Introduction
Fine needle aspiration (FNA) was initially performed in the 1930s when Martin and Ellis first described the procedure and the potential implications in the medical field.[1] Initially, interest in the procedure remained low due in part to concerns with regards to cancer seeding. Walfish later described the use of combined ultrasound guidance and needle aspiration cytology in increasing the diagnostic accuracy of specimen acquisition.[2] The role of ultrasound-guided FNA has evolved over time as an important tool in the assessment of thyroid nodules.
The important aspects of the FNA procedure include:
- Minimizing patient discomfort
- Maintaining patient safety
- Maintaining proper ultrasound and needle technique in order to visualize needle entry to the target nodule
- Ensuring adequate acquisition of tissue sample
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
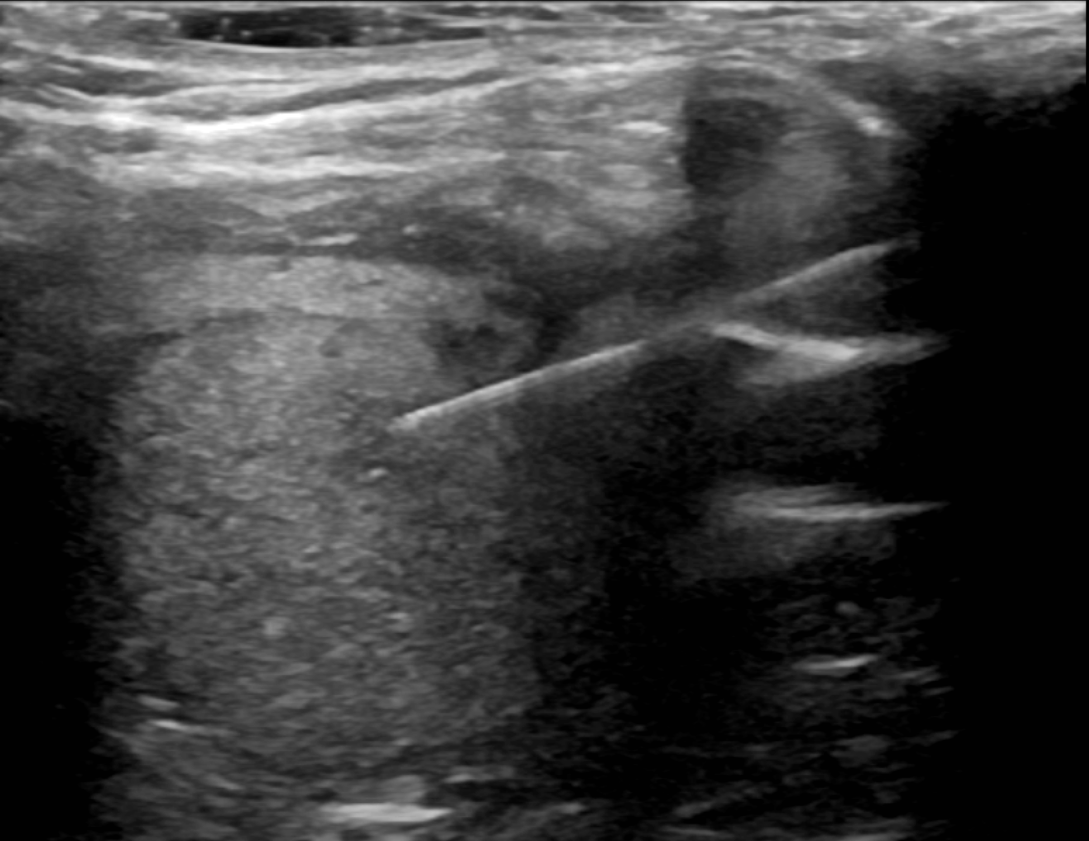
The thyroid gland is a midline structure located in the anterior neck, specifically anterior to the trachea.[3] The thyroid gland is divided into two lobes, which are connected in the midline by the isthmus. The isthmus crosses the midline of the upper trachea at the second and third tracheal rings. On ultrasound, the thyroid gland is easily identified due to its general hyperechogenicity with respect to the adjacent sternocleidomastoid muscle at the lateral margin and the sternohyoid muscle at the anterior margin. Nodularity within the thyroid gland can be considered a normal part of aging, with the incidence of nodules increasing with age.