A functional core where the circuit exists
These elements are present in a typical atrial flutter in the CTI. The initiation of atrial flutter is due to an ectopic beat that depolarizes 1 segment of the pathway of the circuits that become refractory and starts the tachycardia from a no-refractory segment.[2][3]
Epidemiology
Atrial flutter is the second most common cardiac arrhythmia after atrial fibrillation.[4] It is commonly associated with atrial fibrillation, but the incidence and the prevalence of the atrial flutter are less known when compared with atrial fibrillation.[4] Atrial flutter in common in patients with underlying diseases such as chronic obstructive pulmonary disease, pulmonary hypertension, and heart failure. Isolated atrial flutter in the absence of abnormal heart anatomy is rare and usually occurs when atrial size abnormalities have developed.[5] Atrial flutter is more frequent in males than in females. Aging is a significant risk factor as other associated disorders in patients with atrial fibrillation include systemic hypertension, diabetes mellitus, and a history of alcohol abuse. Older age is associated with an increased risk of atrial fibrillation and atrial flutter.
Pathophysiology
Typical Atrial Flutter
Typical atrial flutter is the most common type of atrial flutter and is a macroreentrant atrial tachycardia that uses the CTI as an essential part of the circuit. The Todaro tendon, crista terminalis, the inferior vena cava, the tricuspid valve annulus, and the coronary sinus os delineate the circuit. These structures are essential to provide the pathway length for the flutter system.
The CTI provides the slow conduction pathway, which is present in the lateral aspect of the younger patients and the medial aspect in the older patients. The mechanism of slow conduction is not well understood but might be related to anisotropic fiber orientation. With aging and atrial dilation, atrial tissue fibrosis occurs and produces non-uniform anisotropic conduction through the CTI.
The crista terminalis is a functional barrier that induces a transverse conduction block, steep slope, and arborization, allowing the circuit to exist.
The arrhythmia mechanism is a macro-reentry activation of the right atrium from the interatrial septum and along the crista terminalis with passive activation of the left atrium via the coronary sinus muscular connection.[6][7]
As this cycle occurs in the atrium, conduction is determined by the atrioventricular node mechanism to conduct the atrial impulse. Commonly, the atrioventricular conduction is 2 to 1 with an atrial rate of 300 beats per minute with a ventricular rate of 150 beats per minute, but this can be variable depending on the underlying parasympathetic stimulus or refractoriness of the atrioventricular node.
The absence of an isoelectric line between P waves or QRS complexes is due to the constant cycling of the circuit or atrial activation.
The reason behind the circuit's existence might relate to the nature of the anatomical structures circumscribing the circuit. The crista terminalis thickness might have the capacity to block conduction, and the low voltage of the CTI can be a sign of arrhythmogenesis and poor conduction in the right atrium.
Atypical Atrial Flutter
Atypical atrial flutter or other macroreentrant atrial tachycardia has a circuit configuration different from the typical right atrial flutter circuit. Electrophysiologic studies and intracardiac mapping are the only means to determine the exact mechanism or area generating the atrial flutter. Unlike typical atrial flutter, atypical atrial flutter is related to structural heart diseases such as prior cardiac surgery or ablation procedures.[8]
When the atrial flutter is determined to come from the right atrium but not associated with the CTI system, the circuit can be in the superior vena cava and part of the terminal crest. When prior surgery or intervention occurs, the presence of a scar can often become arrhythmogenic, and the center of the circuit and the onset of the arrhythmia mostly occur after several years of the procedure, likely secondary to remodeling.[9]
In patients without cardiac intervention, the atrial flutter circuit can be low voltage areas like the lateral right atrium.[10] This might be secondary to fibrosis due to chronic atrial high pressures or cardiomyopathy that can produce fibrosis of the myocardium and create low-voltage areas that allow atrial flutter.[10] Left atrial flutter can be associated with surgical atriotomy scars or areas of prior ablations combined with areas of low voltage.[11]
Electrophysiologic studies and mapping of the right and left atrium are necessary to determine the specific location and mechanism of the arrhythmia to guide the ablation. In an intra-atrial septal macro-reentrant system, the success rate is low compared to the free-wall atrial tachycardias.[12]
History and Physical
Patients with atrial flutter can be asymptomatic or present with symptoms such as palpitations, lightheadedness, fatigue, and shortness of breath, especially in the presence of rapid ventricular conduction. Decreased exercise tolerance is another symptom that can be present during patient evaluation. During the rapid ventricular rate, hypotension, syncope, and near syncope can occur in susceptible patients with high ventricular rates. Some patients remain asymptomatic until they develop acutely decompensated heart failure, tachycardia-induced cardiomyopathy, and embolic stroke. The physical exam in patients with atrial flutter shows regular or irregularly regular peripheral pulse (due to variable conduction from the atrioventricular node), jugular venous distension, respiratory sounds with crackles in lung fields, tachycardia, abdominal distention, and lower extremities edema when congestion occurs.
