Introduction
Alveolar osteitis (AO), most commonly known as "dry socket," is one of the most common complications after exodontia. The incidence is most commonly reported between 0.5% and 5%, but some studies have noted it as high as 68%.[1][2]
The condition is characterized by prolonged moderate to severe pain at the site of tooth extraction. This can result in multiple visits for management and symptom relief. The cause is widely believed to be the fibrinolytic theory. The extraction socket is characterized by an area of the exposed bone secondary to the absence of a fibrin clot or loss of clot after formation.[2]
Although alveolar osteitis is a common complication, there is still some uncertainty about the pathophysiology. This has led to several proposed prevention and management strategies, but there is currently no evidence-based consensus.[3] This article aims to explore the risk factors and therapeutic interventions that have been recommended.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Despite the longstanding awareness of this condition, the etiology of alveolar osteitis is not fully understood. It is most commonly noted as a premature fibrinolytic breakdown of the early platelet clot, exposing the underlying bone in the extraction socket.
Birn first hypothesized in 1973 that AO develops from a complete absence of a blood clot or development of an initial clot that is successively lysed soon after creation.[1] Breakdown of the clot results from the plasminogen pathway activation, but the trigger is unknown. Either physiologic or non-physiologic mediators produce the activator substance. Many specific factors have been investigated and debated. Although there is still a poor understanding, all have a promotor effect on clot lysis leading to fibrinolysis.[4]
The immune system's response to tooth extraction is comparable to any other tissue trauma. The inflammatory response in the alveolus involves pro-and anti-inflammatory cytokines. Studies have primarily focused on the effects of IL-6. IL-6 has a dual role in bone formation and bone resorption, which could contribute to the fibrinolysis in alveolar osteitis.[5]
Investigating biomarkers such as tumor necrosis factor-alpha (TNF-a), osteocalcin, and runt-related transcription factor 2 has also been suggested. These physiologic mediators could help create an enhanced understanding of the pathologic process of alveolar osteitis.[6]
Focal fibrinolytic activity influenced by bacteria has also been investigated. The microbiota in alveolar osteitis was significantly different from the patients who presented without postoperative complications. Prevotella, Fusobacterium, Parvimonas, and Peptostreptococcus were the most common bacteria detected in patients with alveolar osteitis in one systematic review.[7]
Another found Treponema denticola, a known red-complex periodontal pathogen, could be a likely culprit in the pathogenesis of AO. For a bacteria to be a causative agent of alveolar osteitis, it needs to be capable of fibrinolysis but must not induce swelling, purulence, or erythema. They must also be isolated from a post-extraction socket and conducive to proliferation. These bacteria thrive with poor oral hygiene. The bacteria are limited to the bone's surface, and thus alveolar osteitis is not categorized as a true infectious process.
Epidemiology
The incidence of alveolar osteitis varies significantly in current literature, reported between 0.5% and 68%. Studies with larger patient populations trend towards a lower incidence, commonly less than 5%.[1][2][5] Multiple systematic reviews found that around 30% of mandibular third molar extractions develop alveolar osteitis.[8]
There is a significantly higher incidence of alveolar osteitis in lower third molars than in all other dental extraction sites combined. The alveolus of posterior mandibular teeth, specifically the third molars, has greater vascularity when compared to the anterior teeth. This finding contradicts the belief that alveolar osteitis is triggered by a lack of blood supply, which is the most common hypothesis to explain why alveolar osteitis is much less common in the maxilla.[4]
Although there is conflicting data, many studies found that patient age and female gender increased the incidence of alveolar osteitis. The prevalence was similar worldwide, and there were no documented differences in ethnicity.[2][5][9]
Many studies show a statistically significant increase in alveolar osteitis in female patients taking oral contraceptive pills or mid-menstrual cycle, explaining the higher incidence of alveolar osteitis in females. The increased incidence of alveolar osteitis in patients taking oral contraceptives is likely a result of decreased levels of plasminogen activator inhibitor and increased levels of plasminogen. This results in increased fibrinolysis and supports Birn’s fibrinolytic theory.[2]
Several other risk factors for developing AO have been investigated, including tobacco use, poor oral hygiene, lack of operator experience, flap design, and difficulty of extraction. These factors have support in multiple publications, but the role of most others has not been demonstrated.[2][4]
History and Physical
The cardinal symptom of alveolar osteitis is radiating pain that increases in intensity after tooth extraction. The pain is at, or near, the extraction socket in the trigeminal nerve distribution. It typically occurs between one and five days post-operatively and is unrelieved by analgesics.[4][3] Halitosis is also commonly reported.[1]
Physical examination is unremarkable mainly. Expected postoperative changes, such as erythema and edema, can be anticipated, but there should be no frank signs of infection. Rarely a low-grade fever or regional lymphadenopathy can be noted.[4]
Vital signs are stable, and the patient is most commonly afebrile. The pain is accompanied by a totally or partially broken down blood clot in the alveolar socket. Exposed bone secondary to this fibrinolysis is the typical clinical presentation but may be difficult to visualize on examination.[3]
Evaluation
An increase in pain intensity a few days after a tooth extraction is the key feature. The absence of a blood clot and moderate to severe pain is pathognomonic of alveolar osteitis, and additional laboratory and radiographic studies are not required. As alveolar osteitis is not an infection but a delayed healing process, no leukocytosis would be expected.