[4] Thyroid nodules can be identified due to their difference in echogenicity when compared to normal surrounding thyroid parenchyma. Various studies have investigated the role of ultrasound features in understanding the malignant potential of nodules.[5][6][7][8] Sonographic features that may relate to and/or raise concern for thyroid malignancy include hypoechogenicity, microcalcifications, lobulated appearance, taller-than-wide shape, irregular margins, and increased internal vascularity.[9][10]
Indications
Ultrasound-guided FNA is often performed based on suspicious sonographic features on an initial thyroid ultrasound or imaging characteristic changes on follow-up examinations. The American Thyroid Association (ATA) and the British Thyroid Association (BTA) have published guidelines providing risk stratification based on ultrasound features. The American College of Radiology (ACR) has also provided Thyroid Imaging, Reporting, and Data System (TI-RADS) classification with regards to FNA or imaging follow-up recommendations based on sonographic features.[11] One recent study demonstrated the ATA and TI-RADS systems demonstrate similar sensitivity and specificity in adequately characterizing malignant nodules.[12] Regardless of classification criteria used by a provider, the primary indication for a thyroid nodule FNA is to further investigate sonographic features suspicious for malignancy.
Contraindications
Contraindications to thyroid nodule FNA include:
- Bleeding diathesis
- An uncooperative patient
- Infection at the skin site of needle entry
- Results of FNA not altering management
Evaluating the patient for a past medical history of bleeding diathesis is especially important. Local post-procedural hematomas in patients with bleeding disorders can exert a mass effect on the trachea and cause significant respiratory distress.
