Introduction
Blepharoplasty refers to the aesthetic or functional surgical manipulation of the upper or lower eyelids. Upper and lower lid blepharoplasty both have their own set of indications and may be undertaken during the same procedure or at different times. Understanding the anatomy of the upper and lower eyelids is key to the identification of deformities that may be amenable to surgical correction while also preventing unwanted complications from these same surgical procedures.[1][2][3][4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Eyelid Lamellae
The upper and lower eyelids consist of an anterior and posterior lamella. The orbital septum separates these lamellae superiorly. The anterior lamella is made up of the skin, subcutaneous tissue, and orbicularis oculi muscle. The posterior lamella consists of the tarsal plate and conjunctiva.[5]
Tarsal Plates
The tarsal plates are part of the posterior lamellae of the eyelid. The tarsal plates are responsible for providing structural integrity to the lid margin. The upper lid tarsal plate is around 10 mm in height, whereas the lower lid tarsal plate is around 4 mm in height.
Canthal Tendons
The medial and lateral canthal tendons anchor the tarsal plates to the orbit, suspending the tarsal plates. The lateral canthal tendon consists of a superior and inferior crus. The posterior reflection of these attachments connects to Whitnall’s tubercle, which is located 2 mm deep to the lateral orbital rim. The medial canthal tendon has a superior and inferior crus, as well as anterior and posterior reflections that attach to the anterior and posterior lacrimal crests.
Postseptal Fat Compartments
The upper eyelid contains only 2 fat pads, the preaponeurotic and the nasal fat pad. The interpad septum separates these compartments. The nasal fat pad contains fat that has a distinctly white color when compared to the other fat compartments of the eyelid. The lower eyelid contains three postseptal fat compartments. These are the nasal, central, and lateral fat pads. The inferior oblique muscle separates the nasal and central fat pads. The central and lateral fat compartments are separated by a component of the Lockwood ligament.
Tear Trough
This anatomic area also referred to as the nasojugal groove, is created by the attachment of the orbital retaining ligament, or orbital malar ligament, to the skin. This ligament originates from the inferior orbital rim and runs from the medial canthus to the medial corneoscleral limbus.
Levator Apparatus
The upper lid levator apparatus consists of the levator palpebrae superioris muscle and the underlying Müller’s muscle, which originates from the levator muscle. The latter is sympathetically innervated, while the levator muscle itself is innervated by the superior division of the oculomotor nerve (cranial nerve III). The confluence of both of these muscles inserts as the levator aponeurosis on the superior aspect of the tarsal plate. Fibers from the levator palpebrae superioris insert onto the skin of the upper lid approximately 8 to 10 mm above the superior edge of the tarsus.
Lacrimal Apparatus
The lacrimal apparatus consists of the secretions of the lacrimal gland which are subsequently collected by the lacrimal canaliculi and lacrimal sac. These secretions, which form the aqueous layer of tears, then empty down the nasolacrimal duct to a meatus just inferior to the inferior concha. The lacrimal gland may contribute to an excessive fullness of the upper lateral aspect of the eye. While suspending it may improve aesthetic outcomes, any manipulation of this apparatus can alter tear secretions and contribute to dry eyes.
