Anatomy, Bony Pelvis and Lower Limb, Foot Peroneus Brevis Muscle
Anatomy, Bony Pelvis and Lower Limb, Foot Peroneus Brevis Muscle
Introduction
The peroneus brevis muscle partially forms the lateral compartment of the leg, together with its longer counterpart, the peroneus longus. The function of the peroneus brevis muscle is to evert the foot and plantarflex the ankle. The muscle receives innervation from the superficial peroneal nerve, and its arterial supply is by muscular branches of the peroneal artery. The peroneus brevis originates from the lower two-thirds of the lateral fibula and inserts on the proximal fifth metatarsal. The peroneus brevis muscle is relevant to occupational medicine due to frequent involvement in lateral ankle sprains; its tendon (along with the tendon of the peroneus longus muscle) is the most commonly dislocated tendon in the ankle [1].
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
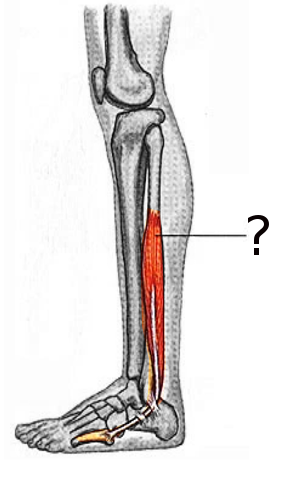
Structure and Function
The peroneus brevis muscle also referred to as the fibularis brevis muscle, is located in the lateral compartment of the lower extremity below the knee, deep to the peroneus longus muscle. It is a small, relatively short leg muscle originating from the lower two-thirds of the lateral surface of the fibula. Its muscle fibers traverse downwards and form a tendon that runs just posterior to the lateral malleolus, crossing the ankle and inserting on the styloid process of the proximal fifth metatarsal bone.[1][2]
The peroneus longus and the peroneus brevis are the only two muscles of the lateral compartment of the leg. The peroneus brevis muscle lies underneath the peroneus longus, is shorter, and has a thicker muscle belly than the peroneus longus. The tendon of the peroneus brevis begins at roughly 2 to 4 cm proximal to the tip of the lateral malleolus. It then crosses the ankle, making an anterior turn at the distal fibula, and inserts on the lateral aspect of the fifth metatarsal.[3]
The tendons of the peroneus brevis and peroneus longus muscles are contained in a common synovial sheath which originates approximately 4 cm proximal to the lateral malleolus and extends about 1cm beyond it.[4] The tendons within the synovial sheath run within the retro-malleolar groove underneath the superior peroneal retinaculum.[5][6] At the calcaneus, the tendons of the peroneus brevis and peroneus longus are separated by the peroneal tubercle of the lateral aspect of the calcaneus. The peroneus brevis courses above the tubercle, and the peroneal longus courses below the peroneal tubercle.[7]
According to cadaveric studies, the average length of the peroneus brevis tendon is 79.6 mm, and the width of the tendon was 4.46 mm and 14.85 mm at its midpoint and insertion at the fifth metatarsal, respectively.[3]
The superior and inferior peroneal retinacula function to prevent tendon subluxation as they secure the tendons of the peroneus brevis and longus in place at the level of the ankle. The superior peroneal retinaculum covers the peroneal muscle tendons with attachments at the distal fibula and lateral calcaneus. The inferior peroneal retinaculum covers the peroneal muscle tendons with insertions at the lateral calcaneus (inferior to the superior peroneal retinaculum). The inferior peroneal retinaculum is contiguous with the inferior extensor retinaculum at the dorsum of the foot.
