Introduction
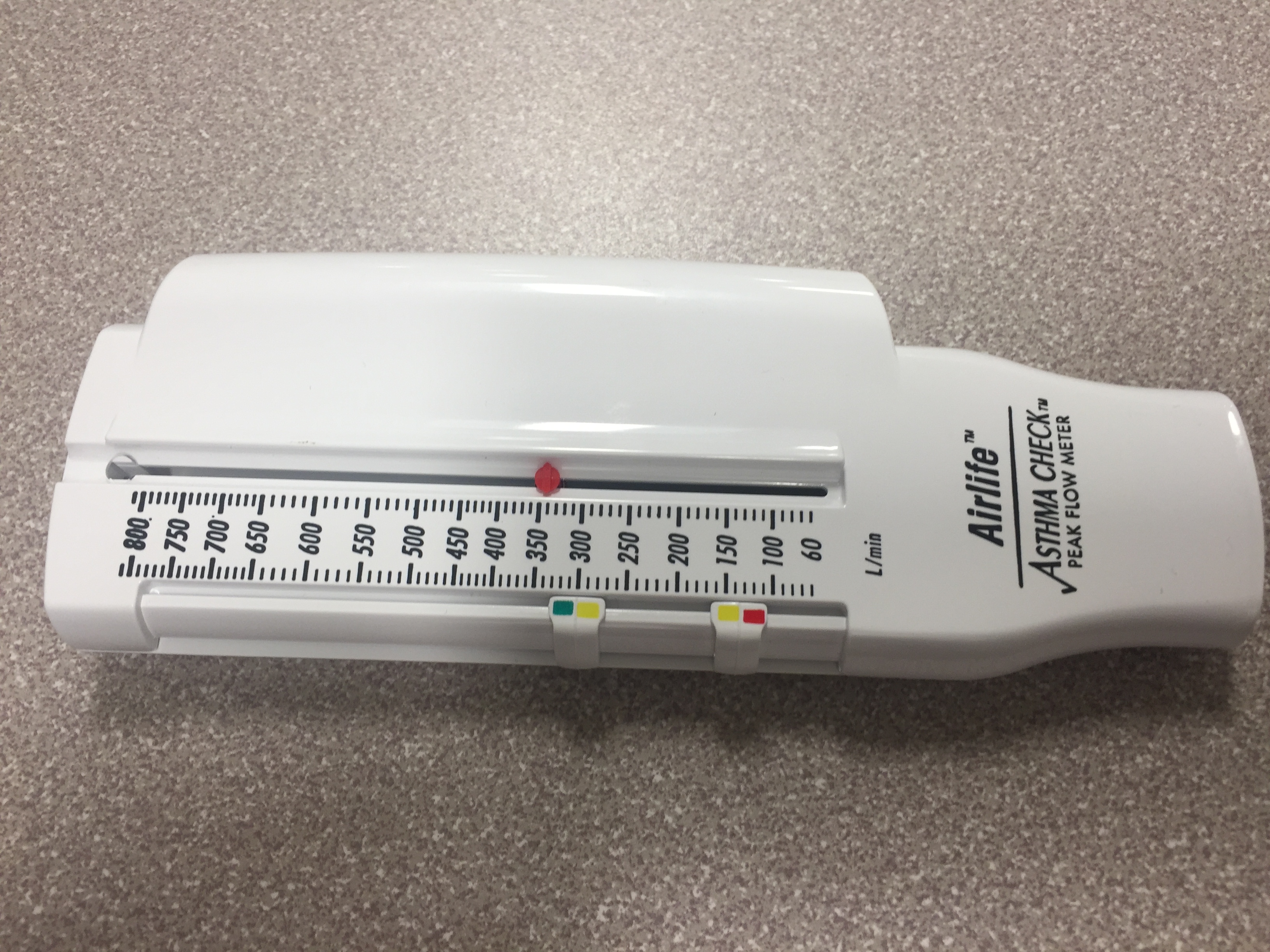
Peak expiratory flow (PEF), a key indicator of lung function, offers clinicians valuable insights into asthma management. Typically measured with a peak flow meter, PEF provides an objective measure of airflow limitation, aiding in assessing asthma control and managing exacerbations (see Image. Peak Flow Meter).[1] A maximal effort is required when using a peak flow meter to obtain valid results.[2] The depth of the preceding breath, airway caliber, muscle strength, and voluntary effort all contribute to PEF. Clinicians should observe patients using a peak flow meter to identify suboptimal effort or technique. However, variability exists between devices, and no good technique exists to calibrate readings between different flow meters.[3] The International Organization for Standardization has published guidelines for PEF meters; clinicians and patients should choose devices that meet these criteria.