Indications
Dermatochalasis refers to the excess of the skin of the lower or upper eyelids. Many patients will seek blepharoplasty for cosmetic concerns related to the amount of dermatochalasis of either the upper or lower lids. However, a large amount of excess skin can contribute to physiologic pathology. Specifically, significant dermatochalasis of the upper lids may contribute to lateral hooding and visual obstruction, while that of the lower lid may contribute to ectropion. Steatoblepharon refers to the fat protrusion in the upper and lower eyelids, which may also cause a cosmetic concern to patients. Significant steatoblepharon or dermatochalasis is an indication for upper or lower lid blepharoplasty. Cosmetically, the goal for the upper lid is resection of skin and fat to allow a mild hollow and shadow related to the superior orbital rim and eliminate lateral hooding. Care must be taken not to remove an excessive amount of skin or fat, as either may cause a severely hollowed appearance of the upper lid or postoperative lagophthalmos. The goal remains the same for the lower eyelid, though lower lid procedures also focus on alleviating the sagging of the lower lid and treating the lid-cheek junction.[6][7][8][9]
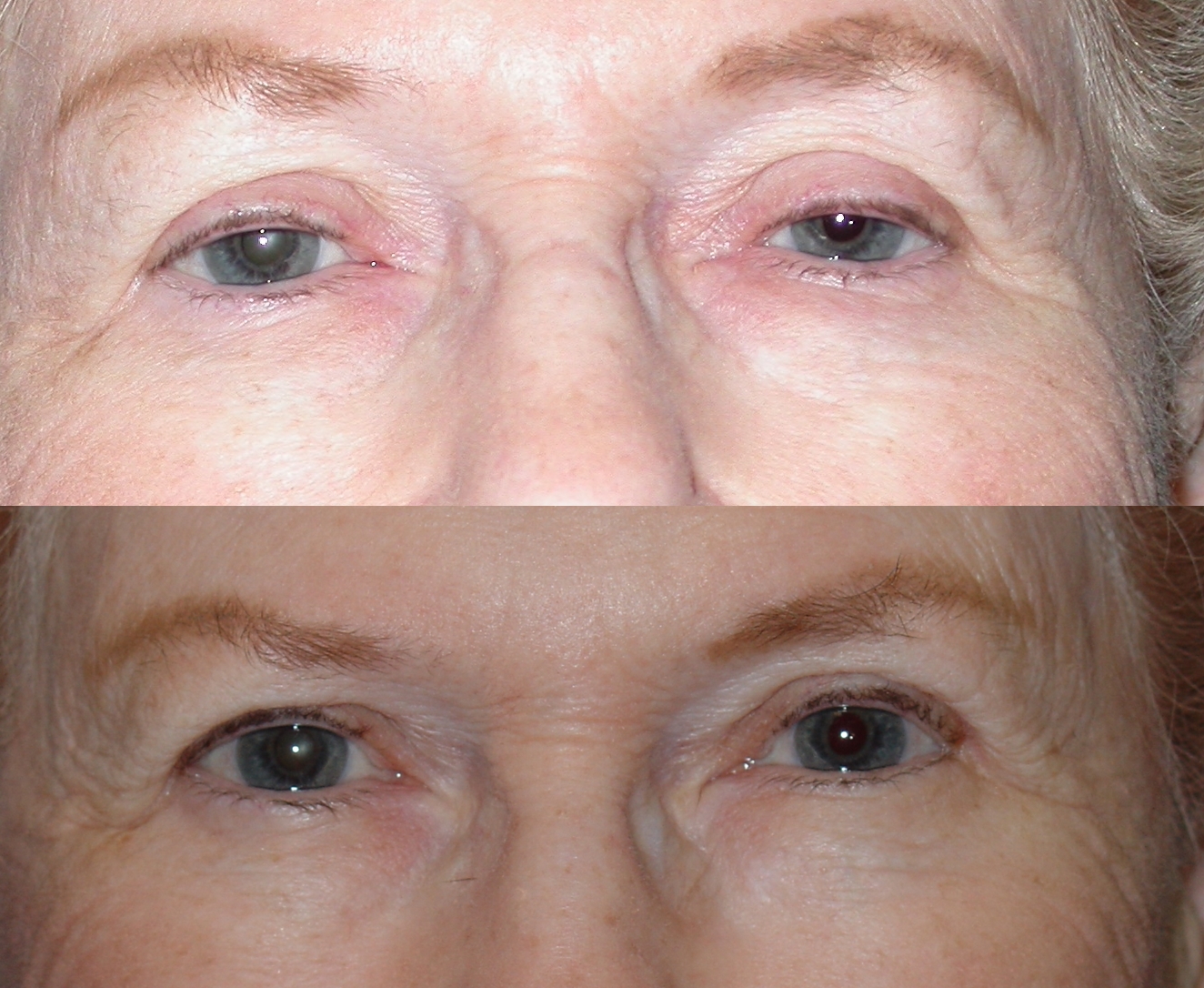
A pathologic concern specific to the upper eyelid is ptosis. While a full review of ptosis is outside of the scope of this chapter, it is worth mentioning that many patients presenting for blepharoplasty will suffer from senile ptosis or the disinsertion of the levator apparatus from the tarsus. Patients affected by this pathology will show the variable overlap of the upper lid over the pupil. Although there are various ways described to assess the degree of ptosis, the most reliable way is to measure the distance from the mid pupil to the lid margin. Classically, this distance has been described by the margin reflex distance 1 (MRD1). This refers to the distance between the light reflected off of the center of the pupil in primary position and the margin of the upper eyelid. To properly assess ptosis utilizing the MRD1, light must be reflected off of the center point of the pupil. The normal MRD1 is 4 mm. It is important to note that ptosis is specific to each eyelid, and the position of the lid on the oculus dexter (OD, right eye) and oculus sinister (OS, left eye) may differ. Patients with significant ptosis, often described as an MRD1 of 1 to 2 mm, are often considered candidates for levator advancement procedures.