Different studies have suggested that FNA procedures can be performed safely in patients taking antithrombotic and anticoagulant agents without the need for discontinuation.[13]. The Society of Interventional Radiology Guidelines classifies thyroid biopsies within the low bleeding risk category without the routine use of screening coagulation blood tests.[14] These guidelines also do not recommend withholding anticoagulants in low-risk bleeding procedures.
Equipment
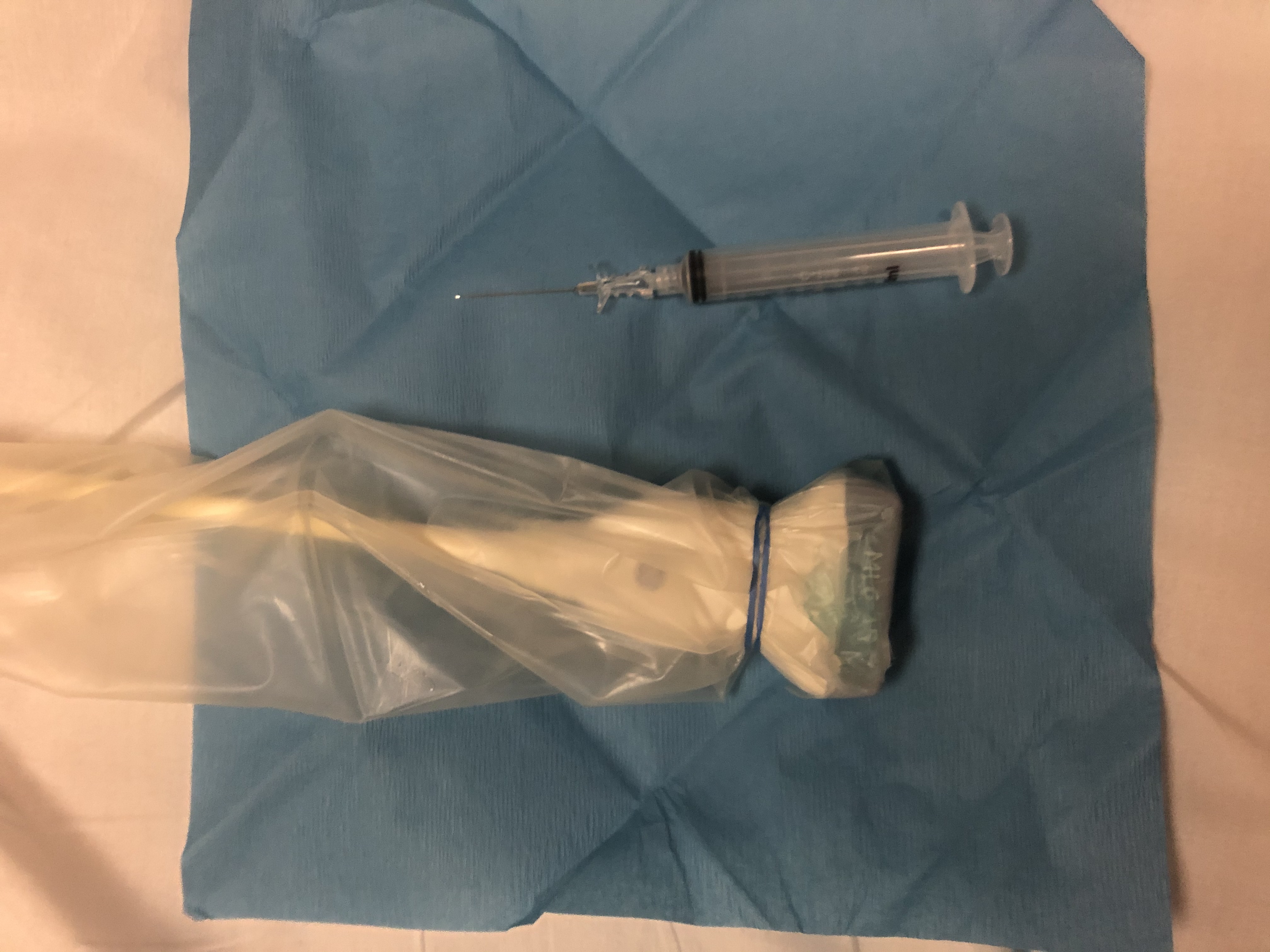
- Fenestrated drape or towel drapes
- High-resolution (7.5 MHz to 15 MHz) linear-array transducer and ultrasound machine
- Sterile cover for the head of the transducer probe
- Sterile ultrasound gel or iodine-based solution as a coupling medium
- 1 mL to 3 mL of 1% lidocaine hydrochloride for local anesthesia
- 22 gauge to 27 gauge needle with an attached syringe used for specimen acquisition
Personnel
- Operator or physician performing the procedure
- Ultrasound technologist assisting the operator
- Pathology technician involved in preparing the acquired specimen for pathologist review
- Pathologist to determine the adequacy of specimen acquisition
Preparation
A thorough discussion with a patient prior to the procedure includes the following:
- A detailed explanation of the procedure
- The expected level of discomfort
- Option for local anesthesia
- History of bleeding disorders or anticoagulant use
- Prior medical conditions that might affect the procedure
- Potential diagnoses resulting from the procedure
- Potential complications of the procedure