Post-operative imaging, such as a panoramic radiograph, could rule out remaining tooth fragments or bony sequestra. Markers of fibrinolysis have been investigated for risk prediction in cardiovascular disease but are not helpful in a clinical setting with AO.[10]
Treatment / Management
Much of the current discussion regarding AO focuses on treatment strategies, but no consensus protocols have been developed. One systematic review concluded there was insufficient evidence to support any management strategies for established AO.[3] Management focuses on symptom relief rather than any particular disease process.(A1)
The initial management strategy for alveolar osteitis with the most support is intra-alveolar irrigation, which removes necrotic tissue and clot debris and reduces the bacterial load. Intra-alveolar irrigation alone may not relieve pain but should complement the other outlined strategies. It is commonly included in studies as an early measure, and curettage of the dry socket is not recommended as it will expose the bone further.
Topical local anesthetic gels can relieve pain shortly after irrigation, and long-acting local anesthetics can provide immediate symptom relief. Local anesthetics can be supplemented with oral analgesics, primarily non-steroidal anti-inflammatory drugs (NSAIDs).
Multiple interventions include placing a medicated dressing into the extraction socket at the time of surgery or post-operatively. Some common options are zinc oxide eugenol or other obtundent dressings that include compounds with analgesic or antibacterial action.
Multiple studies support the success of these interventions, but many dressings have to be removed from the alveolus to prevent foreign body reactions. They also slow the healing process.[8] Hyaluronic acid placement after irrigation has also shown success in reducing pain and inflammation.[2](A1)
Rinsing with chlorhexidine mouthwashes and placing chlorhexidine gels into the extraction socket have also shown treatment success. Many studies explore chlorhexidine as a preventive measure, but resolution after AO development has also been investigated.[8][11] (A1)
Although some studies show AO can be successfully managed by chlorhexidine, there is not as much support for treatment as there is for prevention. There is still insufficient evidence to recommend chlorhexidine as a treatment to relieve established AO.
Platelet-rich fibrin (PRF) has also been investigated. One study found that pain reduction was similar to irrigation alone, but the soft tissue healing was improved. PRF is more commonly used as a preventive measure, and the efficacy of using it as a treatment is debatable.
Recent evidence suggests that phototherapy, specifically low-level laser therapy (LLLT), has a role in symptom management. It is easy to use, quick, relatively safe, and financially advantageous. The results are comparable to all the alternative management strategies above, and many studies find the results superior. Photobiomodulation therapy has been shown to have a higher ability to decrease pain and is considered by some to be the most effective intervention available.[12] (A1)
Low-level laser therapy (LLLT) is a newer technology, and further evaluation is needed, but it could become a mainstay of treatment in the future.
Differential Diagnosis
Alveolar osteitis can be assumed when a patient presents within the first week after extractions with severe pain. Depending on the severity of the pain, it could be classified as normal post-operative discomfort or be a result of food debris impaction.
Treatment with intra-alveolar irrigation is indicated with any of the above diagnoses. Some sources contend that pain beyond a week from surgery is not consistent with alveolar osteitis, and others state that persistent pain longer than three weeks necessitates a different diagnosis.[4][1]
The primary differential diagnosis that needs to be considered is an infection, mainly if there are signs of disease beyond the extraction socket. Symptoms consistent with alveolar osteitis presenting or persisting weeks after surgery are concerning for acute osteomyelitis, subperiosteal infection, or bony sequestra formation. Based on the clinical evaluation of the patient, it may be appropriate to obtain a panoramic radiograph to evaluate healing.
