Introduction
Blunt eye trauma can result in various intrinsic eye injuries.[1] Blunt trauma can result in open and closed globe injuries. The closed globe injuries are further classified as contusion and lamellar lacerations. Open globe injuries can be laceration and globe rupture.[2] The laceration can be due to penetrating injury, perforation injury, or injury due to an intraocular foreign body (IOFB). Blunt eye trauma can be due to coup, countercoup, and anteroposterior compression or horizontal tissue expansion.[3]
The mode of injury can be a direct blow to the eyeball or accidental blunt trauma. The traumatic lesions of blunt eye trauma are classified as closed globe injury, globe rupture, and extraocular lesions. All the anatomical structures of the eyeball can be affected, as discussed below. The diagnosis is clinical, and rarely laboratory and imaging are warranted. Laboratory investigations are needed in critical patients and patients requiring surgical intervention.[4]
Imaging modalities like X-rays, CT, and MRI is usually required post-operatively. In the case of an impacted foreign body, pre-operatively imaging is required to assess the extent and depth of IOFB. The management depends on the type of injury and the need for surgical intervention. The final visual outcome is governed by mode of trauma, time of presentation, the extent of ocular damage, time of surgical intervention, and post-operative care of the patient.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Blunt eye trauma can manifest as open globe and close globe injury. The closed globe injuries are broadly classified as contusion and lamellar lacerations. Open globe injuries can be divided into laceration and globe rupture. The laceration is secondary to penetrating injury, perforation injury, or injury due to an impacted intraocular foreign body (IOFB). The mechanism of blunt eye trauma can be due to coup, countercoup, and anteroposterior compression or horizontal expansion of the tissue. The mode of injury can be a direct blow to the eyeball or accidental blunt trauma.[6]
Closed globe injuries are often seen in pediatric children while playing with friends and at home. The most common pediatric eye injuries are sports-related trauma, wooden stick injury, and thermal burns due to firecrackers. The other common modes of injury can be assault, workplace trauma, road traffic accidents, self-fall, and nonaccidental injuries.[7] These injuries are more common in adults. Closed globe injuries can also be accidental and are broadly listed as occupational and occupational. The occupational injuries can be due to high-risk occupations like the manufacturing industry, plumbing, mining, and agriculture. Nonoccupational can be sports trauma and domestic violence.[8]
Globe rupture occurs when there is a defect in the cornea, sclera, or both structures. Global rupture often occurs after direct penetrating trauma; however, if sufficient blunt force is applied to the eye, the intraocular pressure can increase enough to rupture the sclera. The high-velocity impact or sharp cutting objects may result in perforating or penetrating open globe injuries.[8] Injuries from sharp toys, knives, scissors, screwdrivers, spectacles, household chickens, pets, and other animals like cranes and swans are prevalent in children. The most common is scissor injury. In adults, the most common causes of blunt eye trauma are workplace injury, stick injury, chemical fall, iron rod, iron nail, quarrel, assault, wood, brick, cement, and battery injury.[9] In elderly age, the most common injury mode is falling from bed, in the bathroom, falling from vehicles resulting in self-inflicted trauma, and falling on the ground. Females are more commonly affected in the elderly age group.
