Introduction
Herpes simplex ophthalmicus (HSO) is caused by the neurotropic herpes simplex virus type 1 and type 2 and affects all the structures of the eye. Primary infection occurs in the form of blepharoconjunctivitis both in neonates through birth canal transmission and in children through orofacial mucus membrane transmission. Primary infection is often self-limiting, and the virus ascends through the cutaneous nerves and stays latent in the trigeminal nerve ganglion. Upon reactivation due to unfavorable immune conditions, a secondary infection happens involving eyelids, conjunctiva, cornea, uvea, and rarely retina. Antiviral agents, both topical and systemic antivirals, are the treatment of choice. Severe infections and their sequelae can often cause severe impairment to the vision. Once infected, it is impossible to eradicate the virus from the body.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Herpes simplex ophthalmicus is caused by a neurotrophic double-stranded DNA virus with an icosahedral capsid surrounded by a poorly defined tegument (covering). Two types of herpes simplex virus (HSV) affect humans, HSV type 1 (HSV-1) and HSV type 2 (HSV-2). HSV-1 causes orofacial and eye infections by contact from an infected individual, while HSV-2 causes genital disease transmitted sexually. HSV-2 can be transmitted to neonates during birth through HSV-2 infected genitalia of the mothers and to children through orofacial contact by infected adults.
Primary infection occurs in neonates as ophthalmia neonatorum or children less than five years of age as blepharoconjunctivitis. The virus ascends through the cutaneous nerves to stay latent in the trigeminal ganglion. Viral replication is triggered by conditions like fever, menstruation, irradiation, stress, steroid treatment, immunocompromised conditions, etc. to cause secondary infection in adults. Secondary herpes simplex ophthalmicus manifests most commonly as epithelial dendritic keratitis and its recurrences as stromal keratitis.[2]
Epidemiology
Herpes simplex ophthalmicus is a ubiquitous infection and is universal by late adulthood. HSV keratitis is the most common corneal blindness in developing nations. Worldwide, HSV affects between 60-95% of adults. HSV-1 is more commonly affects 70-80% of low socioeconomic groups and 40-60% of improved socioeconomic status.[3] In the United States of America (USA), neonatal HSV infection occurs at a rate of 1 in 3200 deliveries, and 1500 cases are seen every year.[4][5] The USA has a total prevalence of 400,000 cases of HSV keratitis and a total number of episodes at 58,000/year with an incidence of new cases of about 24,000/year. Recurrent disease, estimated to occur in 27% of patients at one year and over 60% at 20 years, commonly causes keratitis, though it can affect all parts of the eye.[6][7]
Pathophysiology
HSV-1 virus commonly causes Herpes simplex ophthalmicus. Rarely HSV-2 infection can occur in neonates from maternal infected genitalia during birth. Primary infection generally occurs through the oropharyngeal mucosa on exposure to secretions of an individual shedding HSV. At the primary site, the virus enters the epithelial cell, replicates, and transports retrogradely through neurons to the dorsal root ganglia of the Trigeminal nerve where it stays latent.[8][9] Recurrent infection due to viral replication in the sensory ganglia is induced by various stimuli like trauma (physical/surgical/laser), ultraviolet radiation, immunosuppression, stress, hormonal changes (menstruation), etc. During the primary infection, CD8+ T cells are primed by the upregulation of chemokine receptors, CXXR3, and CCR10. HSV-specific CD8+ T cells play an important role in recurrent infections.[10][11][12]
HSV infections incite an inconsistent antibody production, which offers only partial protection to recurrences or reinfections. Recurrent viral replication destroys sensory ganglion cells leading to corneal hypesthesia. Corneal hypesthesia or decreased corneal sensation is a hallmark of HSV keratitis. Rong et al. have shown that the cornea is capable of extraneuronal viral latency and later reactivation.[13]
Classification of Herpes Implex Ophthalmicus
- Primary infection:
- Ophthalmia neonatorum
- Blepharoconjunctivitis (children, adults)
- Recurrent infection:
- Blepharoconjunctivitis (adults)
- Herpetic keratitis
- Marginal keratitis
- Necrotizing stromal keratitis
- Metaherpetic keratitis
- Immune-mediated: endotheliitis and keratouveitis.
- Acute retinal necrosis
- Miscellaneous associations: episcleritis, scleritis, epidemic keratoconjunctivitis, ocular cicatricial pemphigoid, erythema multiforme major, ICE syndrome, Possner-Schlossman syndrome, Fuch heterochromic iridocyclitis.[14]
History and Physical
Primary herpes simplex ophthalmicus is an acute infection occurring in a nonimmune host. It can occur in neonates through intrauterine or birth canal transmission or can occur in children through oro-labial transmission from an infected individual. Primary infection can also occur in an adult as a sexually transmitted disease.
- In-utero HSV infection: The fetus can be infected by an ascending genital infection or trans-placentally and is born with cataracts and chorioretinitis.