The ankle joint is relatively mobile and relies on its surrounding ligaments for stability. The structural ligaments of the ankle connect bones to bones and are deep to the muscles and tendons of the ankle. Muscles that cross the ankle joint have a mechanical action on the foot and ankle. The primary movements of the foot and ankle are plantar flexion, dorsiflexion, eversion, and inversion. The peroneus brevis muscle and tendon cross the ankle joint posterior to the fibula. The peroneus brevis muscle assists with the eversion of the foot and, to a weaker extent, plantarflexes the ankle.[8]
Foot eversion is tilting the sole away from the midline, and foot inversion is tilting the sole towards the midline. Foot eversion requires a muscle to have an insertion on the lateral aspect of the foot, such as with the peroneus brevis, which inserts on the lateral foot at the proximal fifth metatarsal. Plantar flexion describes the movement of the foot down towards the sole, and dorsiflexion is moving the foot upwards towards the tibia. Plantar flexion requires the muscle to have an insertion relatively close to the ankle, such as with the peroneus brevis, which inserts on the proximal fifth metatarsal. The ankle joint serves as the fulcrum for both eversion and plantar flexion.[8]
Embryology
Embryologic development of the limbs begins at the end of the fourth week of fetal development. By the sixth week, the fetus develops hand plates and footplates. During limb development, the shape of the limb forms from mesenchymal cells, condensing and differentiating into chondrocytes which will ultimately differentiate into the bones and cartilage of the upper and lower extremity.
The upper and lower extremities undergo very similar embryological development patterns. Limb musculature first appears around the seventh week.[9] The mesenchyme migrates from the dorsolateral cells of somites out to the limb and differentiates into muscle cells. The lower extremity muscles below the knee develop later than the proximal muscles of the lower extremity.[10]
Blood Supply and Lymphatics
The peroneal artery arises from the tibial-peroneal trunk distal to the popliteal artery. The peroneal artery is also called the fibular artery. The peroneal artery is the blood supply to the lateral compartment of the leg. Muscular branches of the peroneal artery supply the peroneus brevis muscle.[11]
Venous drainage of the lateral compartment of the lower leg is by superficial veins that drain into the small saphenous vein and deep veins that drain into the posterior tibial vein, which then becomes the popliteal vein when joined by the anterior vein.[12]