Once a patient establishes a personal best, clinicians can create an individualized asthma action plan, including instructions the patient can follow at home. Routine monitoring of a PEF aids in determining the effectiveness of therapy, provides an early warning of potential exacerbations, and can be especially helpful for patients with difficulties recognizing asthma symptoms. PEF measurement can also assess the severity and response to treatment during an acute asthma exacerbation in adolescents and adults. PEF is assessed less commonly during acute exacerbations in younger children. With personalized action plans based on individual PEF values, clinicians can provide early intervention and optimized maintenance therapy, improving management and outcomes for patients with asthma.[4]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
The primary indication for a PEF measurement is self-assessment and self-management of asthma symptoms based on a written action plan. Patients follow written instructions based on their symptoms and peak flow measurements. Studies reveal that a written action plan reduces asthma morbidity in adults and children.[5][6][7] Monitoring the PEF may be especially helpful for patients who have difficulty recognizing asthma symptoms or exacerbating factors.[8] Additional indications for using a peak flow meter include assessing severity and the response to treatment during acute asthma exacerbations in adults and adolescents, home monitoring of asthma, and assessing occupational asthma. Due to effort and technique requirements, clinicians rarely use peak flow measurements to measure the severity of an acute exacerbation in children younger than 12. Patients suspected of having occupational asthma may benefit from serial peak flow measurements at and outside the workplace.[9][10]
Equipment
Various peak flow meters are available for purchase. The standard peak flow meter is a simple cylindrical handheld device with a mouthpiece and an indicator with measurements along the body that patients can reuse many times. Some electronic meters can record and transmit the readings to the provider. Handheld electronic spirometers that measure FVC, FEV1, and PEF are also available for home use.
Technique or Treatment
Despite the various designs of peak flow meters, they all operate using the same basic technique. Clinicians should instruct the patient to perform the following process:
- Move the indicator to 0.
- Stand or sit up straight.
- Take in a breath as deep as possible.
- Place the meter in the mouth and close the lips around the mouthpiece, ensuring the tongue is not blocking or inside the opening.
- As soon as the lips are closed, blow out as hard and fast as possible, using the chest and abdominal muscles. This should take no more than 2 seconds.
- Write down the result.
- Repeat the steps above 2 more times.
- Report the highest result to your provider.
The clinician should observe the patient's technique during in-office education and assist with necessary adjustments. Clinicians should also review the technique at subsequent follow-up visits. Peak flow rates in individual patients tend to decrease over time, likely from waning skill and effort.[11] This observation highlights the need for ongoing retraining of techniques after the initial clinic visit. Some authors recommend retraining at every follow-up visit in conjunction with inhaler retraining.[12] Clinicians should reestablish patients' personal best annually to assess for growth in children and disease progression.
Clinical Significance
Ideally, patients establish a personal best peak flow rate when feeling well.[13] Patients should record their peak flow values in a diary 2 to 4 times daily for 2 weeks. The personal best is the highest peak flow measured during this time. A personal best peak flow value can be higher or lower than the predicted value. Clinicians then use the patient's personal best to create an action plan for self-monitoring and managing acute exacerbations. Studies have indicated that an action plan improves asthma control and quality of life.[6]
Clinicians should be cautioned against over-reliance on peak flow measurements alone. Studies evaluating the overall outcomes when utilizing peak flow measurement alone show conflicting results and reveal no advantage of using PEF monitoring over symptom monitoring to guide self-management.[14] Society guidelines have suggested a comprehensive approach that accounts for both subjective symptoms and objective data from the peak flow meter. Data show that this approach can decrease healthcare utilization.
Typical peak flow meters come equipped with gauge markers indicating 3 "zones" that can be set by the patient or clinician to help users interpret their peak flow values. For ease of patient interpretation, the colors of a traditional traffic light designate varying degrees of peak flow limitation. The designated zones correlate with a written asthma action plan.
Green zone: This zone designates peak flow values of 80% to 100% of the patient's personal best. In the absence of symptoms, the patient continues with their current regimen.