- Neonatal conjunctivitis: It is transmitted through the birth canal and caused by the HSV-2 virus. Seen between 3-15 days of postpartum life and is associated with lid vesicles. Keratitis or keratouveitis can follow conjunctivitis. Cataract, vitritis, retinitis, retinal detachment, and optic neuritis have all been reported to occur with conjunctivitis.
- Blepharoconjunctivitis: Primary herpes simplex conjunctivitis usually occurs in children less than 5 years old. Features are watery discharge, follicular conjunctivitis, and preauricular lymphadenopathy with cutaneous vesicular eruption over the lids and margins. Most are caused by HSV-1virus. The lesions are diffuse and shed virus for ten days and resolve over 2-3 weeks. Keratitis in the form of punctate epithelial keratitis, marginal infiltrates, or a dendritic ulcer can occur.
Recurrent herpes simplex ophthalmicus occurs due to the reactivation of the latent virus in the trigeminal ganglion. Rong et al have shown that cornea is also capable of extraneuronal viral latency and later reactivation.[13]
- Blepharoconjunctivitis: Lid vesicles are focal along the lid margin or eyelid skin. The weeping ulcers shed virus for only 2-3 days and last for only a week. The nasolacrimal system also gets involved with scarring and leading to epiphora due to punctal stenosis. It is associated with watery discharge, follicular conjunctivitis, and preauricular lymphadenopathy. Conjunctival smears show mononuclear cell infiltrates. Keratitis in the form of punctate epithelial keratitis, marginal infiltrates, or a dendritic ulcer can occur.
- Epithelial Keratitis: It starts as punctate epithelial opacities caused by actively replicating virus. These opacities coalesce centrally and then break down to form central desquamation. The presentation includes mild irritation, redness, watering, photophobia, and corneal hypesthesia.[15]
- Dendritic ulcer: Central epithelial desquamation develops into a dendritic ulcer with mild subepithelial haze, dichotomous branching, and terminal buds. The bed with dead epithelial cells stains with fluorescein, while the margins with virus-laden cells stain with rose bengal. Inadvertent use of topical corticosteroid drops would cause a dendrite to enlarge into a “Geographic ulcer” with amoeboid configuration.[16] Geographic ulcer also develops in immunocompromised patients and untreated longstanding ulcers.
- Endotheliitis (Disciform keratitis): This is an immune-mediated condition that occurs as an immune reaction to a viral antigen or non-replicating viral particles and manifests as localized, diffuse, and linear forms. The localized form is called Disciform keratitis and manifests as central disc-shaped stroma edema with focal keratic precipitates. The diffuse form is accompanied by trabeculitis with elevated intraocular pressure. The linear form may mimic allograft rejection in a corneal graft.
- Metaherpetic keratitis: This neuropathic ulcer presents as a persistent epithelial defect with greyish elevated borders showing epithelial hyperplasia surrounding the ulcer with a subepithelial haze. Reverse staining is seen with rose bengal staining the unhealthy epithelial cells migrating the base of the ulcer while fluorescein leaks between these cells to stain the margins. Decreased corneal sensation, drug toxicity, poor tear film, chronic low-grade inflammation, and deficient neural growth factors contribute to form the Metaherpetic ulcer.
- Marginal Keratitis: Presents as marginal infiltrates similar to staphylococcal immune infiltrates but epithelial ulceration, and diminished corneal sensation helps in the diagnosis of herpes simplex marginal keratitis.
- Necrotizing stromal keratitis: This results from a severe inflammatory response to viral replication in the cornea. Presents as dense stromal infiltration, ulceration, necrosis, and eventually perforation due to corneal melting. Commonly seen in multiple recurrences and mimics microbial keratitis.
- Keratouveitis: Herpes simplex keratouveitis is immune-mediated and presents as unilateral sectoral iritis with mutton fat keratic precipitates and elevated intraocular pressure, often complicated by posterior synechiae and complicated cataract.
- Acute retinal necrosis (ARN): usually caused by the Herpes zoster virus, Herpes simplex virus, Cytomegalovirus, and Epstein-Barr virus. The classic triad of ARN consists of occlusive vasculitis, rapidly progressing peripheral retinal necrosis and vitritis.
Miscellaneous Syndromes
- Episcleritis and scleritis: Rarely associated.[17]
- Epidemic keratoconjunctivitis: HSV can cause a picture like epidemic keratoconjunctivitis and its nearly impossible to differentiate between adenoviral and HSV infection In a Japanese study, it was observed that 3% of cases of epidemic keratoconjunctivitis (EKC) diagnosed clinically were caused by herpes simplex virus.[18]
- Erythema multiforme major: Erythema multiforme major is an immune-mediated type 4 hypersensitivity reaction triggered by drugs and infections caused by Herpes simplex virus, Mycoplasma pneumonia, Epstein-Barr virus, Histoplasmosis, etc. This self-limiting condition presents as target lesions around eyelids with conjunctivitis. Antiviral therapy helps prevent the complication like symblepharon and shortening of fornices.