A common indication applicable to the lower eyelid is lower lid ectropion or turning out of the lid exposing the conjunctiva. Though the causes of ectropion are vast and again outside of the scope of this text, the presence of ectropion may indicate a decrease in the elasticity and increase in the laxity of the lower lid. This feature can be assessed using the lower lid snap-back test, in which the lower lid is pulled away from the sclera and allowed to retract. The lower lid may be slow to retract or will not retract at all, indicating that a lateral canthopexy or canthoplasty may be necessary.
Contraindications
All patients undergoing eyelid procedures should be questioned regarding ophthalmologic pathology and should receive a full eye exam, complete with the retinal examination. Specifically, patients should be questioned regarding preoperative visual acuity, symptoms of dry eyes, and visual obstruction. Furthermore, the full medical history should include pathology related to systemic disease with ophthalmologic manifestations, including thyroid disease, diabetes, hypertension, or inflammatory diseases treated with steroids. A history of bleeding or clotting disorders should also be elicited. The following tests are useful in the workup of patients undergoing blepharoplasty to identify contraindications based on specific complaints.
Shirmer’s Test
Measures basal tear secretion and identifies patients that are at risk for dry eyes postoperatively. Absorptive paper strips are placed inside the lower lid for 5 minutes, and the amount of moisture on the paper is measured. Greater than or equal to 15 mm is considered normal, while less than 5 mm is indicative of deficient tear production.
Visual Field Testing
Identifies any areas of visual fields that may be obstructed by ptosis or dermatochalasis. The test is typically performed once with the lids in the normal position, and then with tape securing excess skin above the level of the lid margin. Goldman perimetry and Humphrey visual fields can be used to assess for visual deficits.[10][11]
Jones Test
The Jones I and Jones II tests are used to evaluate the patency of lacrimal ducts. During the Jones I test, fluorescein dye is injected into the lacrimal sac and given 5 minutes to flow from the lacrimal sac into the opening at the inferior meatus. If the dye is present after 5 minutes, the test is positive, and the ducts are open. If no dye flows through, the Jones II test is performed in which a lacrimal syringe is used to irrigate the lacrimal ducts, and flow to the intranasal opening is again evaluated. If a positive test is identified in which the dye flows through, this confirms a functional problem with the lacrimal drainage system. If no dye flows through with lacrimal irrigation, a mechanical obstruction is identified.
Equipment
A standard ophthalmologic or plastic surgical instrument set should be adequate to perform the procedure. Local anesthetic with epinephrine will be a valuable tool for this procedure. Not only will it allow the procedure to be done under sedation, but the epinephrine will cause vasoconstriction and will aid in hemostasis.
Personnel
Blepharoplasty may be performed in an office-based setting. Though the eyelids are amenable to complete anesthesia with local anesthetic, it is often helpful to give sedation during injection as this is extremely uncomfortable. As with any procedure, the use of intravenous (IV) sedation should be performed in the presence of an anesthesia provider familiar with airway management. Furthermore, if IV sedation is used, an inpatient facility or an operating room certified by the American Association for Accreditation of Ambulatory Surgery Facilities is strongly advised. Furthermore, to ensure the safety of the patient and the best possible outcomes, blepharoplasty should be performed by those with extensive training in the procedure including board-certified plastic surgeons, oculoplastic surgeons, or facial plastic surgeons.
Technique or Treatment
Upper lid blepharoplasty involves the excision of a wedge of the skin of the upper lid. The lower edge of the skin wedge excision approximates the point of the supratarsal crease, stretching from 4 to 5 mm superior to the medial and lateral canthi with its highest point in the center of the line extending 10 mm above the central aspect of the lid margin. The upper part of the wedge excision is marked as a gentle curve following the natural upward slant of the eyelid and orbit and is determined intra-operatively by pinching the skin of the upper lid. The surgeon must take care to leave approximately 1.5 to 2 cm of skin between the upper part of the excision and the brow, as this will prevent lid hollowing and lagophthalmos from excess skin resection. The excision markings may be extended approximately 1 cm lateral to the lateral canthus to excise lateral hooding.