A retrobulbar hematoma is frequently associated with orbital trauma and associated orbital floor fractures. This trauma may also occur iatrogenically during sinus surgery, ocular surgery, or other eye procedures. In the setting of anticoagulation, this may occur in rare scenarios with increases in Valsalva (e.g., from vomiting, straining, or coughing).[10][11]
Epidemiology
The incidence of globe injuries is quoted as 3.5 eye injuries per 100,000 persons, with males constituting about 80% of open globe injuries. Injuries in the pediatric population are more often with sharp objects directly penetrating the globe (e.g., writing utensils, scissors, or knives). The cause is often blunt trauma (e.g., motor vehicle collisions, altercations, or work-related injuries involving hammering). In the elderly, globe rupture is most often a result of falling.[12][13] The incidence of retrobulbar hematoma is rare; it has been recorded as less than 1%. However, there is a strong association between this diagnosis and subsequent blindness.[14] Open globe injuries are more common in males, usually in the age group of 30 to 40 years. After penetrating and perforating, injuries retained intraocular foreign body (IOFB) can be seen in 40% of cases and may be seen while perforation work such as hammering, grinding, and drilling.[15]
A recent analysis from North India gave insights into nonoccupational and occupational. As per the study, nonoccupational trauma constituted 82.3%. There were 23.9% cases of sports-related trauma and 23.6% cases of road traffic accidents. Approximately 89.3% of cases constituted mechanical injuries. The various modes of trauma were wood injury 24.9%, and metallic object 20.9% for open globe injury. The incidence of blunt trauma was three times less than that of sharp objects (56%).[16]]
Landen et al., in their analysis, reported an annual incidence of 3.5 per 100000 cases of perforating injuries in the USA. Another study from Australia reported 2.4 and 7.9% per 1000 cases of nonindigenous and indigenous adults with monocular blindness due to blunt trauma.[17] As per another analysis by Negrel et al., three quarter million patients undergo hospitalization with ocular injuries globally.[18] Ocular trauma is approximately 7% of all body trauma and 10 to 15% of all ophthalmic pathologies. Globally1.6 million people are blind due to ocular trauma, 2.3 million are bilaterally blind, and 1.9 million are monocularly blind. Approximately 90% of all ocular injuries can be prevented.[19]
Pathophysiology
Globe rupture occurs when there is a defect in the cornea, sclera, or both structures. Global rupture often occurs after direct penetrating trauma; however, if sufficient blunt force is applied to the eye, the intraocular pressure can increase enough to rupture the sclera. The rupture site is most commonly near the globe's equator posterior to the insertion of the rectus muscles, which is where the sclera is weakest and thinnest.[20] A retrobulbar hematoma occurs when blood is accumulated in the retrobulbar space. As blood collects behind the eye, there is increased intraocular pressure, which can subsequently cause stretching of the optic nerve. Within several hours, decreased ocular perfusion can lead to permanent blindness.[21]
Injury Division
- Direct or Coup - Direct blow to the eye. e.g., Corneal abrasion
- Countercoup - Due to pressure waves transmitted at the posterior pole. e.g., commotio retinae
