Introduction
Sinusitis is inflammation of the sinus or nasal passage. Chronic sinusitis is chronic inflammation of the sinus or nasal passages occurring for more than 12 weeks at a time. Recurrent sinusitis is defined as greater than four episodes of sinusitis within a one-year period. The evaluation and management of acute and chronic sinusitis are similar. Chronic sinusitis may present as (1) chronic sinusitis without nasal polyps, (2) chronic sinusitis with nasal polyps, and (3) allergic fungal rhinosinusitis. [1][2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
As stated in the acute sinusitis chapter, viruses and bacteria are the most common etiologies for sinusitis. Streptococcus, pneumococcus, Hemophilus, and Moraxella are the most common bacterial causes. Chronic sinusitis is multifactorial in nature and can include infectious, inflammatory, or structural factors. Thus, other etiologies such as allergic rhinitis (dust mites, molds), exposures (airborne irritants, cigarette smoke or other toxins), structural causes (nasal polyps, deviated nasal septum), ciliary dysfunction, immunodeficiencies, and fungal infections should be considered. Otitis media, asthma, AIDS, and cystic fibrosis, are other medical conditions that can be associated with chronic rhinosinusitis.[3][4]
Epidemiology
When the inflammatory process involves the paranasal sinus, it is sinusitis. It can often involve accompanying nasal airway inflammation, and when it involves both, this is then called rhinosinusitis. Chronic rhinosinusitis is one of the most common chronic conditions. It is prevalent among all age groups and is the fifth most common reason for an antibiotic prescription.[5][6][7]
Pathophysiology
There are four paired sinus cavities: the ethmoid, sphenoid, frontal, and maxillary sinus cavities. These paired cavities allow air to be filtered during inhalation. For the antigens to be filtered and expelled, sinuses need to drain. Chronic inflammation can cause obstruction to the nasal passage, hinder drainage, and lead to lower oxygen tension. This creates foci for bacteria to build up. Ciliary dysfunction or structural abnormalities can further exacerbate this process. [8]
Histopathology
Biopsy samples will usually reveal thickened basement membrane, goblet cell hyperplasia, atypical gland architecture and infiltration with monocytes. Sometimes one may also see neutrophils and eosinophils in chronic cases.
History and Physical
The three cardinal symptoms of sinusitis are:
1) Purulent drainage: green or yellow nasal discharge2) Facial/dental pain: aching, fullness or pressure-like pain 3) Nasal obstruction: this can cause difficulty breathing from one or both nasal passages or cause mouth breathing
Other symptoms of chronic sinusitis include hyposmia (decreased sense of smell), headache, ear pain, halitosis (bad breath), dental pain, cough, or fatigue. Fever only has a 50% sensitivity but is an important factor in determining the severity of sinusitis. The duration of symptoms is the key factor in diagnosing chronic sinusitis. Symptoms should occur for more than 12 weeks. Recurrent sinusitis occurs with four episodes of sinusitis within one year.
Evaluation
Chronic sinusitis is diagnosed when at least two of the following four symptoms are present and occur for more than 12 weeks: (1) purulent drainage, (2) facial and/or dental pain, (3) nasal obstruction, (4) hyposmia. The Infectious Disease Society of America (IDSA) defines sinusitis as two of the following major clinical symptoms: purulent nasal discharge, nasal congestion or obstruction, facial congestion or fullness, facial pain or pressure, hyposmia, anosmia. Alternatively, ISDA defines sinusitis as one of the aforementioned major symptoms plus two or more minor criteria such as a headache, ear pain, pressure, or fullness, halitosis or bad breath, dental pain, cough, or fatigue.
During the history and physical examination evaluation, practitioners should examine the patient for other causes such as nasal polyps. Chronic sinusitis is less common than acute sinusitis. Acute sinusitis can last up to four weeks. However, chronic sinusitis lasts twelve weeks or longer. Practitioners can seek other non-infectious etiologies such as gastric gastroesophageal reflux, anatomical variations or structural problems of the nasal cavity, history of immunodeficiencies, history of ciliary dysfunction, and history consistent fungal infections.