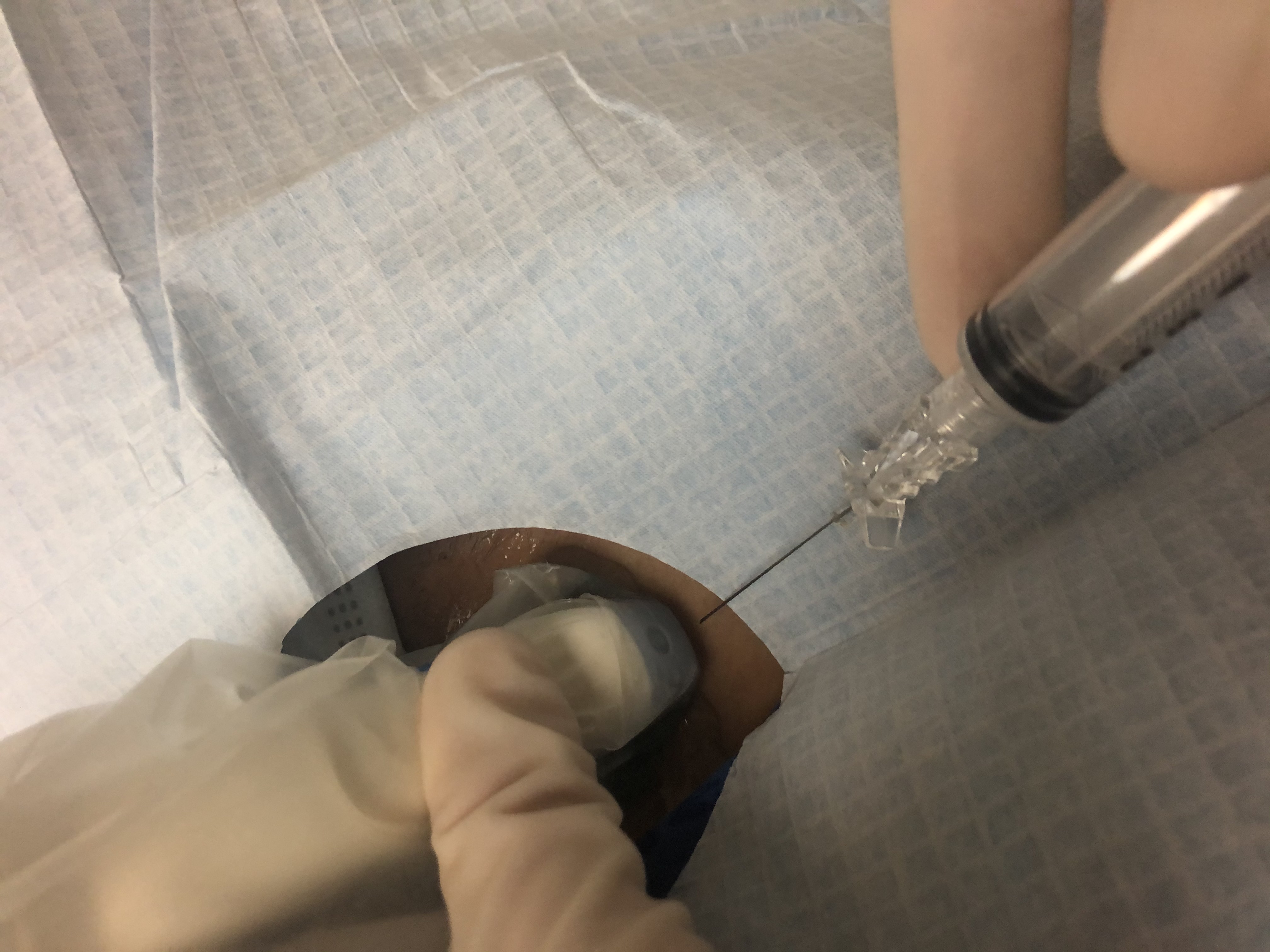
The patient is placed in a supine position for the procedure. Prior to beginning the procedure, a brief preliminary ultrasound of the thyroid is performed to asses the nodule's location. The operator can take this time to better position the patient, probe, and monitor. This also allows the operator to visualize the proposed needle trajectory and surrounding vasculature via doppler mapping. The skin is then marked at the proposed site of entry.
Whether sterile technique and local anesthesia are employed for the procedure often remains dependent on provider and institution preference. The incidence of local infection from FNA is exceptionally rare.[15] Studies have also suggested that anesthesia use can be limited to a small subset of patients.[16][17] Due to the varying levels of operator proficiency, it is recommended to employ the sterile technique and local anesthesia.
The skin site is cleaned, and a sterile field is established with a fenestrated drape or with towel drapes. A high-resolution (7.5 MHz to 15 MHz) linear-array transducer is used for optimal visualization of the target nodule. A sterile cover is placed over the head of the probe. Sterile ultrasound gel can be avoided if the skin site is sterilized with an iodine-based solution, which can serve as an adequate ultrasound coupling medium. Local anesthesia is administered with approximately 1 mL to 3 mL of 1% lidocaine hydrochloride, either subcutaneously or through the proposed soft tissue trajectory of the FNA needle. This ultimately depends on nodule depth and location. A 22 gauge to 27 gauge needle with an attached syringe is used for specimen acquisition.