- Anteroposterior Compression and Horizontal Expansion - Pressure waves in the anteroposterior and horizontal axes. e.g., globe rupture[22]
Blunt Trauma Division
- Direct -injury to the eye by hand, fist, ball, or blunt instruments like a stick, stone, and iron rod
- Accidental- accidental trauma like a fall from a bike, self-fall, stone injury, cracker injury, etc
Stages of the Mechanism of Blunt Trauma
- Direct impact
- Compression wave force
- Reflected compression wave
- Rebound compression wave[23]
History and Physical
High suspicion for globe injury exists in any patient reporting direct eye trauma, continuing eye pain, and vision deficit. The mechanism of the injury should be elicited and the time it occurred. It is also essential to inquire about any anticoagulant use. In globe rupture, physical examination findings may reveal decreased vision or frank vision loss, the irregular contour of the globe, teardrop pupil, hyphema, or a shallow anterior chamber on the slit-lamp exam. The Seidel sign is positive in globe rupture, indicating the flow of aqueous humor from the injury site in the fluorescein-stained eye. However, if the globe rupture is apparent, Seidel's test should be avoided. The clinical presentation of retrobulbar hematoma is classical with proptosis and severe eye pain. As in globe rupture, vision loss may be reported.[24]
There may be associated periorbital swelling, ecchymosis, or subconjunctival hemorrhage in either of these entities, depending on the mechanism of the injury. Typical symptoms of globe rupture include eye deformity, eye pain, and vision loss, though the deformation may not be readily apparent on the exam, depending on the clinical suggestion. Similarly, a retrobulbar hematoma may present with eye pain and vision loss, but proptosis helps clinch this diagnosis. Both are vision-threatening diagnoses and require emergency ophthalmologic consultation for definitive measures.[25][26][27]
Manifestations
Anterior Segment Manifestations
Conjunctiva
- Subconjunctival hemorrhage
- Conjunctival congestion
- Foreign body of conjunctiva
- Conjunctival tear[28]
Cornea
- Epithelial damage - There can be abrasion, punctate epithelial erosions, epithelial defect, foreign body due to breach in the epithelium and revealed brilliantly on fluorescein staining. If the damage involves the pupillary axis, the vision is grossly impaired.[29]
- Corneal edema - There can be corneal edema due to endothelial injury or extensive damage due to abrasion. Corneal edema usually is associated with stromal edema, and Descemet membrane (D.M.) folds.[30]
- Descemet membrane tear - D.M. tears are vertical tears noticed after birth trauma. Recurrent corneal erosions.[31]
- Recurrent corneal erosions (recurrent keractalgia) - Usually result from fingernail injury. The patients will present as pain, redness, watering, and photophobia due to loose attachment of epithelium to the underlying Bowman's membrane.[32]
- Corneal tear (Partial or lamellar or full-thickness tear) - There can be self-sealed tears or total thickness tears best detected with Seidel's test.[33]
- Blood staining of endothelium - This may be secondary to hyphema or raised IOP and may take as long as two years to clear. The blood staining of endothelium clears from periphery to center.[34]
- Corneal scar - May be seen after a long duration post-trauma, usually after 2-3 months.[35]