The lymphatics of the bilateral peroneus brevis muscles and lateral compartments first drain to the popliteal and inguinal nodes and subsequently to the external iliac nodes. The external iliac nodes then drain into lumbar (aortic) nodes.[1]
Nerves
The peroneus brevis receives innervation from the muscular branch of the superficial peroneal nerve (L5-S2). The superficial peroneal nerve courses around the proximal fibula, where it is prone to injury.[1] Furthermore, the superficial peroneal nerve is vulnerable to injury at the lateral malleolus, particularly during malleolar fracture.[13]
Physiologic Variants
The peroneus quartus muscle is the most common anatomical variant of the lateral leg compartment, reported in between 5% and 20% of individuals.[14][15] Significant variations in the nomenclature and reported insertions and attachments of the muscle lead to some confusion and debate among anatomists on the topic. The variant is typically asymptomatic, but it may also be associated with crowding of the retro-malleolar groove and, therefore, an increased predisposition to ankle pain and splits or tears in the tendon of the peroneus brevis.[16] When present, the peroneus quartus muscle most commonly arises from the muscle fibers of the peroneus brevis and inserts at the retro-trochlear eminence of the calcaneus.[14] It passes through the superior peroneal retinaculum but not the inferior peroneal retinaculum before insertion.[17]
Variations in the retro-malleolar groove can predispose the peroneal tendons to tear and dislocation. Imaging and cadaveric studies demonstrate smooth, concave retro-malleolar grooves in approximately 80% of people, whereas a flat groove was seen in 11% and a convex groove in 7% of individuals.[17]
Another known variation in the anatomy of the peroneus brevis muscle is a low-lying muscle belly, defined as the peroneus brevis being beyond the expected end of the muscle belly at approximately 2 cm above the distal fibular tip.[18] This rare phenomenon is posited as a causative factor in peroneus brevis tendon rupture and subluxation.[19] Although it is difficult to ascertain a direct causal relationship, one study identified a low-lying peroneal brevis muscle belly in 80% of patients with a previous peroneus brevis tendon tear and 9 out of 10 patients who had intraoperative peroneus brevis tendon subluxation at ankle surgery.[18]
There are also many reported variations of the insertional anatomy of the peroneus brevis tendon at the fifth metatarsal. Cadaveric studies have identified six insertion types (Ia, Ib, IIa, IIb, IIIa, IIIb). Types Ia and Ib are the most common, describing a single insertion at the inferior part of the lateral aspect of the fifth metatarsal and a widened insertion encompassing the entire lateral aspect of the fifth metatarsal, respectively.[3]