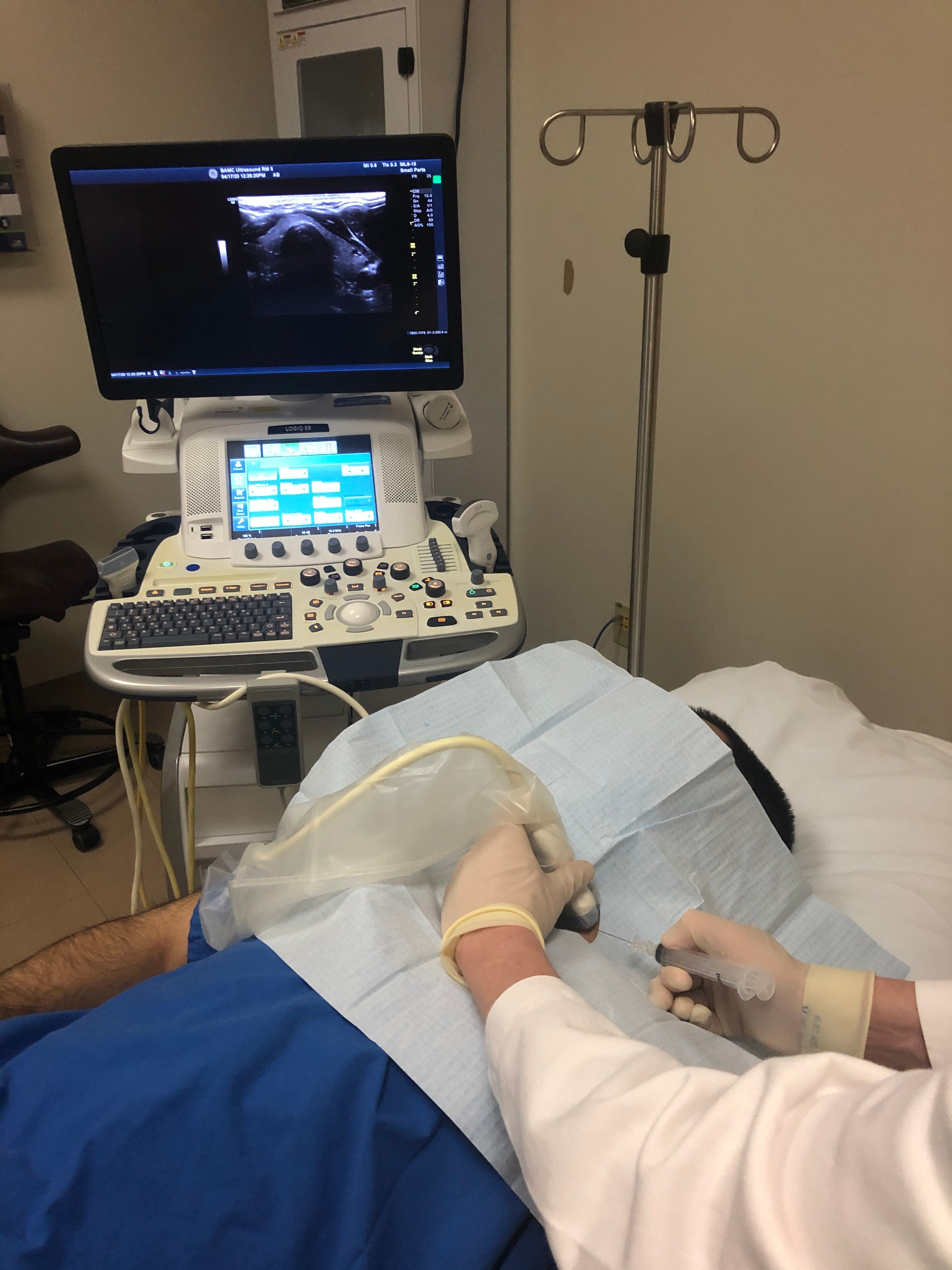
The ultrasound monitor should be located across the patient from the operator. A general linear alignment of the needle, the long axis of the transducer, and the monitor is important for optimal hand-eye coordination. This allows the operator to easily assess needle positioning within the soft tissues on the monitor while comfortably manipulating the needle.