- Iridocorneal endothelial (ICE) syndromes: HSV DNA has been isolated by the Polymerase chain reaction (PCR) test from corneal endothelium in Iridocorneal endothelial (ICE) syndromes.[19][20]
HSV DNA has also been isolated by the PCR test from aqueous humor samples from patients affected with Posner Schlossman syndrome and Fuch heterochromic iridocyclitis.[21]
Evaluation
Most diagnoses are done clinically or with the slit lamp examination because of the distinct characteristics of the infection. Laboratory diagnosis is done in atypical cases where the clinical picture doesn’t yield a conclusive diagnosis because of drug toxicity, immunosuppression, and polytherapy. The following are the methods to confirm Herpes simplex infection.[22]
- Culture: Virus tissue culture is confirmative and yields positive results in 48 hours of inoculation. Prior rose bengal staining interferes with the culture results as it is viricidal. Immunofluorescent staining of the cells can differentiate between types 1 and 2.[23][24][23]
- Direct Fluorescent Antibody (DFA) Testing: Rapid test but low in specificity and sensitivity. Smear over a slide could obtain results in minutes. Requires a skilled technician and ultraviolet microscope. Fluorescent antibody staining reveals herpetic antigen and is a rapid and reliable test. Fluorescein staining interferes with the test.
- Polymerase chain reaction (PCR) DNA Testing: Polymerase chain reaction test is the preferred test for ocular HSV infection to detect HSV DNA. It is more sensitive than virus culture in the diagnosis of epithelial keratitis. Real-time PCR can differentiate virus shedding from replication by viral quantification. Rapid and more sensitive than culture and can detect virus shedders. Used to identify strains for epidemiological purposes.[25]
- Tzanck Smear: Scrapings are obtained from the corneal epithelium from open cutaneous vesicles and then stained. Giemsa stains of corneal smears show multinucleated giant cells and the Papanicolaou stain shows intranuclear eosinophilic inclusion bodies of Lipschutz (Cowdry type A). Rapid and less expensive tests but low in specificity and sensitivity with the inability to differentiate between type 1 and 2 viruses.
- Cytology: Surface cells are obtained by a brush or impression. Low-cost less sensitive rapid test.
- Enzyme-linked immunosorbent assay (ELISA): ELISA kits yield rapid results and use monoclonal antibodies against HSV antigens.[26]
- Serum Antibody Testing: Most adults show positive IgG for HSV thereby making this test of less use. Antibody testing in children and infants is rarely done as most of the cases can be diagnosed clinically. IgM antibodies are seen in primary infection with seroconversion to IgG in 2 to 4 weeks after the infection.[27]
Treatment / Management
Antiviral medication is the mainstay of treatment for the herpetic epithelial disease. They interfere with DNA synthesis by inhibiting viral DNA polymerase. Acyclovir and Ganciclovir specifically inhibit thymidine kinase and polymerase and are least toxic. Topical Acyclovir 3% ointment, Ganciclovir 3% gel, and Trifluridine 1% solutions are used regularly at five times/day. Oral preparations are Acyclovir 400 mg 5 times/day and Valacyclovir 500 mg thrice daily. Intravenously Acyclovir 10mg/kg thrice daily is the usual dosage. Corticosteroids are the mainstay of treatment for stromal keratitis and Keratouveitis. 1% prednisolone acetate or 0.1% dexamethasone are commonly used under antiviral cover to prevent recurrence and reactivation of HSV infection.[28][29](B2)
- Neonatal conjunctivitis: Intravenous Acyclovir 60 mg/kg/day every 8 hours for 14 days for SEM (Skin-Eye-Mouth) disease. Extend the treatment for 21 days for central nervous system involvement and the disseminated disease.[30] Oral suppressive acyclovir therapy (300 mg twice or thrice a day) to pregnant women with active, recurrent genital HSV infection from 36 weeks of gestation and elective Caesarean surgery before the breakage of membranes offer the best prevention for birth-related transmission of the virus.
- Blepharoconjunctivitis: Resolves spontaneously in a week or two. Some patients might need acyclovir eye ointment for keratitis or lid vesicles.
- Dendritic ulcer: Most cases resolve spontaneously. Topical antivirals provide faster resolution in marginal ulcers, ulcers larger than 4 mm, and ulcers with stromal inflammation. Topical antivirals provide faster resolution with less scarring. Topical acyclovir 3% ointment or Ganciclovir 0.15% gel applied five times a day for two weeks will heal most of the ulcers. Surface debridement of the ulcer helps in reducing the viral load and offers better penetration of the medication. Toxicity is uncommon but presents as diffuse punctate erosions or follicular conjunctivitis. Most of the time, adding preservative-free lubricating eyedrops would be enough.