Yellow zone: The yellow zone encompasses peak flow values between 50% and 80% of the patient's personal best. Patients employ their home action plan, beginning with bronchodilators, when they identify readings in this zone.[15]
Red zone: Patients in the red zone have peak flow measurements below 50% of their personal best. They should begin bronchodilator therapy immediately and contact their clinician if their peak flow measurements do not immediately return to the yellow or green zones. Peak flow measurements in this range indicate that severe airway obstruction may be present and is a medical emergency. See StatPearls' companion references "Asthma" and "Pediatric Asthma" for a detailed description of the management of acute asthma exacerbations in adults and children.
PEF measurement is also helpful in guiding disposition in the emergency setting. A patient with a peak flow rate of less than 50% without improvement despite aggressive therapy warrants hospital admission for ongoing care and close monitoring for signs of impending respiratory failure. Respiratory therapists and nurses can obtain and report serial peak flow measurements throughout the hospital course to guide disposition decisions. In the inpatient setting, patients often do not know their personal best. In this situation, published tables of normal PEF rates for height and weight are available. Generally, a peak flow rate below 200 L/min indicates severe obstruction for most adults younger than 65.
Special Populations
Pediatrics
Children aged 5 or older can use the peak flow meter with reliable results. However, cooperation with the technique may limit the accuracy during acute exacerbations, and clinicians should interpret the results cautiously. For this reason, healthcare professionals do not routinely use peak flow measurements during acute asthma exacerbations in children. Tables of normal peak flow rates are available for children and adolescents. Additionally, when children use a peak flow monitor for self-management and assessment, clinicians should consider providing a second meter for the child to keep at school in the nurse's office should concerns arise.
Pregnancy
Despite body changes associated with pregnancy, peak flow rate and personal best numbers do not change through each trimester or during the postpartum period. Changes in the observed PEF in pregnant women should be treated as worsening obstruction until proven otherwise.[6]
Limitations
As mentioned previously, suboptimal effort can lead to falsely decreased readings. Chest wall disease, obesity, and muscle weakness can also reduce PEF without airflow limitation. In patients with severe asthma, peak flow measurement can underestimate the degree of airflow limitation.[14] Patients often have difficulty adhering to long-term peak flow monitoring.[15] Routine measurement is most effective when limited to shorter periods.
Enhancing Healthcare Team Outcomes
Peak flow measurement reflects the maximal exhalation rate following full inspiration, making it a valuable tool for asthma management. Peak flow values objectively measure airflow limitation when spirometry is unavailable. Clinicians and other team members must possess the skills to accurately measure and interpret peak flow values, including proficiency in instructing patients on proper technique and integrating results into clinical decision-making. Patient education on proper technique is essential, as validity hinges on maximal effort, and factors such as the depth of the preceding breath, airway caliber, and muscle strength influence results. After a patient's personal best is established, peak flow guides in creating an asthma action plan, symptom self-management, and assisting in treating acute exacerbations. Color-coded zones modeled after a traditional traffic light simplify interpretation and give patients a clear understanding of necessary management based on their symptoms and peak flow measurements. Interpretation in pediatric patients requires care due to potential limitations in technique.
Developing standardized protocols and guidelines ensures consistency and promotes best practices across disciplines. Effective interprofessional communication ensures seamless care coordination, involving sharing information, clarifying roles, and addressing concerns. Care coordination efforts prioritize patient education, empowerment, and engagement in self-management, ensuring thorough asthma management and optimal use of peak flow measurement. Prioritizing patient-centered care promotes collaboration, trust, and treatment plan adherence, ultimately reducing morbidity and improving healthcare team performance.