Technique or Treatment
The basic steps involved in an ultrasound-guided thyroid nodule FNA include the following:
- The transducer is placed over the target nodule in the transverse (axial) plane.
- The patient is directed to remain stationary and refrain from speaking.
- The needle is placed just above the transducer and advanced through the marked skin site, either parallel or perpendicular to the transducer.
- The needle is advanced to the nodule and moved to and fro multiple times through the nodule.
Nonaspiration technique involves performing this maneuver without suction, with capillary action allowing the collection of the specimen within the needle hub. Aspiration technique allows for specimen acquisition via operator application of gentle suction during the to and fro maneuver. Although nonaspiration technique has occasionally been shown to be superior to the aspiration technique, two meta-analysis studies revealed no significant difference between the two.[18][19][20] The needle-syringes may be delivered to a cytopathologist present during the procedure for further processing to ensure adequate acquisition. Multiple aspiration attempts are performed until a satisfactory tissue sample is confirmed by the cytopathologist.
Complications
The vast majority of thyroid FNAs are performed with ease and without complication. Development of a neck hematoma remains a concerning, yet rare, complication of thyroid FNA procedures. Other complications are also rare and include pain, transient swelling, infection, and vasovagal reaction.[21]
Clinical Significance
The primary goal of performing an FNA of a thyroid nodule is to diagnose and/or exclude a malignant thyroid nodule. Ultrasound-guided FNA is imperative in directing the management of thyroid nodules, allowing for prompt diagnosis and treatment of thyroid malignancies. Additionally, the identification of benign thyroid nodules helps avoid unnecessary surgery and helps guide treatment and reduce the cost of care.[22]
Papillary thyroid cancer rates have been gradually increasing in incidence.[23] Papillary and follicular cancers are considered differentiated malignancies and are treated with total or partial thyroidectomy.[24] In particular, identifying papillary thyroid cancer is especially important due to its relatively good prognosis, with mortality rate, which have been reported as low as 2%.[25] Treatment includes surgical resection or administration of radioactive iodine. Anaplastic thyroid carcinoma, however, is extremely aggressive and occurs during the 6th and 7th decades. Clinically, anaplastic thyroid carcinoma commonly results in aggressive tumor expansion and growth, leading to compressive symptoms from mass effect on adjacent structures such as the cervical airway. The 5-year survival rate is around 5%.[26]
The importance of prompt identification and diagnosis of thyroid cancer has also been demonstrated in the Surveillance, Epidemiology, and End Results database, where the mortality rate of localized thyroid cancer has been shown to be significantly better when compared to regional and metastatic disease.[23][27] Ultrasound-guided FNA is an inexpensive and safe modality in the evaluation of thyroid nodules and will continue to guide clinical management for years to come.
Enhancing Healthcare Team Outcomes
The role of an ultrasound technologist is exceptionally important in helping the operator during the procedure. Patient comfort is critical in properly performing the procedure as significant patient movement can affect specimen acquisition and potentially injure adjacent anatomy such as blood vessels or the trachea. The assistant's role is essential in ensuring patient comfort, safety, and maintaining the sterile field. Quickly obtaining specimens is also important, considering blood infiltration within the thyroid parenchyma limits the quality of successive needle passes. If possible, an assistant ultrasound technologist can deliver the specimens to the cytopathologist while the operator continues acquiring additional specimens. Thus potentially improving the quality and adequacy of all aspirated specimens acquired during the procedure.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Martin HE, Ellis EB. BIOPSY BY NEEDLE PUNCTURE AND ASPIRATION. Annals of surgery. 1930 Aug:92(2):169-81 [PubMed PMID: 17866350]