There are several variations of upper lid blepharoplasty. The first involves variable excision of orbicularis muscle along with the overlying skin. Advocates of significant orbicularis resection will point to the fact that it contributes to upper lid fullness and should be resected. Over resection, however, can hollow the upper lid and destroy the attachments of the levator complex to the overlying skin. These complications could cause postoperative lagophthalmos or ptosis, respectively. Postseptal fat may also be removed during this procedure. The nasal fat pad is most often the offending agent in upper lid blepharoplasty and may be accessed through a 1 cm incision in the orbital septum medially. The surgeon will know he or she is in the correct compartment due to the white hue of the fat compared to the yellow color of other fat compartments. Again, avoiding overcorrection is key.
Upper lid blepharoplasty is often combined with the correction of upper lid ptosis. The most common form of this procedure involves removing the levator aponeurosis from the tarsus, advancing the entire aponeurotic complex, and resecuring the tarsus to the aponeurosis complex. Following the advancement and securing of the levator complex, the patient is asked to open and close his or her eyes. The degree of lagophthalmos is assessed. Up to 2 mm is considered acceptable. If the degree of lid lag is found to be appropriate, the excess muscle and tendon are resected, and the skin and orbicularis flap is closed.
Lower lid blepharoplasty is one of the most variable procedures in plastic surgery, and a full review of this technique is outside of the scope of this article. In general, the technique involves skin resection, postseptal fat resection, blunting of the lid-cheek junction, and tightening of the lower lid tarsoligamentous complex. Not all patients will require every aspect of this procedure. However, each will be addressed separately.
The amount of skin resection should be assessed pre-operatively to determine which incision will be used to access the lower lid. Those patients requiring skin resection will need an external incision on the lid, most often from a subciliary approach. Those patients not requiring skin resection may have postseptal fat resected from the transconjunctival approach. Excess skin resection of the lower lid may contribute to post-operative ectropion.
The excision of postseptal fat is common in lower lid blepharoplasty, as steatoblepharon is one of the main features of many seeking a lower lid blepharoplasty. Each compartment may be accessed separately from either the external or transconjunctival approach. When excising fat in the central or nasal fat pads, care must be taken to not injure the inferior oblique muscles. Meticulous hemostasis is crucial in all aspects of blepharoplasty but is particularly important in the fat resection. As fat resection occurs in the postseptal compartment, bleeding may contribute to retrobulbar hemorrhage, and in severe cases can cause blindness.
The treatment of the lid-cheek junction is a complex aspect of the procedure and can be accomplished in many different ways. The fundamental concept of this procedure is to cause blunting and a more gradual, youthful appearance of a facial line that has been caused by aging. To accomplish this, fat released from the postseptal compartment may be spread over the angle to cause a more gradual transition from the cheek to the lower eyelid. Conversely, the arcus marginalis may be completely released and then sutured over this angle to cause a more obtuse angle. Though there are countless other methods for addressing this problem and it is impossible to review them all here, it is important when evaluating these patients postoperatively to understand that this junction has likely been manipulated in some way.
Tightening of the lower lid tarsoligamentous complex is accomplished by traditional canthopexy or canthoplasty techniques. This typically involves a lateral canthotomy with inferior cantholysis. Part of the lateral tarsoligamentous complex may be resected utilizing a lateral tarsal strip procedure. It is imperative to inset the lower lid partially inside of the orbit and at a superior angle to the medial canthus to approximate the actual position of the lower eyelid. Some surgeons will choose to temporarily support the repair of the lateral tarsoligamentous complex with an external suture, tape, or gentle upward massage.
Both upper and lower blepharoplasty techniques may differ greatly between surgeons. However, being aware of the principles outlined above should give both specialist and general practitioners general guidelines on upper and lower lid blepharoplasty procedures.
Complications
Lagophthalmos
Defined by the failure of the upper lid margin to reach the lower lid margin, what is commonly referred to as “lid lag” can either be a complication or an expected outcome of the blepharoplasty procedure. With levator advancement procedures, up to 2 mm of lid lag can be acceptable and will resolve over time. Management of post-operative lagophthalmos includes corneal lubrication to protect against corneal abrasion. Patients should be monitored closely during this time to ensure any degree of lagophthalmos is resolving.[9]
Ectropion
Ectropion can evolve during lower lid procedures with excess skin resection, scarring, or loosening of the tarsoligamentous complex. While conservative management such as upward massage or upward taping can be undertaken, ectropion is typically corrected by surgical retightening of the lower lid. Until that time, eye lubrication can be utilized to decrease discomfort.