Evaluation
Initial evaluation of the underlying rhythm is necessary, and determination of possible etiology or trigger is crucial.
Electrocardiogram:
Electrocardiogram generally shows flutter waves with the absence of an isoelectric line between QRS complexes, with an atrial wave around 300 beats per minute with ventricular conduction that can be 2 to 1, 3 to 1 or 4 to 1 or with variable conduction due to Wenckebach phenomenon. See Image. Atrial Flutter.
In inferior leads, typical flutter waves resemble a picket fence or sawtooth because the P waves are negative due to the direction of the vector. Typical atrial flutter with counterclockwise activation shows inferior leads with negative flutter waves with low amplitude in the lead I and upright flutter waves in aVL.[9]
Echocardiogram
Echocardiography for evaluating atrial flutter bases its value on determining underlying structural heart disease. The presence of dilated atrial chambers is a sign of chronicity and fibrosis of the atrium that could make the circuit persist and more challenging to control.[13]
Assessment of left ventricular ejection fraction can be the cause or consequence of underlying atrial flutter because the persistence of tachycardia can generate tachycardia induced-cardiomyopathy, or cardiomyopathy and volume status can trigger the atrial flutter. Evaluating atrial or ventricular thrombus is also important, especially when desiring cardioversion to sinus rhythm. A transesophageal echocardiogram is the modality of choice because it can visualize the atrial appendage where atrial thrombus is more frequently present.[14]
Laboratory evaluation
An initial determination of atrial flutter triggers is necessary. Laboratory evaluation of electrolyte disturbance, abnormal thyroid function, infection, anemia, and hypoxia. Correction of these abnormalities can improve symptoms and decrease the threshold of atrial flutter and rapid ventricular response development. A pulmonary function test might be necessary for this set of patients; there is a correlation between lung disease and the presence of atrial arrhythmias, including atrial flutter. Management of the underlying lung condition can improve the control of the atrial flutter.
Treatment / Management
Treatment management should focus on the following aspects:
- Rhythm control
- Rate control
- Anticoagulation due to embolization risk
Rhythm control
- Maintenance of the sinus rhythm or conversion of the sinus rhythm is essential.
- Persistence of atrial flutter can cause chronic remodeling of the atrium, making it more difficult to manage the rate and the conversion or maintenance of sinus rhythm.
- There are different ways to achieve sinus rhythm: electrical cardioversion, pharmacological cardioversion, and catheter ablation.
- The rhythm strategy is divided into acute and long-term management.
- In the acute setting, in patients with atrial flutter who are hemodynamically unstable, synchronized cardioversion is indicated for the conversion of sinus rhythm to stabilize the patient.[15]
- In stable patients, pharmacological cardioversion is achievable with different antiarrhythmics. Antiarrhythmic drugs like amiodarone, class IA (procainamide, quinidine, and disopyramide), IC drugs (flecainide and propafenone), calcium channel blockers (verapamil, diltiazem), and beta-blockers (metoprolol, carvedilol, esmolol) are some of the choices for pharmacological cardioversion.[16]
- Despite the multiple pharmacological options, controlling and converting atrial flutter to sinus rhythm is difficult. The mechanism by which antiarrhythmic drugs maintain sinus rhythm is the prevention of premature beats that usually start the activation of the tachycardia circuit by a reentrant or an ectopic beat.