- Disciform keratitis: The mainstay of treatment is corticosteroid eyedrops under topical Acyclovir cover for ten weeks. The antiviral cover is essential as any reactivation of the infection under steroid drops would lead to devastating stromal necrosis. Disciform keratitis is prone to recurrence leading to dense corneal opacity impairing vision. Recurrent episodes need long term oral acyclovir prophylaxis (400 mg bid) as it is proven to be beneficial in preventing recurrent attacks as per the Herpetic eye disease study.[31]
- Metaherpetic keratitis: The mainstay of treatment is first to eliminate the main cause for the persistent epithelial defect. Drug toxicity should be detected and avoided. Dry eye being an aggravating factor for neuropathic keratitis, is treated with preservative-free lubricating drops, punctal occlusion, and cyclosporin eyedrops. Epithelial healing is promoted by autologous serum eyedrops and bandage contact lenses. Resistant cases are treated with an amniotic membrane graft, Gunderson conjunctival fap, or with a central tarsorrhaphy. Cautious use of low potent topical corticosteroids like Fluorometholone is used to treat the underlying inflammation. Non-steroidal anti-inflammatory eyedrops are avoided as they might induce corneal melting leading to perforation.
- Stromal keratouveitis: Topical steroids either 1% prednisolone acetate or 0.1% dexamethasone resolves the underlying immune-mediated inflammation and prevents scarring. The topical antiviral cover is essential as HSV reactivation causes severe epithelial disease or stromal necrosis. Oral Acyclovir 400 mg twice daily for six months to one year prevents recurrences.
- Acute retinal necrosis(ARN): ARN is an ophthalmic emergency and needs to be treated immediately. The goal is to protect the fellow eye from the infection. Intravenous Acyclovir 10 mg/kg 3 times daily for 5 to 10 days depending on the response followed by oral acyclovir 800 mg five times daily orally for six weeks to 3 months.[32] (A1)
Surgery is usually done for dense stromal scarring, non-healing ulcers, and impending perforations as in stromal necrosis.
- Stromal melting: Penetrating keratoplasty may be needed with antiviral medication coverage. Long term oral acyclovir prophylaxis needed to prevent the recurrence of herpes simplex infection in the graft
- Corneal perforation: There needs to be cyanoacrylate glue application or placement of a corneal patch graft
- Persistent epithelial defect: Amniotic membrane grafting or Gunderson conjunctival flap or central tarsorrhaphy is usually performed. The amniotic membrane acts by lowering the inflammatory cells and matrix metalloproteinase levels on the corneas enabling better healing of the epithelial defect. Amniotic membrane causes reduced expression and activity of MMP-8 and nine and increases expression of TIMP-1 and 2.[33]
- Dense stromal scarring: Penetrating keratoplasty (PKP) is done 6 months after the infection is fully controlled. It has a poor prognosis with high graft recurrence and rejection rates. Prophylactic acyclovir 400 mg twice daily should be started prior to the surgery and continued until a year after the surgery to prevent recurrences.[34][35][36] (A1)
Differential Diagnosis
Ophthalmia Neonatorum
- Infective keratitis
- Dacryocystitis
- Congenital nasolacrimal duct obstruction
- Congenital glaucoma
- Orbital and pre-septal cellulitis
HSV Keratitis
- Herpes zoster keratitis
- Microbial keratitis
- Adenoviral keratitis
- Acanthamoeba keratitis
- Drug toxicity
- Epithelial regeneration line
- Chronic Contact lens wear
HSV Stromal/Interstitial Keratitis
- Varicella-zoster keratitis
- Epstein-Barr virus keratitis
- Measles keratitis
- Mumps keratitis
- Cogan’s syndrome
- Syphilis
- Lyme’s disease
Corneal Hypesthesia
- Herpes virus keratitis
- Chronic contact lens wear
- Lesions of Trigeminal nerve: acoustic neuroma/surgery/trauma
- Diabetes
- Topical medications: anesthetics, beta-blockers, and nonsteroidal anti-inflammatory agents
- Laser surgery: surface ablation and Lasik.[37]
Prognosis
Ophthalmia neonatorum and primary blepharoconjunctivitis respond well with antiviral treatment and have a very good prognosis with the least complications. HSV epithelial keratitis resolves within 1 to 2 weeks with topical antiviral therapy. Stromal keratitis and iritis occur in 25% of people affected with epithelial keratitis and often recurs and results in corneal scarring, glaucoma, neovascularization, and corneal melting leading to irreversible loss of vision. The Australian corneal graft registry has reported that 4% of their failed grafts are due to HSV ophthalmicus.[38] Acute retinal necrosis has a very poor visual prognosis, with 64% of affected eyes have a final vision of 20/200 or worse due to vision-threatening complications like retinal detachment, optic neuropathy, macular edema, and retinal ischemia.[39]
Complications
- Infectious keratitis
- Dense corneal stromal scarring
- Chronic dry eye
- Chronic uveitis
- Corneal melting
- Corneal neovascularization
- Persistent epithelial defect
- Secondary glaucoma
- Complicated cataract
- Posterior synechiae
- Peripheral anterior synechiae
- Chronic vitritis with vitreous condensation and floaters
- Retinal detachment, optic neuritis, cystoid macular edema, and retinal ischemia in patients with acute retinal necrosis[40]
Deterrence and Patient Education
Educating patients and care providers about the visually devastating nature of the HSV keratitis and the need for adherence to treatment are very important. As herpes simplex virus is ubiquitous in nature and nearly impossible to avoid infection, the following measures will help in the prevention of both acquiring and recurrence of the disease.