- Corneal infiltrate - Blunt trauma can also result in a corneal ulcer.[36]
Sclera
Can have a partial thickness or full thickness tear with or without vitreous prolapse. There can also be occult posterior tears. Sometimes the foreign body can be lodged in the sclera. The sclera is thinnest at the equator; hence occult posterior equatorial injuries are common. The direction of trauma also determines the site of the tear. e.g., the sclera usually gives way at the site of old manual small incision cataracts surgery incision in case of inferior blunt trauma.[37]
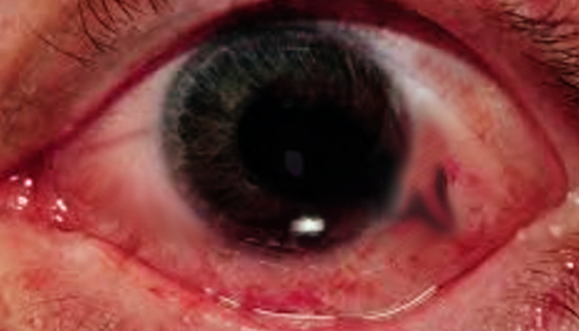
Anterior Chamber Hyphema
- Anterior chamber hyphema - can also result from a blunt trauma from the iris root or ciliary body. The blood settles down at the bottom of the chamber with a particular fluid level. Hyphema can result in raised IOP and manifest as optic neuropathy and corneal endothelial staining.[38]
Hyphema Grading
|
S. No |
Grade |
Anterior chamber volume |
|
1 |
Microhyphema |
Circulating red blood cells |
|
2 |
I |
Less than 33% of anterior chamber volume |
|
3 |
II |
33-50% of anterior chamber volume |
|
4 |
III |
More than 50% of anterior chamber volume |
|
5 |
IV |
Total anterior chamber hyphema (Eightball hyphema) |
- Anterior chamber exudates and fibrinous membrane - can also be seen due to traumatic uveitis. Traumatic glaucoma or angle recession glaucoma can be detected on gonioscopy post blunt trauma. Angle recession is the separation of longitudinal muscle fibers from circular muscle fibers of the ciliary body, resulting in widened ciliary body band and deep anterior chamber.[39]
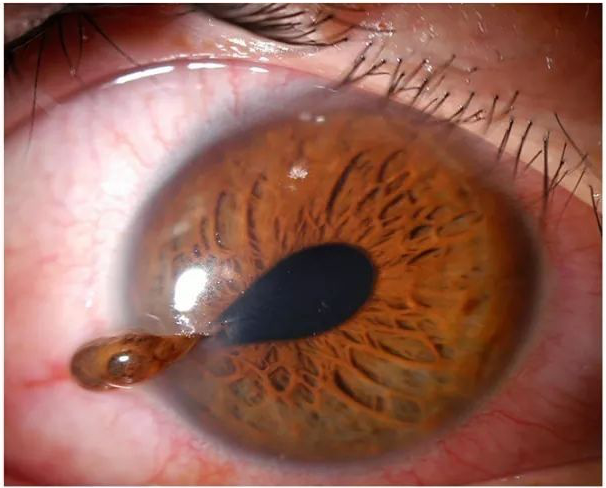
Iris
- Iridodialysis - It is the separation of the iris root from the ciliary body. It is described as D-shaped with a biconvex area adjacent to the limbus best visible on retro illumination. The upper lid masks superior iridodialysis, but iridodialysis in other quadrants caused glare, photophobia, and monocular diplopia. Very rarely, blunt trauma can result in 360-degree iridodialysis with extrusion of the iris through cataract surgery tunnel resulting in aniridia.[40]
- Iris stromal tears - Tears in the iris stromal tissue
Pupil
- Traumatic mydriasis (iridoplegia) - Iridoplegia is due to spasms of the sphincter muscle[41]
- Traumatic miosis - It occurs due to the irritation of ciliary muscles and loss of accommodation[42]
- Pupillary margin rupture - multiple sphincter tears at the pupillary margin
Ciliary Body
- Ciliary body detachment - result in ciliary body shutdown and hypotony.[43]
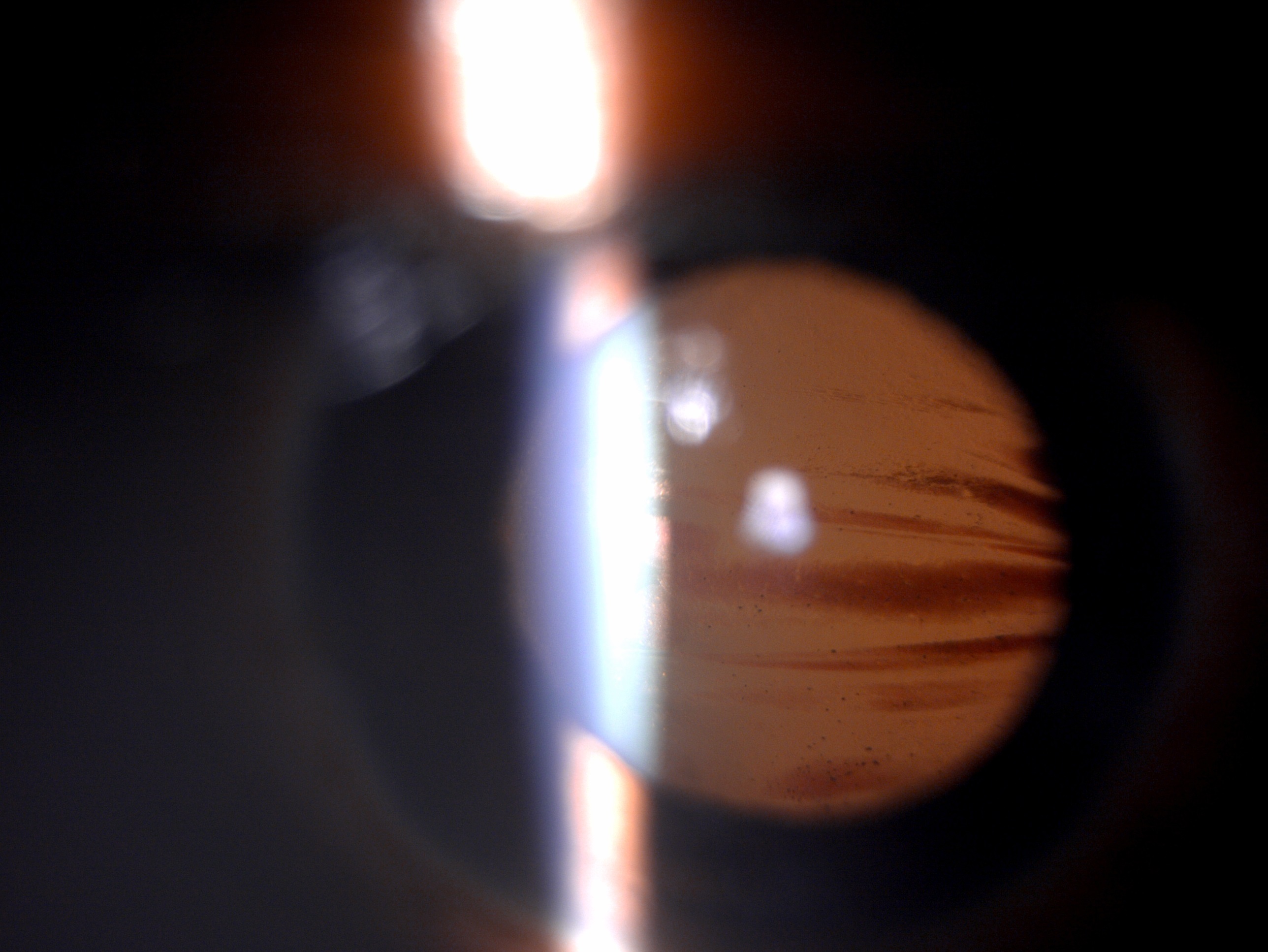
Lens
- Cataract - Traumatic cataracts can result from blunt trauma due to direct damage to the lens and ruptures in the lens capsule leading to an aqueous humour inflow, lenticular fiber hydration, and opacification of lens fibers.[44]
- Vossius ring - Ring-shaped impression of the pupillary margin over the anterior lens capsule due to blunt trauma. The ring is usually smaller than the pupillary diameter.[45]
- Rosette cataract - Blunt trauma can manifest as opacification of posterior subcapsular cortex and sutures, resulting in a flower-shaped cataract.[46]
- Subluxation - Subluxation can result from zonular dialysis or damage to suspensory ligaments. The lens may tilt towards the area of intact zonules. The anterior chamber becomes deep, and the lens may tilt or rotate posteriorly. The lenticular edges and zonules can be seen during dilatation, and there may be iridodonesis and phacodonesis with blinking and ocular movements. If there is gross subluxation, it may result in diplopia and astigmatism from the aphakic portion of the lens.[47]