- In the presence of a new diagnosis of atrial flutter, one should start the patient on anticoagulation. In the absence of an intracardiac thrombus, electrical cardioversion in stable patients can be considered, especially to prevent the persistence of the arrhythmia and further fibrosis that perpetuates the presence of atrial flutter and is more difficult to control or to convert to sinus rhythm.[17]
- Patients who have a contraindication to these drugs or do not tolerate them may consider catheter ablation of the atrial flutter circuit.[18]
- Radiofrequency catheter ablation of the CTI is the standard treatment for typical atrial flutter with a success rate of 95% and few complications post-procedure.[19] The procedure involves placing intracardiac catheters into the coronary sinus, the atrium, and an ablation catheter. The anatomical target for the CTI is found through a mapping and entrapment technique. After this, the linear lesion is made by the ablation catheter with the use of radiofrequency energy. At the end of the ablation, when the line is complete, verification of bidirectional conduction block and absence of atrial flutter is done to confirm ablation is complete. In the rare cases of medication and ablation failure, atrioventricular nodal ablation with the placement of a pacemaker might be indicated to prevent atrial to ventricular conduction of rapid atrial flutter. (A1)
Rate control
- Rate control is achievable using atrioventricular nodal agents such as calcium channel blockers (first line) or beta blockers.[20] Digoxin is another option for rate control but needs to be used carefully due to its side effects and toxicity.
- A combination of these agents is an option.
- Adequate control of the atrial flutter through AV nodal agents is difficult because the atrial flutter continuously fires at the same rate as the AV node.
- The heart rate goal should be below 110 beats per minute.[21] This was determined after the RACE II trial (Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II). This study compared strict heart rate control of <80 bpm versus < 110 bpm; this study showed that very stringed heart rate control is unnecessary, and more lenient control reduces polypharmacy, fewer side effects, and fewer outpatient visits. This study was conducted on patients with atrial flutter, but it can be extrapolated to the rate control of atrial flutter.
- In patients who are intolerant of medications or have significant bradycardia due to rate control measures, catheter ablation is an option. (A1)
Anticoagulation due to the risk of embolic events:
- Patients with atrial flutter have a similar risk of strokes as those with atrial fibrillation.[22]
- Use of a scoring system to determine the annual risk of stroke must be used, such as the CHADS2-Vasc.[23] This scoring system helps to risk stratify the patient according to their risk of developing embolic strokes due to atrial flutter or atrial fibrillation. The presence of congestive heart failure, systemic hypertension, diabetes, female sex, age between 65 to 74 years, and a history of peripheral vascular disease score 1 point for each comorbidity that is present.
- Age more than 75 years old and a history of stroke are 2 additional points each.
- The presence of 1 point can give the patient an annual risk of 1.3% of embolic stroke per year; with 2 points, the risk is 2.2%. In patients with 2 or more points, anticoagulation is a strong recommendation. In patients with 1 point, one may use either aspirin or full anticoagulation. (B2)
Differential Diagnosis
The differential diagnoses for atrial flutter include the following:
- Atrial fibrillation: mostly irregular, no evidence of organized atrial activity in the electrocardiogram, absence of P waves
- Multifocal atrial tachycardia: multiple P waves morphology due to the presence of several atrial pacers
- Atrial tachycardia with variable conduction: the isoelectric line between QRS complexes
Prognosis
The prognosis of patients with typical atrial flutter undergoing catheter ablation is good, with a recurrence rate of less than 5%. The persistence of atrial flutter can generate tachycardia and induce cardiomyopathy that is hard to control, causing multiple hospitalizations due to decompensation.
Complications
The most common complication of atrial flutter is the increased risk of embolic stroke and disability related to this event. Hemodynamic instability is also possible, especially in patients with a rapid ventricular response. Chronicity and poor control of atrial flutter can generate tachycardia, induce cardiomyopathy, and also produce hard-to-control heart failure. The complications secondary to the use of antiarrhythmic drugs are related to the drug and underlying mechanism of the drug.
Atrial flutter ablation complications also depend on the side of the origin of the atrial flutter. Right-sided atrial flutter is related to fewer complication rates than left-sided atrial flutter ablation, and this is due to the need for creating a transeptal communication during the procedure to reach the left atrium foci of arrhythmia and perform the ablation. The transseptal puncture produces transient communication between the left and right chambers of the heart. There is also an increasing risk of embolic strokes with left-sided atrial flutter ablation when compared with right-side procedures.