- Oral antiviral prophylaxis of pregnant women at 36 weeks and opting for elective cesarean delivery prevents neonatal spread during birth
- Avoid oro-labial contacts of adults to newborns.
- Long term oral antiviral prophylaxis prevents recurrences in corneal graft and stromal keratitis and keratouveitis.
- Long term oral antiviral prophylaxis prevents recurrences in corneal graft following penetrating keratoplasty for uncontrolled epithelial keratitis or for dense stromal scar secondary to HSV keratitis
Enhancing Healthcare Team Outcomes
The primary care physician, pediatricians, and health care workers should be educated and made well aware of the signs and symptoms of ophthalmia neonatorum and primary HSV blepharoconjunctivitis. Prompt referral pathways to primary care physicians or an ophthalmologist should be established to treat HSV ophthalmia neonatorum without delay. Primary care physicians should be trained to stain the corneas with the fluorescein and examine under cobalt blue light for a possible dendrite. Every physician and healthcare worker should be trained to assess corneal sensations. A proper detailed history of previous episodes of HSV keratitis should be elicited before starting the patients on topical steroids or before corneal surgical procedures. As of now, there isn’t a successful vaccine to prevent herpes simplex ophthalmicus. The treatment guidelines are provided by the Herpetic eye disease study (HEDS).
Herpetic eye disease study (HEDS) consists of five randomized double-masked placebo-controlled multicentre trials designed to evaluate oral acyclovir (400 mg twice daily) for herpetic stromal keratitis.[41] [Level 1] The conclusions of the HEDS trial are as follows:
- Oral acyclovir has no significant benefit in HSV stromal keratitis already on topical antiviral and steroid medications.[42]
- Topical steroids are beneficial than placebo in herpetic stromal keratitis.[43]
- A possible benefit of oral acyclovir in herpetic iridocyclitis.[44]
- No added benefit of oral acyclovir to topical trifluridine in the prevention of anterior uveitis or stromal disease in patients with HSV epithelial keratitis.[45]
- Long-term oral acyclovir prevents recurrences in patients with a history of HSV stromal keratitis.[35]
Media
(Click Image to Enlarge)
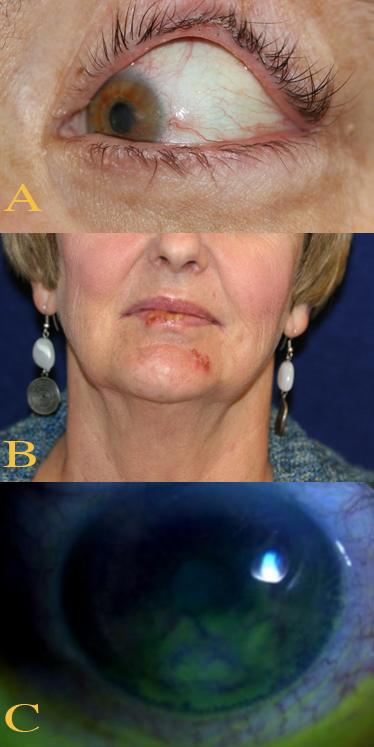
Ocular and Perioral Involvement in Herpes Simplex Virus Infection. Various clinical findings of herpetic keratitis are demonstrated. In image A (top), herpetic keratitis with neovascularization of the cornea is noted. In image B (middle), HSV type 1 lesions are seen on the patient's lips and chin. Image C (bottom) demonstrates findings of stage 1 neurotrophic keratitis, including fluorescein epithelial staining with Gaule spots, which are scattered areas of dried epithelium.