- Dislocation - When the zonular fibers are damaged completely, they may dislodge the lens in the anterior chamber or the vitreous cavity.[48]
Globe Rupture
Globe rupture can also result after severe blunt trauma. If the visual acuity at presentation is light perception, the prognosis is usually poor. Globe rupture usually occurs adjacent to the angle structures, with prolapse of iris, lens, ciliary body, and vitreous. Anterior globe rupture can be hidden by subconjunctival hemorrhage, and rupture at the site of the old surgical wound like cataract and keratoplasty may result from severe blunt trauma. An occult posterior rupture can be present when the anterior chamber depth is variable. The rupture can be the site of recti muscle insertion, where the scleral is the thinnest.[49]
Posterior Segment Manifestations
Optic Nerve
- Optic nerve avulsion - It is a rare manifestation when a foreign body or object gets impacted between the globe and orbital wall, thus displacing the eye. The mechanism implicated is the rotation or anterior movement of the globe. It can occur as isolated or in association with other orbital trauma. Fundoscopy shows retraction of the optic nerve head from the dural sheath. The visual prognosis is poor in most cases, and there is no treatment.[50]
- Traumatic optic neuropathy - Traumatic optic neuropathy can also result from blunt head or orbital trauma. The patient usually presents with sudden vision loss, and there is RAPD with color vision defect.[51]
Vitreous
- Vitreous hemorrhage - It can be seen in association with posterior vitreous detachment. Pigmentary cells floating in the vitreous, also called tobacco dust, can be noticed. The tobacco dusting may or may not be associated with a retinal tear.[52]]
- Vitreous detachment - It can be anterior or posterior[53]
- Vitreous opacities - Liquefaction of vitreous can occur, and clouds of opacities can be present.[54]
- Vitreous prolapse - Can occur in an anterior chamber associated with subluxated or dislocated cataracts.[55]
Choroid
- Choroidal rupture - Usually temporal to the optic disc and its circular shape. It can be associated with pigmentation at the margins.[56]
- Choroidal hemorrhage - Can be seen under the retina, or the blood may enter the vitreous in case of retinal tear.[57]
- Choroidal detachment - Kissing choroidals are also observable in cases of blunt trauma.[57]
- Traumatic choroiditis - Patches of depigmentation and discoloration can be seen.[58]
Retina
- Berlin's Edema (Commotio Retinae) - It usually presents as a cherry spot at the fovea and results in milky white cloudiness at the posterior pole. Usually, berlin's edema resolves on its own and, in some cases, may manifest as pigmentary changes at the fovea.[59]
- Retinal tear - It occurs in eyes predisposed to retinal tears like myopia, white without pressure, or senile degeneration after blunt trauma.[60]
- Retinal detachment - It may manifest after blunt trauma in the eyes with retinal tears or vitreoretinal traction. Approximately 10% of retinal detachments are secondary to blunt ocular trauma and are more common in young boys. There can be retinal dialysis, giant retinal tear, or equatorial breaks.[60]