Prognosis
Since alveolar osteitis is self-limiting, the prognosis is excellent. If the diagnosis is correct, it will resolve within days after initiating treatment.[4] Even without treatment, the course will be short, and it does not cause any long-term morbidity.[1]
Complications
There is no evidence that alveolar osteitis can result in additional complications. After resolution, the extraction socket heals as it does in patients who did not experience AO. There is no peer-reviewed literature correlating it with an increased risk of other complications associated with dental extractions.[1]
Chlorhexidine usage, the prevention strategy with the most support, does have some rare but serious adverse effects. The primary concern with chlorhexidine is hypersensitivity reactions, and there have been multiple documented cases of minor adverse reactions after irrigation of an AO socket with chlorhexidine mouthwash.
There are two case reports from the United Kingdom of fatal adverse events related to chlorhexidine used in intra-alveolar irrigation secondary to hypersensitivity reactions. The dental practitioners who prescribe or administer this medication should be aware of potential hypersensitivity and educate their patients on minor and severe adverse side effects.[8]
Another known complication of alveolar osteitis treatment is possible foreign body reactions. The delivery vehicles of the intra-socket medicaments delay healing and can cause this reaction.[4] This results from granulomatous inflammation and the body's inability to phagocytose foreign materials. Therefore, obtundent dressings should be removed to prevent this from happening. Many authors will discourage the use of topical medicaments for this reason.[8]
Deterrence and Patient Education
Prevention is based on knowledge of the risk factors and available prophylactic agents. Although there is some debate about the risk factors discussed above, the practitioner should educate the patient about mitigating the risk of alveolar osteitis. Smoking cessation is something all patients should consider to deter several complications, including AO. Females should also be aware that their risk can increase, especially if they are taking oral contraceptives.[4] Controlling factors such as these could reduce the incidence of AO. Detailed post-operative instructions are always recommended, but this has been investigated, and there was no significant decrease in AO rate even when given.
The prophylactic measure with the most support is the use of chlorhexidine. One study demonstrated that chlorhexidine mouthwash following dental extractions reduced AO incidence by 63%.[13] Chlorhexidine gels were also effective in preventing alveolar osteitis in another meta-analysis.[14] The formulation, concentration, and regimen of chlorhexidine have been investigated, and the gel was found to be moderately more efficacious; however, all were shown to prevent AO.[15]
One systematic review did find the use of chlorhexidine to be safe without any significant adverse reactions. Still, it concluded the evidence was insufficient to support its use to prevent AO.[16] Overall, a preponderance of evidence points towards chlorhexidine in any formulation as a safe and effective method to reduce AO incidence.
A systematic review concluded that all other preventative interventions for alveolar osteitis lack sufficient evidence to support their use. Yet platelet-rich fibrin (PRF) is an effective preventive measure in many studies. One randomized controlled trial concluded that PRF in combination with chlorhexidine was the intervention that effectively reduced AO incidence.
Most other interventions have conflicting results, but saline irrigation post-operatively is largely beneficial. Warm saline mouth baths were shown to reduce post-operative complications, including AO. New studies were recommended to establish a standardized protocol to maximize their effectiveness.[17]
Current guidelines have also discouraged the prevention and treatment of alveolar osteitis with the prescription of oral antibiotics. Perioperative antibiotics have some support in reducing infection after dental extractions, but there is poor support for their use with AO. Even in studies that show a minimal reduction or improvement in AO, it is often not statistically significant, and minor adverse reactions to antibiotics are likely. Antibiotics are not indicated for routine extractions in immunocompetent patients.[11]
Enhancing Healthcare Team Outcomes
Alveolar osteitis is a painful, debilitating condition and one of the most common complications after tooth extraction. There is no consensus on the criteria used for diagnosis. Patients exhibit non-specific signs and symptoms such as pain not relieved by analgesics, halitosis, necrotic debris, or a disintegrated blood clot within the alveolus.[16] This poses a diagnostic dilemma, but providers should treat patients for alveolar osteitis if at all suspicious of the condition.