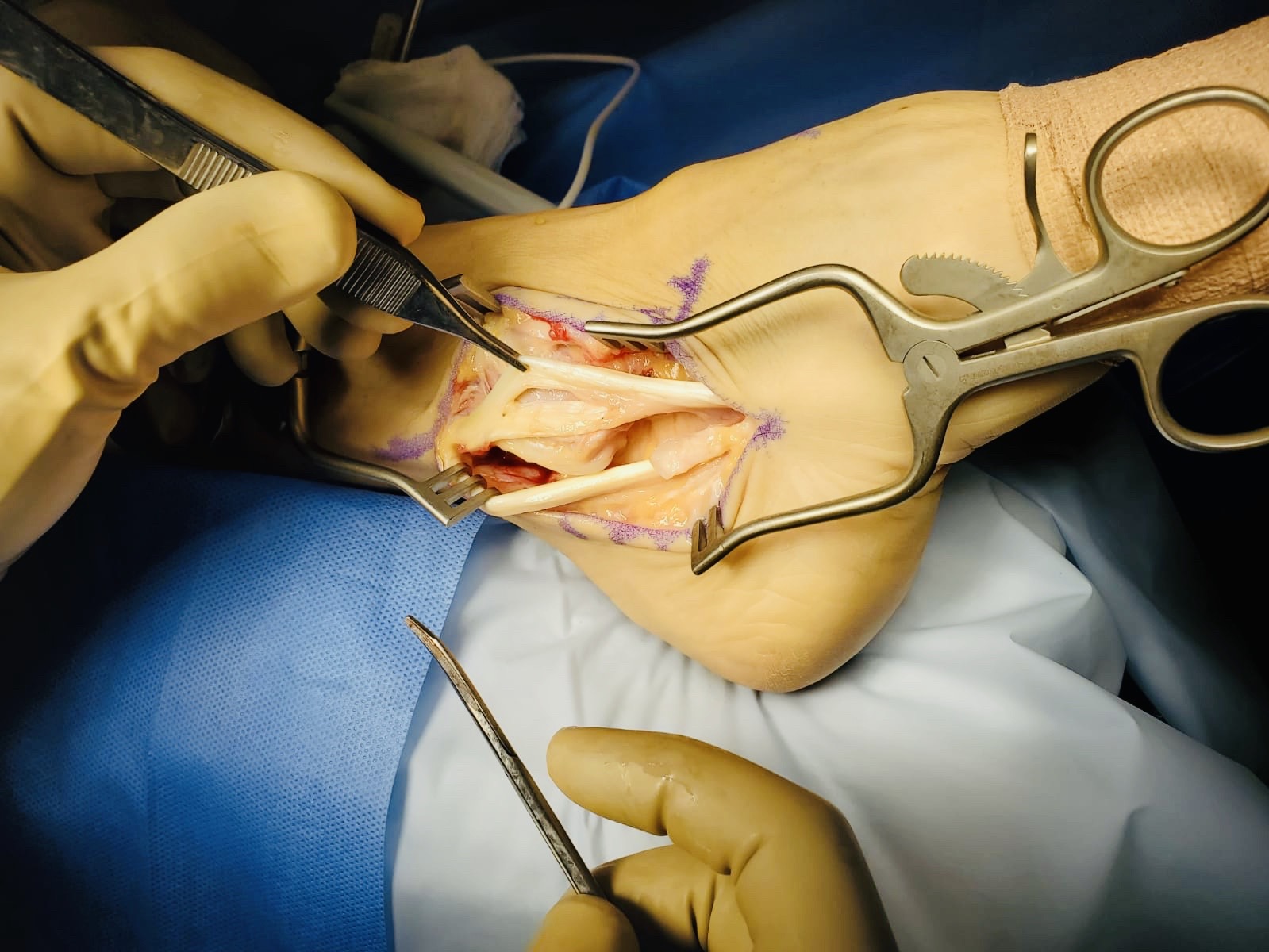
Surgical Considerations
Conservative treatment is usually sufficient for injuries to the peroneus brevis tendon; surgery to reattach or reconstruct the tendon may be necessary for highly active individuals. Different repair techniques are appropriate depending on the specific injury and grade of damage to the peroneus tendon. Peroneal tendon subluxation, for example, can be managed via a direct retinaculum repair, a deepening of the retro-malleolar groove, tendon grafting, or rerouting procedures.[20]
The peroneus brevis muscle is used in reconstructive and plastic surgery of the lower extremity, most commonly in non-healing wounds related to diabetic lower extremity ulcers. Plastic surgeons use the peroneus brevis muscle flap to reconstruct small defects in the lower third of the anterior leg.[21] In addition, the muscle and the peroneal artery can be transposed to small distal leg wounds.[22]
Clinical Significance
Ankle and foot injuries are common in the occupational setting and during amateur and professional sporting activities.[23] Ankle sprain has significant deleterious health and quality of life burden, with chronic pain reported up to 6 years post-injury in between 50% and 79% of individuals.[24] Furthermore, ankle injury is associated with a general reduction in overall physical activity and, therefore, general well-being and health.[25] Awareness of a few common pathologies related to the peroneus brevis muscle and tendon can assist in diagnosing cases of ankle and foot injury. The most common injuries to the peroneus brevis muscle are to its tendon in the form of tendon sprain, dislocation, or splitting.[26]
The tendinous insertion of the peroneus brevis can be injured following an inversion or supination injury resulting in a tendon sprain. For example, during an ankle sprain, the peroneus brevis can be torn, presenting as persistent swelling along the lateral aspect of the ankle at the peroneal tendon sheath. Likewise, supination-adduction injuries to the ankle often involve damage to the lateral ligaments of the ankle, fracture of the distal fibula, and possibly an injury to the peroneal tendons and peroneal retinacula. Occasionally, the base of the fifth metatarsal is also fractured in a lateral ankle sprain, and the peroneus brevis tendon may pull on and detach the bone at the metaphyseal-diaphyseal junction, which is called a Jones fracture.[27] This can occur as either an avulsion or oblique/spiral-type fracture. Additionally, a strike to the lateral aspect of the foot can result in a laceration of the peroneal brevis tendon.