- Traumatic Proliferative Retinopathy - It occurs in cases with vitreous hemorrhage.[61]
- Retinal hemorrhage - There can be flame-shaped or boat-shaped. Flame-shaped hemorrhage occurs in cases with blunt trauma.[62]
Macula
- Macular edema - due to concussion injury after blunt trauma[63]
- Pigmentary degeneration - Pigmentary degeneration is usually observed in long-standing cases after blunt eye trauma[64]
- Macular hole - Traumatic macular can be seen after blunt eye trauma[65]
- Macular cyst - Traumatic macular cyst can be also be observed after blunt trauma[66]
- Macular scar - Macular scar can also be seen after blunt eye trauma[67]
Evaluation
Visual Acuity
Visual acuity should be evaluated in each eye separately, if possible, taking care not to manipulate any possible intrinsic globe injury. Pupillary defects should also be noted.[68]
Intraocular Pressure
Intraocular pressure assessment by noncontact tonometry or applanation tonometry is essential in cases of blunt trauma, as secondary glaucoma can result in acute vision loss. Traumatic secondary glaucoma can occur due to blockage, damage, or collapse of the trabecular meshwork, and angle-closure and hypotony can be secondary ciliary body detachment.[69]
Gonioscopy
Gonioscopy is helpful to rule out a foreign body, blood in Schlemm's canal, blood in angles, pigment dispersion, and angle recession. Gonioscopy should be performed under topical anesthesia with 0.5% proparacaine and when the eye is not inflamed. Gonioscopy can be deferred or delayed in case of pain.[69]
Fluorescein Staining
This investigation is essential to locate the epithelial defect, look for abrasions, erosions, and seidel's test.[70]
Seidel's Test
The cornea is stained with fluorescein under topical anesthesia, and the tear site is observed for spontaneous aqueous leak under a cobalt blue filter.[71]
Forced Seidel's Test
The cornea is stained with fluorescein stain under topical anesthesia, and the tear site is observed for an aqueous leak on pressure on the globe under a cobalt blue filter.[71]
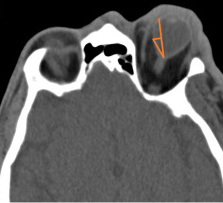
Imaging
X-Ray
A plain X-ray of the skull and orbit is helpful to locate any intraocular foreign body. A metallic foreign can show positional changes due to up and down movement.[72]
B Scan Ultrasonography
This is an essential tool to locate retinal IOFB rule out retinal detachment, globe rupture, vitreous hemorrhage, choroidal detachment, and suprachoroidal hemorrhage. The examining ophthalmologist has to be careful not to exert excess pressure on the globe in case of open globe injuries to prevent extrusion of intraocular contents.[72]
Computed Tomography
Computed tomography (C.T.) imaging can rule out additional maxillofacial injuries while confirming the diagnosis. In addition to globe deformity and retrobulbar hematoma, C.T. imaging can evaluate foreign bodies, scleral disruption, and even vitreous hemorrhage. It is superior to X-ray in locating and detecting IOFBs.[72]
Magnetic Resonance Imaging
Magnetic Resonance Imaging (MRI) is superior in detecting and locating occult posterior rupture and soft tissue trauma. MRI is not indicated in cases of metallic foreign bodies.[72]
Electrodiagnostic Tests
In cases of doubtful visual acuity, electroretinogram (ERG), electrooculography (EOG), visual evoked potential (VEP) are helpful to assess the integrity of the optic nerve and retina.[72]
Optical Coherence Tomography