While oral and maxillofacial surgeons are often involved in these patients' care, other providers should also be adept at treating this condition. Patients are likely to also present to general dentistry offices and occasionally even to primary care or emergency medicine physicians. Interprofessional communication is essential to enhance patient-centered care and improve outcomes.
Although there is still debate regarding the most effective strategies for prevention and management of AO, chlorhexidine is the intervention with the most support. That recommendation was developed after an exhaustive review of the current medical literature from peer-reviewed journals and included large randomized clinical trials and systematic reviews.[8] [Level I]
Media
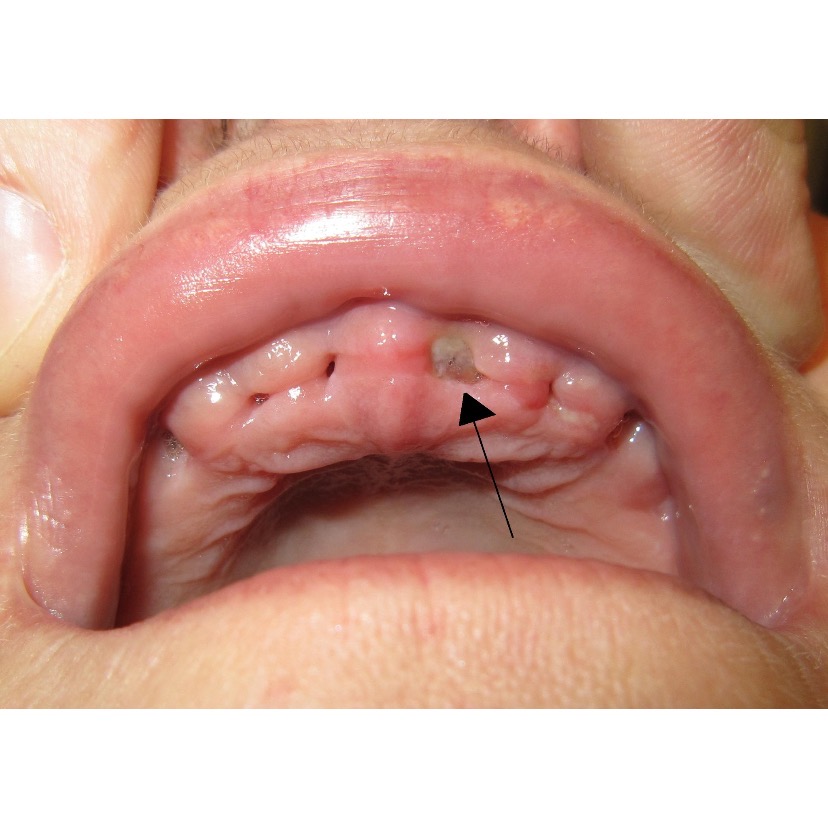
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Chow O, Wang R, Ku D, Huang W. Alveolar Osteitis: A Review of Current Concepts. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2020 Aug:78(8):1288-1296. doi: 10.1016/j.joms.2020.03.026. Epub 2020 Apr 5 [PubMed PMID: 32348729]
Ghosh A, Aggarwal VR, Moore R. Aetiology, Prevention and Management of Alveolar Osteitis-A Scoping Review. Journal of oral rehabilitation. 2022 Jan:49(1):103-113. doi: 10.1111/joor.13268. Epub 2021 Oct 22 [PubMed PMID: 34625985]
Level 2 (mid-level) evidenceGarola F, Gilligan G, Panico R, Leonardi N, Piemonte E. Clinical management of alveolar osteitis. A systematic review. Medicina oral, patologia oral y cirugia bucal. 2021 Nov 1:26(6):e691-e702. doi: 10.4317/medoral.24256. Epub 2021 Nov 1 [PubMed PMID: 34704976]
Level 1 (high-level) evidenceKrakowiak PA, Alveolar osteitis and osteomyelitis of the jaws. Oral and maxillofacial surgery clinics of North America. 2011 Aug; [PubMed PMID: 21798440]
Øyri H, Jensen JL, Barkvoll P, Jonsdottir OH, Reseland J, Bjørnland T. Incidence of alveolar osteitis after mandibular third molar surgery. Can inflammatory cytokines be identified locally? Acta odontologica Scandinavica. 2021 Apr:79(3):205-211. doi: 10.1080/00016357.2020.1817546. Epub 2020 Sep 8 [PubMed PMID: 32898447]
Zahid T, Ghafoor S. Molecular events in the clinicopathological diagnosis of alveolar osteitis. JPMA. The Journal of the Pakistan Medical Association. 2021 Feb:71(2(A)):508-513. doi: 10.47391/JPMA.491. Epub [PubMed PMID: 33819239]
Riba-Terés N, Jorba-García A, Toledano-Serrabona J, Aguilar-Durán L, Figueiredo R, Valmaseda-Castellón E. Microbiota of alveolar osteitis after permanent tooth extractions: A systematic review. Journal of stomatology, oral and maxillofacial surgery. 2021 Apr:122(2):173-181. doi: 10.1016/j.jormas.2020.08.007. Epub 2020 Sep 5 [PubMed PMID: 32896676]