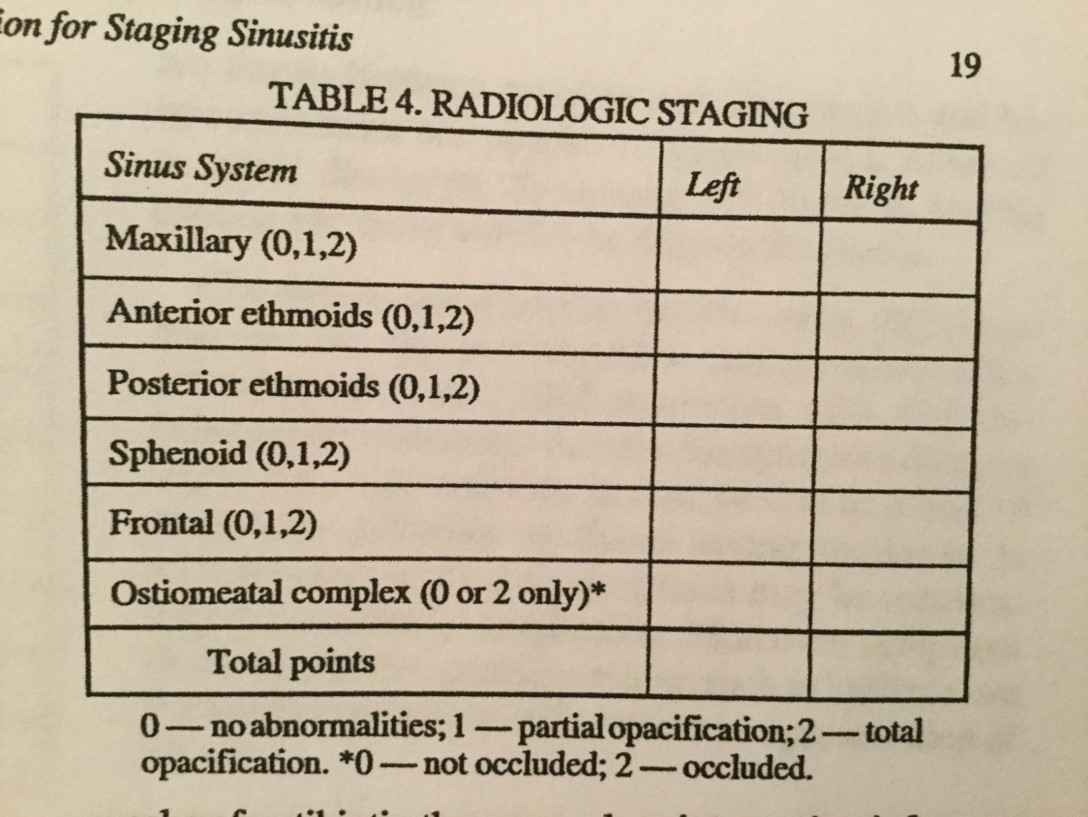
Either CT or nasal endoscopy, confirming the presence of inflammation must be documented to confirm the diagnosis of chronic sinusitis. CT is more sensitive but also more expensive than nasal endoscopy. Anterior rhinoscopy has limited visualization and has lower sensitivity and should not be used to confirm chronic sinusitis. There is a large role for shared decision-making when discussing which option to choose. Cone-beam CT scanning has become a point-of-care alternative imaging study.
Routine lab work is not necessary to diagnose chronic rhinosinusitis. Cultures are not necessary but can be helpful in treatment. If a practitioner does a nasal endoscopy, the sinus cultures should be done and are much more accurate than nasopharyngeal swabs. This can assist in providing targeted antibiotic therapy.
Allergy testing, in general, is helpful and should be considered as an option.[9][10][11]
Treatment / Management
There is no consensus on an approach to the management of chronic sinusitis. The treatment should focus on modulating triggers, reducing inflammation, and eradicating the infection.[12][5](B2)
Trigger Reduction
- Allergy testing can help identify environmental triggers that patients should avoid.
Medical Management
- Nasal steroids should be used with or without nasal saline irrigation. The treatment should last at least eight to 12 weeks with proper usage.
- Nasal saline irrigation is inferior to nasal steroids. However, nasal saline irrigation can serve as a useful adjunct. High volume nasal saline irrigation was found to be more effective than low-volume nasal spray techniques.
- Antihistamines should only be used if an allergic component is suspected.
- Decongestants can be used for symptomatic relief, but evidence for supporting their use in chronic sinusitis is lacking.
- Antibiotics can be given for an extended period of three weeks. However, there is no consensus on their routine use in chronic sinusitis, nor is their consensus on antibiotic selection.
- Anti-fungal empiric therapy should not be given.
- Oral steroids can be used. However, their use is not routinely indicated. Comments regarding their use are given below. Should oral steroids be used, physicians should engage in shared decision-making with patients.