There is a groove in the posterior aspect of the distal fibula where the tendon of the peroneus brevis muscle sits with the tendon of the peroneus longus behind it. The groove is variable in depth and, in some instances, shallow; this is why the peroneal tendons are the most commonly dislocated ankle tendons. Another cause for tendon dislocation is the peroneus brevis tendon rubbing on the fibula, causing an inflammatory periosteal reaction and bony proliferation, which can cause chronic subluxation or displacement of the peroneal tendons. A longitudinal (vertically oriented) split of the peroneus tendon can also occur with subluxation. Furthermore, a low-lying or inferiorly positioned peroneus brevis muscle belly can cause tendon problems and lead to instability, dislocation, tendonitis, or tendon tears.[28]
Media
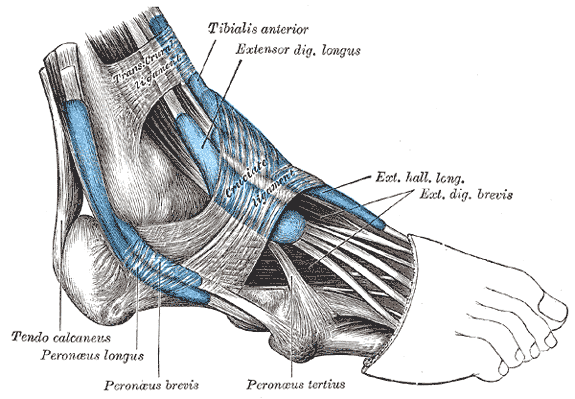
(Click Image to Enlarge)
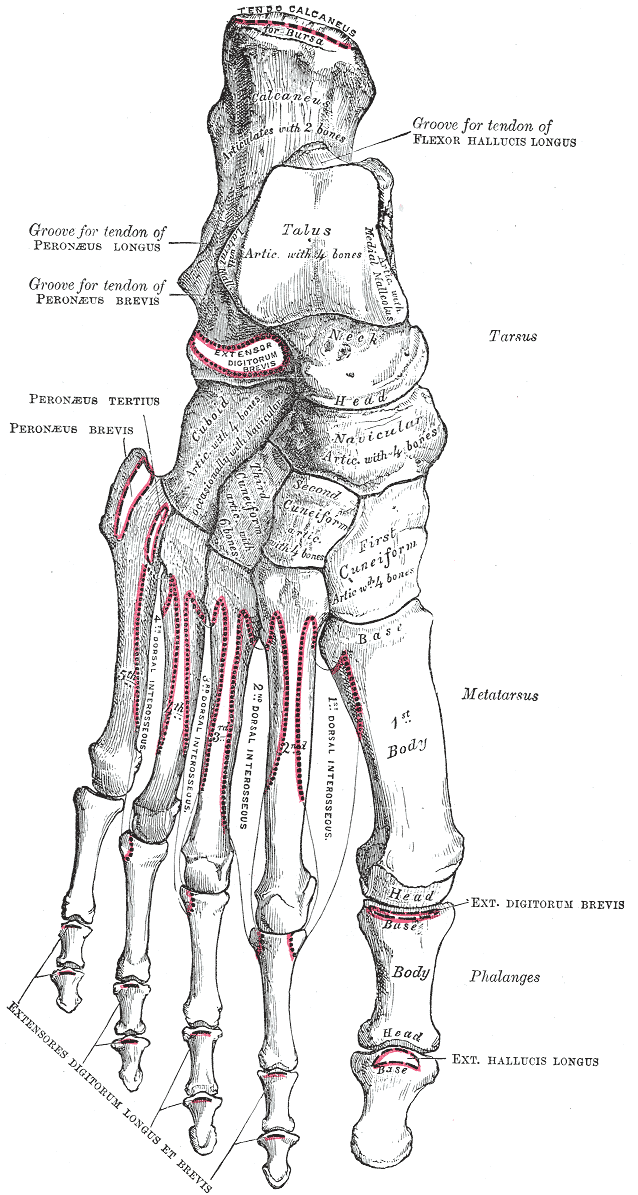
Anatomy of the Dorsal Surface of Right Foot Bones. Anatomy includes tendo calcaneus, bursa, calcaneus, flexor hallucis longus, talus, peroneus longus, peroneus brevis, tarsus, metatarsus, phalanges, digitorum brevis, peroneus tertius, peroneus brevis, cuboid, navicular, cuneiform, dorsal interosseous, extensores, digitorum, longus, brevis, and hallucis longus.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Vohra S, Arnold G, Doshi S, Marcantonio D. Normal MR imaging anatomy of the thigh and leg. Magnetic resonance imaging clinics of North America. 2011 Aug:19(3):621-36, ix. doi: 10.1016/j.mric.2011.05.011. Epub 2011 Jun 14 [PubMed PMID: 21816335]
Mateen S, Ali S, Meyr AJ. Normal Distal Excursion of the Peroneus Brevis Myotendinous Junction. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2021 Oct 22:():. pii: S1067-2516(21)00398-7. doi: 10.1053/j.jfas.2021.10.013. Epub 2021 Oct 22 [PubMed PMID: 34785130]
Imre N, Kocabiyik N, Sanal HT, Uysal M, Ozan H, Yazar F. The peroneus brevis tendon at its insertion site on fifth metatarsal bone. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2016 Mar:22(1):41-5. doi: 10.1016/j.fas.2015.04.009. Epub 2015 Jun 14 [PubMed PMID: 26869499]
Davda K, Malhotra K, O'Donnell P, Singh D, Cullen N. Peroneal tendon disorders. EFORT open reviews. 2017 Jun:2(6):281-292. doi: 10.1302/2058-5241.2.160047. Epub 2017 Jun 22 [PubMed PMID: 28736620]
Mabit C, Salanne P, Boncoeur-Martel MP, Fiorenza F, Valleix D, Descottes B, Caix M. [The lateral retromalleolar groove: a radio-anatomic study]. Bulletin de l'Association des anatomistes. 1996 Jun:80(249):17-21 [PubMed PMID: 9102053]
Drakonaki EE, Gataa KG, Solidakis N, Szaro P. Anatomical variations and interconnections of the superior peroneal retinaculum to adjacent lateral ankle structures: a preliminary imaging anatomy study. Journal of ultrasonography. 2021:21(84):12-21. doi: 10.15557/JoU.2021.0003. Epub 2021 Mar 8 [PubMed PMID: 33791112]