Contributed by BCK Patel, MD, FRCS
References
Liang F, Glans H, Enoksson SL, Kolios AGA, Loré K, Nilsson J. Recurrent Herpes Zoster Ophthalmicus in a Patient With a Novel Toll-Like Receptor 3 Variant Linked to Compromised Activation Capacity in Fibroblasts. The Journal of infectious diseases. 2020 Mar 28:221(8):1295-1303. doi: 10.1093/infdis/jiz229. Epub [PubMed PMID: 31268141]
Kim JS, Rafailov L, Leyngold IM. Corneal Neurotization for Postherpetic Neurotrophic Keratopathy: Initial Experience and Clinical Outcomes. Ophthalmic plastic and reconstructive surgery. 2021 Jan-Feb 01:37(1):42-50. doi: 10.1097/IOP.0000000000001676. Epub [PubMed PMID: 32332687]
Level 2 (mid-level) evidenceChayavichitsilp P, Buckwalter JV, Krakowski AC, Friedlander SF. Herpes simplex. Pediatrics in review. 2009 Apr:30(4):119-29; quiz 130. doi: 10.1542/pir.30-4-119. Epub [PubMed PMID: 19339385]
Level 2 (mid-level) evidenceBrown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L. Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant. JAMA. 2003 Jan 8:289(2):203-9 [PubMed PMID: 12517231]
Kimberlin DW. Neonatal herpes simplex infection. Clinical microbiology reviews. 2004 Jan:17(1):1-13 [PubMed PMID: 14726453]
Liesegang TJ, Melton LJ 3rd, Daly PJ, Ilstrup DM. Epidemiology of ocular herpes simplex. Incidence in Rochester, Minn, 1950 through 1982. Archives of ophthalmology (Chicago, Ill. : 1960). 1989 Aug:107(8):1155-9 [PubMed PMID: 2787981]
Level 2 (mid-level) evidenceYoung RC, Hodge DO, Liesegang TJ, Baratz KH. Incidence, recurrence, and outcomes of herpes simplex virus eye disease in Olmsted County, Minnesota, 1976-2007: the effect of oral antiviral prophylaxis. Archives of ophthalmology (Chicago, Ill. : 1960). 2010 Sep:128(9):1178-83. doi: 10.1001/archophthalmol.2010.187. Epub [PubMed PMID: 20837803]
Kaye SB, Lynas C, Patterson A, Risk JM, McCarthy K, Hart CA. Evidence for herpes simplex viral latency in the human cornea. The British journal of ophthalmology. 1991 Apr:75(4):195-200 [PubMed PMID: 1850616]
Labetoulle M, Maillet S, Efstathiou S, Dezelee S, Frau E, Lafay F. HSV1 latency sites after inoculation in the lip: assessment of their localization and connections to the eye. Investigative ophthalmology & visual science. 2003 Jan:44(1):217-25 [PubMed PMID: 12506078]
Level 3 (low-level) evidenceHensel MT, Peng T, Cheng A, De Rosa SC, Wald A, Laing KJ, Jing L, Dong L, Magaret AS, Koelle DM. Selective Expression of CCR10 and CXCR3 by Circulating Human Herpes Simplex Virus-Specific CD8 T Cells. Journal of virology. 2017 Oct 1:91(19):. doi: 10.1128/JVI.00810-17. Epub 2017 Sep 12 [PubMed PMID: 28701399]
Stuart PM, Summers B, Morris JE, Morrison LA, Leib DA. CD8(+) T cells control corneal disease following ocular infection with herpes simplex virus type 1. The Journal of general virology. 2004 Jul:85(Pt 7):2055-2063. doi: 10.1099/vir.0.80049-0. Epub [PubMed PMID: 15218191]
Level 3 (low-level) evidenceBanerjee K, Biswas PS, Kumaraguru U, Schoenberger SP, Rouse BT. Protective and pathological roles of virus-specific and bystander CD8+ T cells in herpetic stromal keratitis. Journal of immunology (Baltimore, Md. : 1950). 2004 Dec 15:173(12):7575-83 [PubMed PMID: 15585885]
Level 3 (low-level) evidenceRong BL, Pavan-Langston D, Weng QP, Martinez R, Cherry JM, Dunkel EC. Detection of herpes simplex virus thymidine kinase and latency-associated transcript gene sequences in human herpetic corneas by polymerase chain reaction amplification. Investigative ophthalmology & visual science. 1991 May:32(6):1808-15 [PubMed PMID: 1851732]
Gore DM, Gore SK, Visser L. Progressive outer retinal necrosis: outcomes in the intravitreal era. Archives of ophthalmology (Chicago, Ill. : 1960). 2012 Jun:130(6):700-6. doi: 10.1001/archophthalmol.2011.2622. Epub [PubMed PMID: 22801826]
Level 2 (mid-level) evidenceKodama T, Hayasaka S, Setogawa T. Immunofluorescent staining and corneal sensitivity in patients suspected of having herpes simplex keratitis. American journal of ophthalmology. 1992 Feb 15:113(2):187-9 [PubMed PMID: 1312774]