Enhancing Healthcare Team Outcomes
There is no cure for atrial flutter, and the disorder is known to be associated with a high risk of a stroke and other embolic phenomena; the management of atrial flutter is best done by an interprofessional team including physicians, specialists, pharmacists, and a cardiac specialty nurse is recommended. While the cardiologist may initiate the initial treatment, most patients are followed by the primary provider or nurse practitioner. These patients need life-long follow-up because there is a risk of an embolic stroke. If the disorder receives inadequate therapy, it leads to a poor quality of life.
Primary care providers, pharmacists, and nurse practitioners should enforce medication compliance. Those patients on warfarin should have a dietary consult because a sudden change in the consumption of green leafy vegetables can affect the INR. The hematology nurse and pharmacist should monitor the INR, but the clinician should adjust the warfarin dose.
An ECG should be performed at each clinic visit, and the patient should be examined for any embolic phenomenon. To improve outcomes, open communication between interprofessional team members is essential.
Outcomes
Despite advances in treatment, recurrence and multiple admission to the hospital are very common.
Media
References
Bun SS, Latcu DG, Marchlinski F, Saoudi N. Atrial flutter: more than just one of a kind. European heart journal. 2015 Sep 14:36(35):2356-63. doi: 10.1093/eurheartj/ehv118. Epub 2015 Apr 2 [PubMed PMID: 25838435]
Matsuo K, Uno K, Khrestian CM, Waldo AL. Conduction left-to-right and right-to-left across the crista terminalis. American journal of physiology. Heart and circulatory physiology. 2001 Apr:280(4):H1683-91 [PubMed PMID: 11247780]
Level 3 (low-level) evidenceWatson RM, Josephson ME. Atrial flutter. I. Electrophysiologic substrates and modes of initiation and termination. The American journal of cardiology. 1980 Apr:45(4):732-41 [PubMed PMID: 7361663]
Granada J, Uribe W, Chyou PH, Maassen K, Vierkant R, Smith PN, Hayes J, Eaker E, Vidaillet H. Incidence and predictors of atrial flutter in the general population. Journal of the American College of Cardiology. 2000 Dec:36(7):2242-6 [PubMed PMID: 11127467]
Level 2 (mid-level) evidenceHalligan SC, Gersh BJ, Brown RD Jr, Rosales AG, Munger TM, Shen WK, Hammill SC, Friedman PA. The natural history of lone atrial flutter. Annals of internal medicine. 2004 Feb 17:140(4):265-8 [PubMed PMID: 14970149]
Level 2 (mid-level) evidenceKlein GJ, Guiraudon GM, Sharma AD, Milstein S. Demonstration of macroreentry and feasibility of operative therapy in the common type of atrial flutter. The American journal of cardiology. 1986 Mar 1:57(8):587-91 [PubMed PMID: 3953444]
Level 3 (low-level) evidenceKalman JM, Olgin JE, Saxon LA, Lee RJ, Scheinman MM, Lesh MD. Electrocardiographic and electrophysiologic characterization of atypical atrial flutter in man: use of activation and entrainment mapping and implications for catheter ablation. Journal of cardiovascular electrophysiology. 1997 Feb:8(2):121-44 [PubMed PMID: 9147698]
Tai CT, Chen SA. Electrophysiological mechanisms of atrial flutter. Journal of the Chinese Medical Association : JCMA. 2009 Feb:72(2):60-7. doi: 10.1016/S1726-4901(09)70024-3. Epub [PubMed PMID: 19251532]
Level 3 (low-level) evidenceCosío FG. Atrial Flutter, Typical and Atypical: A Review. Arrhythmia & electrophysiology review. 2017 Jun:6(2):55-62. doi: 10.15420/aer.2017.5.2. Epub [PubMed PMID: 28835836]
Kall JG, Rubenstein DS, Kopp DE, Burke MC, Verdino RJ, Lin AC, Johnson CT, Cooke PA, Wang ZG, Fumo M, Wilber DJ. Atypical atrial flutter originating in the right atrial free wall. Circulation. 2000 Jan 25:101(3):270-9 [PubMed PMID: 10645923]
Jaïs P, Shah DC, Haïssaguerre M, Hocini M, Peng JT, Takahashi A, Garrigue S, Le Métayer P, Clémenty J. Mapping and ablation of left atrial flutters. Circulation. 2000 Jun 27:101(25):2928-34 [PubMed PMID: 10869265]