Level 1 (high-level) evidenceDaly B, Sharif MO, Newton T, Jones K, Worthington HV. Local interventions for the management of alveolar osteitis (dry socket). The Cochrane database of systematic reviews. 2012 Dec 12:12():CD006968. doi: 10.1002/14651858.CD006968.pub2. Epub 2012 Dec 12 [PubMed PMID: 23235637]
Level 1 (high-level) evidenceSigron GR, Pourmand PP, Mache B, Stadlinger B, Locher MC. The most common complications after wisdom-tooth removal: part 1: a retrospective study of 1,199 cases in the mandible. Swiss dental journal. 2014:124(10):1042-6, 1052-6 [PubMed PMID: 25342545]
Level 2 (mid-level) evidenceChoi BG, Vilahur G, Ibanez B, Zafar MU, Rodriguez J, Badimon JJ. Measures of thrombosis and fibrinolysis. Clinics in laboratory medicine. 2006 Sep:26(3):655-78, vii [PubMed PMID: 16938589]
Cho H,Lynham AJ,Hsu E, Postoperative interventions to reduce inflammatory complications after third molar surgery: review of the current evidence. Australian dental journal. 2017 Dec; [PubMed PMID: 28498604]
Shafaee H, Bardideh E, Nazari MS, Asadi R, Shahidi B, Rangrazi A. The effects of photobiomodulation therapy for treatment of alveolar osteitis (Dry Socket): Systematic review and meta-analysis. Photodiagnosis and photodynamic therapy. 2020 Dec:32():102000. doi: 10.1016/j.pdpdt.2020.102000. Epub 2020 Sep 9 [PubMed PMID: 32919077]
Level 1 (high-level) evidenceHalabi D, Escobar J, Alvarado C, Martinez N, Muñoz C. Chlorhexidine for prevention of alveolar osteitis: a randomised clinical trial. Journal of applied oral science : revista FOB. 2018:26():e20170245. doi: 10.1590/1678-7757-2017-0245. Epub 2018 May 7 [PubMed PMID: 29742264]
Level 1 (high-level) evidenceZhou J, Hu B, Liu Y, Yang Z, Song J. The efficacy of intra-alveolar 0.2% chlorhexidine gel on alveolar osteitis: a meta-analysis. Oral diseases. 2017 Jul:23(5):598-608. doi: 10.1111/odi.12553. Epub 2016 Aug 29 [PubMed PMID: 27479137]
Level 1 (high-level) evidenceRodríguez Sánchez F, Rodríguez Andrés C, Arteagoitia Calvo I. Does Chlorhexidine Prevent Alveolar Osteitis After Third Molar Extractions? Systematic Review and Meta-Analysis. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2017 May:75(5):901-914. doi: 10.1016/j.joms.2017.01.002. Epub 2017 Jan 13 [PubMed PMID: 28189661]
Level 1 (high-level) evidenceYengopal V, Mickenautsch S. Chlorhexidine for the prevention of alveolar osteitis. International journal of oral and maxillofacial surgery. 2012 Oct:41(10):1253-64. doi: 10.1016/j.ijom.2012.04.017. Epub 2012 May 22 [PubMed PMID: 22622144]
Level 1 (high-level) evidenceAdekunle AA, Egbunah UP, Erinoso OA, Adeyemo WL. Effectiveness of warm saline mouth bath in preventing alveolar osteitis: A systematic review and meta-analysis. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2021 Oct:49(10):980-988. doi: 10.1016/j.jcms.2021.09.001. Epub 2021 Sep 4 [PubMed PMID: 34509363]
Level 1 (high-level) evidence