Wilhelmus KR, Coster DJ, Donovan HC, Falcon MG, Jones BR. Prognostic indicators of herpetic keratitis. Analysis of a five-year observation period after corneal ulceration. Archives of ophthalmology (Chicago, Ill. : 1960). 1981 Sep:99(9):1578-82 [PubMed PMID: 6793030]
Bhat PV, Jakobiec FA, Kurbanyan K, Zhao T, Foster CS. Chronic herpes simplex scleritis: characterization of 9 cases of an underrecognized clinical entity. American journal of ophthalmology. 2009 Nov:148(5):779-789.e2. doi: 10.1016/j.ajo.2009.06.025. Epub 2009 Aug 11 [PubMed PMID: 19674728]
Level 2 (mid-level) evidenceUchio E, Takeuchi S, Itoh N, Matsuura N, Ohno S, Aoki K. Clinical and epidemiological features of acute follicular conjunctivitis with special reference to that caused by herpes simplex virus type 1. The British journal of ophthalmology. 2000 Sep:84(9):968-72 [PubMed PMID: 10966946]
Level 2 (mid-level) evidenceAlvarado JA, Underwood JL, Green WR, Wu S, Murphy CG, Hwang DG, Moore TE, O'Day D. Detection of herpes simplex viral DNA in the iridocorneal endothelial syndrome. Archives of ophthalmology (Chicago, Ill. : 1960). 1994 Dec:112(12):1601-9 [PubMed PMID: 7993217]
Hooks JJ, Kupfer C. Herpes simplex virus in iridocorneal endothelial syndrome. Archives of ophthalmology (Chicago, Ill. : 1960). 1995 Oct:113(10):1226-8 [PubMed PMID: 7575245]
Level 3 (low-level) evidenceBarequet IS, Li Q, Wang Y, O'Brien TP, Hooks JJ, Stark WJ. Herpes simplex virus DNA identification from aqueous fluid in Fuchs heterochromic iridocyclitis. American journal of ophthalmology. 2000 May:129(5):672-3 [PubMed PMID: 10844066]
Level 3 (low-level) evidenceSingh A, Preiksaitis J, Ferenczy A, Romanowski B. The laboratory diagnosis of herpes simplex virus infections. The Canadian journal of infectious diseases & medical microbiology = Journal canadien des maladies infectieuses et de la microbiologie medicale. 2005 Mar:16(2):92-8 [PubMed PMID: 18159535]
Brooks SE, Kaza V, Nakamura T, Trousdale MD. Photoinactivation of herpes simplex virus by rose bengal and fluorescein. In vitro and in vivo studies. Cornea. 1994 Jan:13(1):43-50 [PubMed PMID: 8131406]
Level 3 (low-level) evidenceStroop WG, Chen TM, Chodosh J, Kienzle TE, Stroop JL, Ling JY, Miles DA. PCR assessment of HSV-1 corneal infection in animals treated with rose bengal and lissamine green B. Investigative ophthalmology & visual science. 2000 Jul:41(8):2096-102 [PubMed PMID: 10892849]
Level 3 (low-level) evidenceBispo PJM, Davoudi S, Sahm ML, Ren A, Miller J, Romano J, Sobrin L, Gilmore MS. Rapid Detection and Identification of Uveitis Pathogens by Qualitative Multiplex Real-Time PCR. Investigative ophthalmology & visual science. 2018 Jan 1:59(1):582-589. doi: 10.1167/iovs.17-22597. Epub [PubMed PMID: 29372257]
Level 2 (mid-level) evidenceMadhavan HN, Priya K. The diagnostic significance of enzyme linked immuno-sorbent assay for herpes simplex, varicella zoster and cytomegalovirus retinitis. Indian journal of ophthalmology. 2003 Mar:51(1):71-5 [PubMed PMID: 12701866]
Souissi S, Fardeau C, Le HM, Rozenberg F, Bodaghi B, Le Hoang P. Chronic Herpetic Retinitis: Clinical Features and Long-Term Outcomes. Ocular immunology and inflammation. 2018:26(1):94-103. doi: 10.1080/09273948.2017.1327079. Epub 2017 Jun 19 [PubMed PMID: 28628343]
Carter SB, Cohen EJ. Development of Herpes Simplex Virus Infectious Epithelial Keratitis During Oral Acyclovir Therapy and Response to Topical Antivirals. Cornea. 2016 May:35(5):692-5. doi: 10.1097/ICO.0000000000000806. Epub [PubMed PMID: 26989961]
Duan R, de Vries RD, Osterhaus AD, Remeijer L, Verjans GM. Acyclovir-resistant corneal HSV-1 isolates from patients with herpetic keratitis. The Journal of infectious diseases. 2008 Sep 1:198(5):659-63. doi: 10.1086/590668. Epub [PubMed PMID: 18627246]
Level 2 (mid-level) evidenceKimberlin DW, Lin CY, Jacobs RF, Powell DA, Frenkel LM, Gruber WC, Rathore M, Bradley JS, Diaz PS, Kumar M, Arvin AM, Gutierrez K, Shelton M, Weiner LB, Sleasman JW, de Sierra TM, Soong SJ, Kiell J, Lakeman FD, Whitley RJ, National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. Natural history of neonatal herpes simplex virus infections in the acyclovir era. Pediatrics. 2001 Aug:108(2):223-9 [PubMed PMID: 11483781]