Coffey JO, d'Avila A, Dukkipati S, Danik SB, Gangireddy SR, Koruth JS, Miller MA, Sager SJ, Eggert CA, Reddy VY. Catheter ablation of scar-related atypical atrial flutter. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2013 Mar:15(3):414-9. doi: 10.1093/europace/eus312. Epub 2013 Feb 5 [PubMed PMID: 23385050]
Level 2 (mid-level) evidenceHöglund C, Rosenhamer G. Echocardiographic left atrial dimension as a predictor of maintaining sinus rhythm after conversion of atrial fibrillation. Acta medica Scandinavica. 1985:217(4):411-5 [PubMed PMID: 3160222]
Verhorst PM, Kamp O, Welling RC, Van Eenige MJ, Visser CA. Transesophageal echocardiographic predictors for maintenance of sinus rhythm after electrical cardioversion of atrial fibrillation. The American journal of cardiology. 1997 May 15:79(10):1355-9 [PubMed PMID: 9165157]
Gallagher MM, Guo XH, Poloniecki JD, Guan Yap Y, Ward D, Camm AJ. Initial energy setting, outcome and efficiency in direct current cardioversion of atrial fibrillation and flutter. Journal of the American College of Cardiology. 2001 Nov 1:38(5):1498-504 [PubMed PMID: 11691530]
Level 2 (mid-level) evidenceBianconi L, Castro A, Dinelli M, Alboni P, Pappalardo A, Richiardi E, Santini M. Comparison of intravenously administered dofetilide versus amiodarone in the acute termination of atrial fibrillation and flutter. A multicentre, randomized, double-blind, placebo-controlled study. European heart journal. 2000 Aug:21(15):1265-73 [PubMed PMID: 10924317]
Level 1 (high-level) evidenceVan Gelder IC, Crijns HJ, Van Gilst WH, Verwer R, Lie KI. Prediction of uneventful cardioversion and maintenance of sinus rhythm from direct-current electrical cardioversion of chronic atrial fibrillation and flutter. The American journal of cardiology. 1991 Jul 1:68(1):41-6 [PubMed PMID: 2058558]
Pytkowski M, Jankowska A, Kraska A, Sterliński M, Kowalik I, Krzyzanowski W, Szwed H. [Pharmacological versus invasive treatment in patients with atrial fibrillation]. Polskie Archiwum Medycyny Wewnetrznej. 2004 Jun:111(6):703-7 [PubMed PMID: 15508793]
Level 1 (high-level) evidenceSaoudi N, Atallah G, Kirkorian G, Touboul P. Catheter ablation of the atrial myocardium in human type I atrial flutter. Circulation. 1990 Mar:81(3):762-71 [PubMed PMID: 2306828]
Shah SR, Luu SW, Calestino M, David J, Christopher B. Management of atrial fibrillation-flutter: uptodate guideline paper on the current evidence. Journal of community hospital internal medicine perspectives. 2018:8(5):269-275. doi: 10.1080/20009666.2018.1514932. Epub 2018 Oct 15 [PubMed PMID: 30357020]
Level 3 (low-level) evidenceSmit MD, Crijns HJ, Tijssen JG, Hillege HL, Alings M, Tuininga YS, Groenveld HF, Van den Berg MP, Van Veldhuisen DJ, Van Gelder IC, RACE II Investigators. Effect of lenient versus strict rate control on cardiac remodeling in patients with atrial fibrillation data of the RACE II (RAte Control Efficacy in permanent atrial fibrillation II) study. Journal of the American College of Cardiology. 2011 Aug 23:58(9):942-9. doi: 10.1016/j.jacc.2011.04.030. Epub [PubMed PMID: 21851883]
Level 1 (high-level) evidenceLanzarotti CJ, Olshansky B. Thromboembolism in chronic atrial flutter: is the risk underestimated? Journal of the American College of Cardiology. 1997 Nov 15:30(6):1506-11 [PubMed PMID: 9362409]
Level 2 (mid-level) evidenceFuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Zamorano JL, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, American College of Cardiology, American Heart Association, European Society of Cardiology. [ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation--excutive summary]. Revista portuguesa de cardiologia : orgao oficial da Sociedade Portuguesa de Cardiologia = Portuguese journal of cardiology : an official journal of the Portuguese Society of Cardiology. 2007 Apr:26(4):383-446 [PubMed PMID: 17695733]