Nasal Polyps
- Chronic sinusitis with polyps should be treated with topical nasal steroids. If severe or unresponsive to therapy after 12 weeks, a short course of oral steroids can be considered.
- Leukotriene antagonists can be considered.
Surgical Management
- Functional endoscopic sinus surgery can be considered for patients who fail medical management. In more complicated cases, it can serve as an adjunct to medical management. The goal of this surgery is to relieve obstructions, restore drainage and mucociliary clearance, and to ventilate the sinuses.
If an underlying medical condition is found, then therapy should target the underlying condition. This could include surgical and medical approaches to fungal sinusitis or Intravenous immunoglobulin for immunodeficiencies. Management for both of these conditions is beyond the scope of this chapter.
Other associated and predisposing medical conditions should also be treated. These include asthma, otitis media, and cystic fibrosis.
Differential Diagnosis
- Asthma
- Sinus tumors
- Oral cavity infections
- Nasal and sinus papillomas
Complications
- Laryngitis
- Dacryocystitis
- Orbital cellulitis/abscess
- Cavernous sinus thrombosis
- Meningitis, subdural abscess, brain abscess
- Frontal bone osteomyelitis
Enhancing Healthcare Team Outcomes
The management of chronic sinusitis is best done with an interprofessional team of healthcare workers that includes primary care, infectious disease experts, otolaryngologists, and radiologists, and specialty trained nurses. Otolaryngology nurses should educate the patient on controlling the trigger factors like avoiding tobacco, which can exacerbate the symptoms of chronic sinusitis. The pharmacist should educate the patient on antiallergy therapies that can help control the symptoms. The patients should also be told to manage gastroesophageal reflux disease because it is a known trigger for chronic sinusitis. Finally, the patients should be educated on the possible complications of chronic sinusitis and when to seek medical assistance.[13][14][15] [Level V]
Outcomes
Chronic sinusitis may be a benign disorder, but it has significant morbidity. If not treated, the quality of life is poor. The condition is known to exacerbate asthma and can even lead to meningitis and brain abscess formation- which increases morbidity and mortality. Patients with chronic sinusitis who are treated usually have satisfactory outcomes. Symptom relief can be obtained after functional endoscopic sinus surgery in about 75% of patients who fail to respond to medical management. In rare cases, chronic sinusitis can result in orbital and intracranial infections, leading to visual and neurological deficits. [16][17][Level V]
Media
(Click Image to Enlarge)
References
Klimek L, Koennecke M, Hagemann J, Wollenberg B, Becker S. [Immunology of chronic rhinosinusitis with nasal polyps as a basis for treatment with biologicals]. HNO. 2019 Jan:67(1):15-26. doi: 10.1007/s00106-018-0557-7. Epub [PubMed PMID: 30167718]
Pipolo C, Saibene AM, Felisati G. Prevalence of pain due to rhinosinusitis: a review. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2018 Jun:39(Suppl 1):21-24. doi: 10.1007/s10072-018-3336-z. Epub [PubMed PMID: 29904833]
Stryjewska-Makuch G, Janik MA, Lisowska G, Kolebacz B. Bacteriological analysis of isolated chronic sinusitis without polyps. Postepy dermatologii i alergologii. 2018 Aug:35(4):375-380. doi: 10.5114/ada.2018.77667. Epub 2018 Aug 21 [PubMed PMID: 30206450]
Cho HJ, Kim CH. Oxygen matters: hypoxia as a pathogenic mechanism in rhinosinusitis. BMB reports. 2018 Feb:51(2):59-64 [PubMed PMID: 29366441]
Park JJH, Seidel DU, Bachert C, Dazert S, Kostev K. Medication use in patients with chronic rhinosinusitis in Germany - a large retrospective patient-based study. Rhinology. 2019 Apr 1:57(2):94-100. doi: 10.4193/Rhin18.055. Epub [PubMed PMID: 30076702]