Gomes MDR, Pinto AP, Fabián AA, Gomes TJM, Navarro A, Oliva XM. Insertional anatomy of peroneal brevis and longus tendon - A cadaveric study. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2019 Oct:25(5):636-639. doi: 10.1016/j.fas.2018.07.005. Epub 2018 Jul 23 [PubMed PMID: 30321932]
Bavdek R, Zdolšek A, Strojnik V, Dolenec A. Peroneal muscle activity during different types of walking. Journal of foot and ankle research. 2018:11():50. doi: 10.1186/s13047-018-0291-0. Epub 2018 Sep 3 [PubMed PMID: 30202446]
Karykowska A, Rohan-Fugiel A, Mączka G, Grzelak J, Gworys B, Tarkowski V, Domagała Z. Topography of muscular branches of the superficial fibular nerve based on anatomical preparation of human foetuses. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2021 Sep:237():151728. doi: 10.1016/j.aanat.2021.151728. Epub 2021 Apr 3 [PubMed PMID: 33823227]
Ohmura Y, Morokuma S, Kato K, Kuniyoshi Y. Species-specific Posture of Human Foetus in Late First Trimester. Scientific reports. 2018 Jan 8:8(1):27. doi: 10.1038/s41598-017-18384-w. Epub 2018 Jan 8 [PubMed PMID: 29311655]
Gosselin MM, Haynes JA, McCormick JJ, Johnson JE, Klein SE. The Arterial Anatomy of the Lateral Ligament Complex of the Ankle: A Cadaveric Study. The American journal of sports medicine. 2019 Jan:47(1):138-143. doi: 10.1177/0363546518808060. Epub 2018 Nov 19 [PubMed PMID: 30452871]
Uhl JF, Gillot C. Anatomy of the veno-muscular pumps of the lower limb. Phlebology. 2015 Apr:30(3):180-93. doi: 10.1177/0268355513517686. Epub 2014 Jan 10 [PubMed PMID: 24415543]
Solomon LB, Ferris L, Tedman R, Henneberg M. Surgical anatomy of the sural and superficial fibular nerves with an emphasis on the approach to the lateral malleolus. Journal of anatomy. 2001 Dec:199(Pt 6):717-23 [PubMed PMID: 11787825]
Bilgili MG, Kaynak G, Botanlioğlu H, Basaran SH, Ercin E, Baca E, Uzun I. Peroneus quartus: prevalance and clinical importance. Archives of orthopaedic and trauma surgery. 2014 Apr:134(4):481-7. doi: 10.1007/s00402-014-1937-4. Epub 2014 Feb 14 [PubMed PMID: 24525795]
Sobel M, Levy ME, Bohne WH. Congenital variations of the peroneus quartus muscle: an anatomic study. Foot & ankle. 1990 Oct:11(2):81-9 [PubMed PMID: 2265813]
Zammit J, Singh D. The peroneus quartus muscle. Anatomy and clinical relevance. The Journal of bone and joint surgery. British volume. 2003 Nov:85(8):1134-7 [PubMed PMID: 14653594]
Level 2 (mid-level) evidenceWang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005 May-Jun:25(3):587-602 [PubMed PMID: 15888611]