Media
References
Rathod MB, Budensab A, Bhalla S, Mahesh NK, Alex E, Jesudas M. Spirometric Assessment of Pulmonary Function Tests in Asthma Patients. Cureus. 2024 Feb:16(2):e54979. doi: 10.7759/cureus.54979. Epub 2024 Feb 26 [PubMed PMID: 38550448]
Kyejo W, Matillya N, Ismail N, Gachocha G, Salum H, Iseme R, Noorani M. The anthropometric determinants of peak expiratory flow rate among children in Dar Es Salaam, Tanzania. BMC pediatrics. 2024 Jan 13:24(1):42. doi: 10.1186/s12887-023-04520-1. Epub 2024 Jan 13 [PubMed PMID: 38218839]
Tsukioka K. [Comparison of different types of peak flow meter and reference values for peak expiratory flow (PEF) for healthy Japanese subjects]. Nihon rinsho. Japanese journal of clinical medicine. 1996 Nov:54(11):2927-32 [PubMed PMID: 8950932]
Soumagne T, Chenivesse C, Didier A, Giovannini-Chami L, Magnan A, Taillé C, et les investigateurs du groupe d’étude PAE. [Written action plans for asthma control: How are they used by pulmonologists in France?]. Revue des maladies respiratoires. 2024 Feb:41(2):102-109. doi: 10.1016/j.rmr.2024.01.001. Epub 2024 Jan 15 [PubMed PMID: 38228440]
Chen X, Han P, Kong Y, Shen K. The relationship between changes in peak expiratory flow and asthma exacerbations in asthmatic children. BMC pediatrics. 2024 Apr 27:24(1):284. doi: 10.1186/s12887-024-04754-7. Epub 2024 Apr 27 [PubMed PMID: 38678177]
Muhammad J, Ngah ND, Ahmad I. Written Asthma Action Plan Improves Asthma Control and the Quality of Life among Pediatric Asthma Patients in Malaysia: A Randomized Control Trial. Korean journal of family medicine. 2023 Jan:44(1):44-52. doi: 10.4082/kjfm.22.0016. Epub 2023 Jan 19 [PubMed PMID: 36709960]
Level 1 (high-level) evidenceGatheral TL, Rushton A, Evans DJ, Mulvaney CA, Halcovitch NR, Whiteley G, Eccles FJ, Spencer S. Personalised asthma action plans for adults with asthma. The Cochrane database of systematic reviews. 2017 Apr 10:4(4):CD011859. doi: 10.1002/14651858.CD011859.pub2. Epub 2017 Apr 10 [PubMed PMID: 28394084]
Level 1 (high-level) evidenceBarnes PJ, Szefler SJ, Reddel HK, Chipps BE. Symptoms and perception of airway obstruction in asthmatic patients: Clinical implications for use of reliever medications. The Journal of allergy and clinical immunology. 2019 Nov:144(5):1180-1186. doi: 10.1016/j.jaci.2019.06.040. Epub 2019 Jul 19 [PubMed PMID: 31330221]
Moscato G, Godnic-Cvar J, Maestrelli P. Statement on self-monitoring of peak expiratory flows in the investigation of occupational asthma. Subcommittee on Occupational Allergy of European Academy of Allergy and Clinical Immunology. The Journal of allergy and clinical immunology. 1995 Sep:96(3):295-301 [PubMed PMID: 7560631]
Park D, Moore VC, Burge CB, Jaakkola MS, Robertson AS, Burge PS. Serial PEF measurement is superior to cross-shift change in diagnosing occupational asthma. The European respiratory journal. 2009 Sep:34(3):574-8. doi: 10.1183/09031936.00150108. Epub 2009 Mar 26 [PubMed PMID: 19324953]
van Schoor NM, de Jongh RT, Lips P, Deeg DJH, Kok AAL. Long-term trajectories of peak expiratory flow rate in older men and women show linear decline mainly determined by baseline levels. Aging clinical and experimental research. 2024 Apr 16:36(1):93. doi: 10.1007/s40520-024-02735-5. Epub 2024 Apr 16 [PubMed PMID: 38627297]
Gannon PF, Belcher J, Pantin CF, Burge PS. The effect of patient technique and training on the accuracy of self-recorded peak expiratory flow. The European respiratory journal. 1999 Jul:14(1):28-31 [PubMed PMID: 10489825]
Reddel HK, Marks GB, Jenkins CR. When can personal best peak flow be determined for asthma action plans? Thorax. 2004 Nov:59(11):922-4 [PubMed PMID: 15516464]
Tierney WM, Roesner JF, Seshadri R, Lykens MG, Murray MD, Weinberger M. Assessing symptoms and peak expiratory flow rate as predictors of asthma exacerbations. Journal of general internal medicine. 2004 Mar:19(3):237-42 [PubMed PMID: 15009778]
Polk BI, Dinakar C. Management of acute loss of asthma control: yellow zone strategies. Current opinion in allergy and clinical immunology. 2019 Apr:19(2):154-160. doi: 10.1097/ACI.0000000000000512. Epub [PubMed PMID: 30649012]
Level 3 (low-level) evidence