Level 2 (mid-level) evidencePhilpott CM, Erskine S, Hopkins C, Kumar N, Anari S, Kara N, Sunkaraneni S, Ray J, Clark A, Wilson A, CRES group, Erskine S, Philpott C, Clark A, Hopkins C, Robertson A, Ahmed S, Kara N, Carrie S, Sunkaraneni V, Ray J, Anari S, Jervis P, Panesaar J, Farboud A, Kumar N, Cathcart R, Almeyda R, Khalil H, Prinsley P, Mansell N, Salam M, Hobson J, Woods J, Coombes E. Prevalence of asthma, aspirin sensitivity and allergy in chronic rhinosinusitis: data from the UK National Chronic Rhinosinusitis Epidemiology Study. Respiratory research. 2018 Jun 27:19(1):129. doi: 10.1186/s12931-018-0823-y. Epub 2018 Jun 27 [PubMed PMID: 29945606]
Barac A, Ong DSY, Jovancevic L, Peric A, Surda P, Tomic Spiric V, Rubino S. Fungi-Induced Upper and Lower Respiratory Tract Allergic Diseases: One Entity. Frontiers in microbiology. 2018:9():583. doi: 10.3389/fmicb.2018.00583. Epub 2018 Apr 3 [PubMed PMID: 29666610]
Heath J, Hartzell L, Putt C, Kennedy JL. Chronic Rhinosinusitis in Children: Pathophysiology, Evaluation, and Medical Management. Current allergy and asthma reports. 2018 May 29:18(7):37. doi: 10.1007/s11882-018-0792-8. Epub 2018 May 29 [PubMed PMID: 29845321]
Sohn HG, Park SJ, Ryu IS, Lim HW, Song YJ, Yeo NK. Comparison of Clinical Presentation and Surgical Outcomes Between Recurrent Acute Rhinosinusitis and Chronic Rhinosinusitis. The Annals of otology, rhinology, and laryngology. 2018 Nov:127(11):763-769. doi: 10.1177/0003489418792942. Epub 2018 Aug 10 [PubMed PMID: 30095001]
Kalaiarasi R, Vijayakumar C, Archana R, Venkataramanan R, Chidambaram R, Shrinuvasan S, Prabhu R. Role of Thermography in the Diagnosis of Chronic Sinusitis. Cureus. 2018 Mar 10:10(3):e2298. doi: 10.7759/cureus.2298. Epub 2018 Mar 10 [PubMed PMID: 29755895]
She W, Yang J, Wang C, Zhang L. Diagnostic Value of Nasal Cytology in Chronic Rhinosinusitis Assessed by a Liquid-based Cytological Technique. American journal of rhinology & allergy. 2018 May:32(3):181-187. doi: 10.1177/1945892418768581. Epub 2018 Apr 17 [PubMed PMID: 29660995]
Kim DK, Kang SI, Kong IG, Cho YH, Song SK, Hyun SJ, Cho SD, Han SY, Cho SH, Kim DW. Two-Track Medical Treatment Strategy According to the Clinical Scoring System for Chronic Rhinosinusitis. Allergy, asthma & immunology research. 2018 Sep:10(5):490-502. doi: 10.4168/aair.2018.10.5.490. Epub [PubMed PMID: 30088369]
Expert Panel on Neurologic Imaging:, Kirsch CFE, Bykowski J, Aulino JM, Berger KL, Choudhri AF, Conley DB, Luttrull MD, Nunez D Jr, Shah LM, Sharma A, Shetty VS, Subramaniam RM, Symko SC, Cornelius RS. ACR Appropriateness Criteria(®) Sinonasal Disease. Journal of the American College of Radiology : JACR. 2017 Nov:14(11S):S550-S559. doi: 10.1016/j.jacr.2017.08.041. Epub [PubMed PMID: 29101992]
Levy JM, Rudmik L, Peters AT, Wise SK, Rotenberg BW, Smith TL. Contemporary management of chronic rhinosinusitis with nasal polyposis in aspirin-exacerbated respiratory disease: an evidence-based review with recommendations. International forum of allergy & rhinology. 2016 Dec:6(12):1273-1283. doi: 10.1002/alr.21826. Epub 2016 Aug 2 [PubMed PMID: 27480830]
Sedaghat AR. Chronic Rhinosinusitis. American family physician. 2017 Oct 15:96(8):500-506 [PubMed PMID: 29094889]
Chowdhury NI, Mace JC, Bodner TE, Alt JA, Deconde AS, Levy JM, Smith TL. Does Medical Therapy Improve SinoNasal Outcomes Test-22 Domain Scores? An Analysis of Clinically Important Differences. The Laryngoscope. 2019 Jan:129(1):31-36. doi: 10.1002/lary.27470. Epub 2018 Sep 12 [PubMed PMID: 30208209]
Alt JA, Orlandi RR, Mace JC, Soler ZM, Smith TL. Does Delaying Endoscopic Sinus Surgery Adversely Impact Quality-of-Life Outcomes? The Laryngoscope. 2019 Feb:129(2):303-311. doi: 10.1002/lary.27473. Epub 2018 Sep 12 [PubMed PMID: 30208208]
Level 2 (mid-level) evidence