. Acyclovir for the prevention of recurrent herpes simplex virus eye disease. Herpetic Eye Disease Study Group. The New England journal of medicine. 1998 Jul 30:339(5):300-6 [PubMed PMID: 9696640]
Level 1 (high-level) evidenceTam PM, Hooper CY, Lightman S. Antiviral selection in the management of acute retinal necrosis. Clinical ophthalmology (Auckland, N.Z.). 2010 Feb 2:4():11-20 [PubMed PMID: 20169044]
Heiligenhaus A, Li HF, Yang Y, Wasmuth S, Steuhl KP, Bauer D. Transplantation of amniotic membrane in murine herpes stromal keratitis modulates matrix metalloproteinases in the cornea. Investigative ophthalmology & visual science. 2005 Nov:46(11):4079-85 [PubMed PMID: 16249483]
Level 3 (low-level) evidenceLomholt JA, Baggesen K, Ehlers N. Recurrence and rejection rates following corneal transplantation for herpes simplex keratitis. Acta ophthalmologica Scandinavica. 1995 Feb:73(1):29-32 [PubMed PMID: 7627755]
van Rooij J, Rijneveld WJ, Remeijer L, Völker-Dieben HJ, Eggink CA, Geerards AJ, Mulder PG, Doornenbal P, Beekhuis WH. Effect of oral acyclovir after penetrating keratoplasty for herpetic keratitis: a placebo-controlled multicenter trial. Ophthalmology. 2003 Oct:110(10):1916-9; discussion 1919 [PubMed PMID: 14522763]
Level 1 (high-level) evidenceBhatt UK, Abdul Karim MN, Prydal JI, Maharajan SV, Fares U. Oral antivirals for preventing recurrent herpes simplex keratitis in people with corneal grafts. The Cochrane database of systematic reviews. 2016 Nov 30:11(11):CD007824 [PubMed PMID: 27902849]
Level 1 (high-level) evidenceGroen-Hakan F, Babu K, Tugal-Tutkun I, Pathanapithoon K, de Boer JH, Smith JR, de Groot-Mijnes JDF, Rothova A. Challenges of Diagnosing Viral Anterior Uveitis. Ocular immunology and inflammation. 2017 Oct:25(5):710-720. doi: 10.1080/09273948.2017.1353105. Epub 2017 Oct 11 [PubMed PMID: 29020537]
Barker NH. Ocular herpes simplex. BMJ clinical evidence. 2008 Jul 23:2008():. pii: 0707. Epub 2008 Jul 23 [PubMed PMID: 19445742]
Level 1 (high-level) evidenceFisher JP, Lewis ML, Blumenkranz M, Culbertson WW, Flynn HW Jr, Clarkson JG, Gass JD, Norton EW. The acute retinal necrosis syndrome. Part 1: Clinical manifestations. Ophthalmology. 1982 Dec:89(12):1309-16 [PubMed PMID: 7162777]
Level 3 (low-level) evidenceSakai JI, Usui Y, Suzuki J, Kezuka T, Goto H. Clinical features of anterior uveitis caused by three different herpes viruses. International ophthalmology. 2019 Dec:39(12):2785-2795. doi: 10.1007/s10792-019-01125-5. Epub 2019 May 27 [PubMed PMID: 31134426]
Dawson CR, Jones DB, Kaufman HE, Barron BA, Hauck WW, Wilhelmus KR. Design and organization of the herpetic eye disease study (HEDS). Current eye research. 1991:10 Suppl():105-10 [PubMed PMID: 1864086]
Level 1 (high-level) evidence. Oral acyclovir for herpes simplex virus eye disease: effect on prevention of epithelial keratitis and stromal keratitis. Herpetic Eye Disease Study Group. Archives of ophthalmology (Chicago, Ill. : 1960). 2000 Aug:118(8):1030-6 [PubMed PMID: 10922194]
Level 1 (high-level) evidenceWilhelmus KR, Gee L, Hauck WW, Kurinij N, Dawson CR, Jones DB, Barron BA, Kaufman HE, Sugar J, Hyndiuk RA. Herpetic Eye Disease Study. A controlled trial of topical corticosteroids for herpes simplex stromal keratitis. Ophthalmology. 1994 Dec:101(12):1883-95; discussion 1895-6 [PubMed PMID: 7997324]
Level 1 (high-level) evidence. A controlled trial of oral acyclovir for iridocyclitis caused by herpes simplex virus. The Herpetic Eye Disease Study Group. Archives of ophthalmology (Chicago, Ill. : 1960). 1996 Sep:114(9):1065-72 [PubMed PMID: 8790090]
Level 1 (high-level) evidence. A controlled trial of oral acyclovir for the prevention of stromal keratitis or iritis in patients with herpes simplex virus epithelial keratitis. The Epithelial Keratitis Trial. The Herpetic Eye Disease Study Group. Archives of ophthalmology (Chicago, Ill. : 1960). 1997 Jun:115(6):703-12 [PubMed PMID: 9194719]
Level 1 (high-level) evidence