Walfish PG, Hazani E, Strawbridge HT, Miskin M, Rosen IB. Combined ultrasound and needle aspiration cytology in the assessment and management of hypofunctioning thyroid nodule. Annals of internal medicine. 1977 Sep:87(3):270-4 [PubMed PMID: 900669]
Allen E, Fingeret A. Anatomy, Head and Neck, Thyroid. StatPearls. 2023 Jan:(): [PubMed PMID: 29262169]
Chaudhary V, Bano S. Thyroid ultrasound. Indian journal of endocrinology and metabolism. 2013 Mar:17(2):219-27. doi: 10.4103/2230-8210.109667. Epub [PubMed PMID: 23776892]
Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, Cronan JJ, Doubilet PM, Evans DB, Goellner JR, Hay ID, Hertzberg BS, Intenzo CM, Jeffrey RB, Langer JE, Larsen PR, Mandel SJ, Middleton WD, Reading CC, Sherman SI, Tessler FN. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Ultrasound quarterly. 2006 Dec:22(4):231-8; discussion 239-40 [PubMed PMID: 17146329]
Level 3 (low-level) evidenceMandel SJ. Diagnostic use of ultrasonography in patients with nodular thyroid disease. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2004 May-Jun:10(3):246-52 [PubMed PMID: 15310543]
Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, Panunzi C, Rinaldi R, Toscano V, Pacella CM. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. The Journal of clinical endocrinology and metabolism. 2002 May:87(5):1941-6 [PubMed PMID: 11994321]
Rago T, Vitti P, Chiovato L, Mazzeo S, De Liperi A, Miccoli P, Viacava P, Bogazzi F, Martino E, Pinchera A. Role of conventional ultrasonography and color flow-doppler sonography in predicting malignancy in 'cold' thyroid nodules. European journal of endocrinology. 1998 Jan:138(1):41-6 [PubMed PMID: 9461314]
Hong YJ, Son EJ, Kim EK, Kwak JY, Hong SW, Chang HS. Positive predictive values of sonographic features of solid thyroid nodule. Clinical imaging. 2010 Mar-Apr:34(2):127-33. doi: 10.1016/j.clinimag.2008.10.034. Epub [PubMed PMID: 20189077]
Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, Kim J, Kim HS, Byun JS, Lee DH, Thyroid Study Group, Korean Society of Neuro- and Head and Neck Radiology. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008 Jun:247(3):762-70. doi: 10.1148/radiol.2473070944. Epub 2008 Apr 10 [PubMed PMID: 18403624]
Level 2 (mid-level) evidenceTessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, Cronan JJ, Beland MD, Desser TS, Frates MC, Hammers LW, Hamper UM, Langer JE, Reading CC, Scoutt LM, Stavros AT. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. Journal of the American College of Radiology : JACR. 2017 May:14(5):587-595. doi: 10.1016/j.jacr.2017.01.046. Epub 2017 Apr 2 [PubMed PMID: 28372962]
Chng CL, Tan HC, Too CW, Lim WY, Chiam PPS, Zhu L, Nadkarni NV, Lim AYY. Diagnostic performance of ATA, BTA and TIRADS sonographic patterns in the prediction of malignancy in histologically proven thyroid nodules. Singapore medical journal. 2018 Nov:59(11):578-583. doi: 10.11622/smedj.2018062. Epub 2018 May 18 [PubMed PMID: 29774361]
Khadra H, Kholmatov R, Monlezun D, Kandil E. Do anticoagulation medications increase the risk of haematoma in ultrasound-guided fine needle aspiration of thyroid lesions? Cytopathology : official journal of the British Society for Clinical Cytology. 2018 Dec:29(6):565-568. doi: 10.1111/cyt.12608. Epub 2018 Aug 3 [PubMed PMID: 29969159]