Dry Eyes
Many patients may complain of dry eyes postoperatively. Utilizing Schirmer’s test pre-operatively can select for the patients at the highest risk. Any manipulation of the lacrimal system, such as resuspension of the lacrimal gland, can also place patients at high risk for dry eyes. Corneal lubrication is the mainstay of treatment. Referral to an ophthalmologist may be necessary if these symptoms do not resolve.
Retrobulbar Hemorrhage
The most feared complication of blepharoplasty is a retrobulbar hematoma. Typically caused by bleeding following postseptal fat resection, this complication presents with severe ocular pain, proptosis, and visual complaints. Patients may have all symptoms or only one. In any patient presenting with these symptoms following blepharoplasty, the diagnosis of a retrobulbar hematoma should be considered. The treatment is emergent orbital decompression with lateral canthotomy with inferior cantholysis.
Clinical Significance
Blepharoplasty is a common procedure that can improve the visual fields and cosmesis of a patient. Knowing the indications can help patients be correctly evaluated for the procedure. Knowing the complications can help patients get the correct post-operative treatment.
Enhancing Healthcare Team Outcomes
Blepharoplasty is a common procedure performed by multiple surgical specialties. Primary care physicians, as well as specialists that perform surgical procedures of the face and orbit, should be aware of the anatomy, technique, and complications of blepharoplasty. The outcomes of blepharoplasty are usually good but many complications have been reported over the years. Any professional who performs blepharoplasty must know how to manage the complications. When done well, it can significantly improve patient self-esteem and confidence. [7](Level V)
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
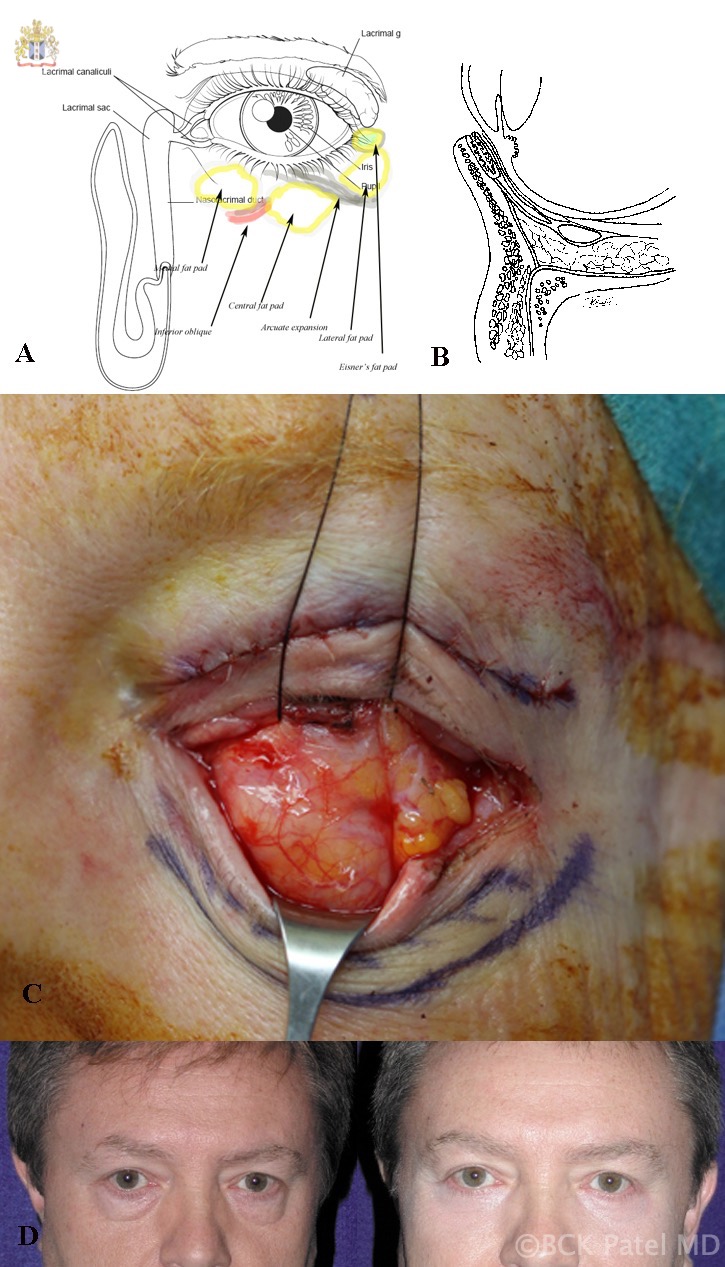
Transconjunctival Lower Blepharoplasty in a Male. Surface anatomy of the left lower eyelid fat pads (A). Cross-sectional anatomy showing the septum and post-septal fat and lower eyelid retractors (B). Traction sutures through the lower eyelid retractors (left eye) show the medial and central fat pads, often appearing as one and the lateral fat pad (C). Before-and-after photographs of transconjunctival lower blepharoplasty in a male (D).