Mirmiran R, Squire C, Wassell D. Prevalence and Role of a Low-Lying Peroneus Brevis Muscle Belly in Patients With Peroneal Tendon Pathologic Features: A Potential Source of Tendon Subluxation. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2015 Sep-Oct:54(5):872-5. doi: 10.1053/j.jfas.2015.02.012. Epub 2015 May 19 [PubMed PMID: 25998478]
Geller J, Lin S, Cordas D, Vieira P. Relationship of a low-lying muscle belly to tears of the peroneus brevis tendon. American journal of orthopedics (Belle Mead, N.J.). 2003 Nov:32(11):541-4 [PubMed PMID: 14653483]
Pitarini A, Anastasia M, Kennedy D, Sumargono E, Kholinne E. The Surgical Procedure in Managing Peroneal Tendon Injury: A Case Series. Orthopedic research and reviews. 2022:14():255-262. doi: 10.2147/ORR.S351356. Epub 2022 Jul 27 [PubMed PMID: 35923302]
Level 2 (mid-level) evidenceSchubert CD, von Freyhold-Hünecken J, Bittrich T, Onken ML, Tomala L, Montenegro V, Elsner J. Distally Based Peroneus Brevis Muscle Flap for Lower Extremity Defect Reconstruction in Severely Ill Multimorbid Patients. Zeitschrift fur Orthopadie und Unfallchirurgie. 2022 Aug:160(4):422-430. doi: 10.1055/a-1373-6564. Epub 2021 Apr 19 [PubMed PMID: 33873224]
Ebrahiem AA, Manas RK, Vinagre G. Distally Based Sural Artery Peroneus Flap (DBSPF) for Foot and Ankle Reconstruction. Plastic and reconstructive surgery. Global open. 2017 Apr:5(4):e1276. doi: 10.1097/GOX.0000000000001276. Epub 2017 Apr 18 [PubMed PMID: 28507850]
Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports medicine (Auckland, N.Z.). 2014 Jan:44(1):123-40. doi: 10.1007/s40279-013-0102-5. Epub [PubMed PMID: 24105612]
Level 1 (high-level) evidenceAl Adal S, Pourkazemi F, Mackey M, Hiller CE. The Prevalence of Pain in People With Chronic Ankle Instability: A Systematic Review. Journal of athletic training. 2019 Jun:54(6):662-670. doi: 10.4085/1062-6050-531-17. Epub 2019 Jun 11 [PubMed PMID: 31184959]
Level 1 (high-level) evidenceGribble PA, Kleis RE, Simon JE, Vela LI, Thomas AC. Differences in health-related quality of life among patients after ankle injury. Frontiers in sports and active living. 2022:4():909921. doi: 10.3389/fspor.2022.909921. Epub 2022 Aug 3 [PubMed PMID: 35992155]
Level 2 (mid-level) evidencePhilbin TM, Landis GS, Smith B. Peroneal tendon injuries. The Journal of the American Academy of Orthopaedic Surgeons. 2009 May:17(5):306-17 [PubMed PMID: 19411642]
Metzl JA, Bowers MW, Anderson RB. Fifth Metatarsal Jones Fractures: Diagnosis and Treatment. The Journal of the American Academy of Orthopaedic Surgeons. 2022 Feb 15:30(4):e470-e479. doi: 10.5435/JAAOS-D-21-00542. Epub [PubMed PMID: 34932521]
Khan IA, Mahabadi N, D’Abarno A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Lateral Compartment. StatPearls. 2023 Jan:(): [PubMed PMID: 30137811]