Patel IJ, Rahim S, Davidson JC, Hanks SE, Tam AL, Walker TG, Wilkins LR, Sarode R, Weinberg I. Society of Interventional Radiology Consensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in Patients Undergoing Percutaneous Image-Guided Interventions-Part II: Recommendations: Endorsed by the Canadian Association for Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. Journal of vascular and interventional radiology : JVIR. 2019 Aug:30(8):1168-1184.e1. doi: 10.1016/j.jvir.2019.04.017. Epub 2019 Jun 20 [PubMed PMID: 31229333]
Level 3 (low-level) evidenceFeldkamp J, Führer D, Luster M, Musholt TJ, Spitzweg C, Schott M. Fine Needle Aspiration in the Investigation of Thyroid Nodules. Deutsches Arzteblatt international. 2016 May 20:113(20):353-9. doi: 10.3238/arztebl.2016.0353. Epub [PubMed PMID: 27294815]
Lo WC, Cheng PW, Wang CT, Yeh ST, Liao LJ. Pain levels associated with ultrasound-guided fine-needle aspiration biopsy for neck masses. Head & neck. 2014 Feb:36(2):252-6. doi: 10.1002/hed.23303. Epub 2013 Jun 1 [PubMed PMID: 23728803]
Leboulleux S, Borget I, Labro S, Bidault S, Vielh P, Hartl D, Dauchy S, Chougnet CN, Girard E, Azoulay S, Mirghani H, Berdelou A, Lumbroso J, Deandreis D, Baudin E, Schlumberger M, Laurent S. Frequency and intensity of pain related to thyroid nodule fine-needle aspiration cytology. Thyroid : official journal of the American Thyroid Association. 2013 Sep:23(9):1113-8. doi: 10.1089/thy.2012.0461. Epub 2013 Aug 27 [PubMed PMID: 23384309]
Song H, Wei C, Li D, Hua K, Song J, Maskey N, Fang L. Comparison of Fine Needle Aspiration and Fine Needle Nonaspiration Cytology of Thyroid Nodules: A Meta-Analysis. BioMed research international. 2015:2015():796120. doi: 10.1155/2015/796120. Epub 2015 Sep 29 [PubMed PMID: 26491689]
Level 1 (high-level) evidenceMaurya AK, Mehta A, Mani NS, Nijhawan VS, Batra R. Comparison of aspiration vs non-aspiration techniques in fine-needle cytology of thyroid lesions. Journal of cytology. 2010 Apr:27(2):51-4. doi: 10.4103/0970-9371.70737. Epub [PubMed PMID: 21157549]
Guo YM, Huo JL, Qu R, Hu XC, Liu DS, Chen ZY, Hong W. [A comparison of fine needle nonaspiration cytology versus fine needle aspiration for thyroid nodules: a Meta-analysis]. Lin chuang er bi yan hou tou jing wai ke za zhi = Journal of clinical otorhinolaryngology, head, and neck surgery. 2018 Jun 5:32(11):868-872. doi: 10.13201/j.issn.1001-1781.2018.11.017. Epub [PubMed PMID: 29921061]
Level 1 (high-level) evidencePolyzos SA, Anastasilakis AD. Clinical complications following thyroid fine-needle biopsy: a systematic review. Clinical endocrinology. 2009 Aug:71(2):157-65. doi: 10.1111/j.1365-2265.2009.03522.x. Epub 2009 Jan 19 [PubMed PMID: 19170717]
Level 1 (high-level) evidenceGharib H. Fine-needle aspiration biopsy of thyroid nodules: advantages, limitations, and effect. Mayo Clinic proceedings. 1994 Jan:69(1):44-9 [PubMed PMID: 8271850]
Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013. JAMA. 2017 Apr 4:317(13):1338-1348. doi: 10.1001/jama.2017.2719. Epub [PubMed PMID: 28362912]
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid : official journal of the American Thyroid Association. 2016 Jan:26(1):1-133. doi: 10.1089/thy.2015.0020. Epub [PubMed PMID: 26462967]
Ito Y, Miyauchi A, Kihara M, Fukushima M, Higashiyama T, Miya A. Overall Survival of Papillary Thyroid Carcinoma Patients: A Single-Institution Long-Term Follow-Up of 5897 Patients. World journal of surgery. 2018 Mar:42(3):615-622. doi: 10.1007/s00268-018-4479-z. Epub [PubMed PMID: 29349484]
Chiacchio S, Lorenzoni A, Boni G, Rubello D, Elisei R, Mariani G. Anaplastic thyroid cancer: prevalence, diagnosis and treatment. Minerva endocrinologica. 2008 Dec:33(4):341-57 [PubMed PMID: 18923370]
Lin B, Ma H, Ma M, Zhang Z, Sun Z, Hsieh IY, Okenwa O, Guan H, Li J, Lv W. The incidence and survival analysis for anaplastic thyroid cancer: a SEER database analysis. American journal of translational research. 2019:11(9):5888-5896 [PubMed PMID: 31632557]