Contributed by BCK Patel, MD, FRCS
(Click Video to Play)
References
Pan L, Sun Y, Yan S, Shi H, Jin T, Li J, Zhang L, Wu S. A Flexible Suspension Technique of Blepharoplasty: Clinical Application and Comparison with Traditional Technique. Aesthetic plastic surgery. 2019 Apr:43(2):404-411. doi: 10.1007/s00266-019-01317-5. Epub 2019 Feb 12 [PubMed PMID: 30756143]
Guo F, Ning G. [Effectiveness of upper eyelid rotation flap via blepharoplasty incision for correction of mild to moderate epicanthus]. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery. 2019 Feb 15:33(2):203-206. doi: 10.7507/1002-1892.201805097. Epub [PubMed PMID: 30739416]
Duan R, Wu M, Tremp M, Oranges CM, Xie F, Li Q. Modified Lower Blepharoplasty with Fat Repositioning via Transconjunctival Approach to Correct Tear Trough Deformity. Aesthetic plastic surgery. 2019 Jun:43(3):680-685. doi: 10.1007/s00266-019-01309-5. Epub 2019 Feb 7 [PubMed PMID: 30734070]
Johnson AR, Bravo MG, Granoff MD, Lee BT. Cultural Insensitivity Pervasive in Spanish Online Cosmetic Surgery Resources: A Call to Action. Annals of plastic surgery. 2019 Apr:82(4S Suppl 3):S228-S233. doi: 10.1097/SAP.0000000000001841. Epub [PubMed PMID: 30730317]
Patel BC, Lopez MJ, Joos ZP. Anatomy, Head and Neck: Eyelash. StatPearls. 2023 Jan:(): [PubMed PMID: 30725963]
Kokubo K, Katori N, Hayashi K, Sugawara J, Kou S, Fujii A, Kitamura S, Ninomiya R, Maegawa J. Evaluation of the eyebrow position after aponeurosis advancement. Journal of plastic surgery and hand surgery. 2019 Feb:53(1):60-64. doi: 10.1080/2000656X.2018.1547735. Epub 2019 Jan 24 [PubMed PMID: 30676851]
Papadopulos NA, Hodbod M, Henrich G, Kovacs L, Papadopoulos O, Herschbach P, Machens HG. The Effect of Blepharoplasty on Our Patient's Quality of Life, Emotional Stability, and Self-Esteem. The Journal of craniofacial surgery. 2019 Mar/Apr:30(2):377-383. doi: 10.1097/SCS.0000000000005057. Epub [PubMed PMID: 30608369]
Level 2 (mid-level) evidenceRomeo F. Upper Eyelid Filling Approach [U.E.F.A.] Technique: State of the Art After 500 Consecutive Patients. Aesthetic plastic surgery. 2019 Jun:43(3):663-672. doi: 10.1007/s00266-018-1296-6. Epub 2019 Jan 3 [PubMed PMID: 30607571]
Neves JC, Medel Jiménez R, Arancibia Tagle D, Vásquez LM. Postoperative Care of the Facial Plastic Surgery Patient-Forehead and Blepharoplasty. Facial plastic surgery : FPS. 2018 Dec:34(6):570-578. doi: 10.1055/s-0038-1676354. Epub 2018 Dec 28 [PubMed PMID: 30593072]
Hacker HD, Hollsten DA. Investigation of automated perimetry in the evaluation of patients for upper lid blepharoplasty. Ophthalmic plastic and reconstructive surgery. 1992:8(4):250-5 [PubMed PMID: 1476973]
Level 3 (low-level) evidencePemberton JD, Salter M, Fay A, Thuro B, Spencer H, Dajani O. Investigation of goldmann perimetry in evaluation of patients for upper eyelid blepharoplasty. Orbit (Amsterdam, Netherlands). 2018 Feb:37(1):48-52. doi: 10.1080/01676830.2017.1353115. Epub 2017 Aug 16 [PubMed PMID: 28812936]