This investigation is useful to look at the morphology and anatomy of the macula and rule out the macular hole, macular edema, scar, and disruption of IS-OS junction.[72]
A thorough evaluation of any concomitant intracranial and facial bony injury should be pursued. A high number of globe ruptures and retrobulbar hematomas are associated with fractures, particularly the orbital floor. Extraocular motility testing may be decreased in the affected eye because of entrapment, intrinsic globe deformity, or retrobulbar hematoma. Laboratory evaluation should be pursued as the clinical situation dictates in the setting of trauma or anticoagulant use.
Treatment / Management
For globe rupture, emergency department treatment includes supportive measures to prevent worsening of the injury or extrusion of intraocular contents. Hence, antiemetics should be provided to prevent Valsalva from vomiting, leading to increased intraocular pressures and subsequent loss of aqueous fluid. Analgesia should be provided as needed. A rigid eye shield should be placed, and additional manipulation of the eye should be avoided. The patient should be placed in a semi-recumbent position.[73][74][75]
Similarly, in retrobulbar hematoma, analgesia and antiemetic should be provided. Definitive therapy, however, is immediate decompression with a lateral canthotomy and inferior cantholysis. This can be performed by the emergency medicine provider or the ophthalmologist if there are no delays in the consultant performing this procedure. Vision prognosis is time-sensitive in this setting, with poorer outcomes seen in delays of greater than 4 hours from the time of symptoms. Prophylactic antibiotics can be used to prevent secondary endophthalmitis.[14]
In the setting of globe injury or retrobulbar hematoma, emergent consultation with ophthalmology is warranted. Definitive management in these diagnoses is surgical repair by the appropriate ophthalmologic specialist.
Management of Various Manifestations of Blunt Eye Trauma
|
S. No. |
Anatomical Structure |
Pathology |
Medical/ Conservative Management |
Surgical Management |
|
1 |
Conjunctival |
Subconjunctival hemorrhage |
Vitamin C 500 mg B.D. 7 days, observation |
- |
|
|
|
Conjunctival congestion (Conjunctivitis)
|
Topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day based on clinical response |
- |
|
|
|
Foreign body of conjunctiva
|
Superficial- Removal under topical anesthesia, topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day |
Deep- warrants removal in O.T., topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day |
|
|
|
Conjunctival Tear
|
If tenons are intact, topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day |
If there is a breach in tenons and irregular Tear- Conjunctival tear suturing with 8-0 vicryl sutures in O.T., topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day |
|
2 |
Cornea |
Epithelial damage |
Topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day, Non-resolving cases- bandage contact lens |
Non-resolving cases, amniotic membrane graft, topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day |
|
|
|
Corneal edema |
Antiglaucoma medication 0.5% timolol B.D. for 1-2 weeks if intraocular pressure is high |
|
|
|
|
Descemet Membrane tear |
Localized -Observation |
Large DMD involving visual axis- Air descematopexy |
|
|
|
Recurrent corneal erosions |
Topical 0.5% moxifloxacin 4-6 times per days 0.5% carboxymethylcellulose 4-6 times per day, BCL |
Anterior stromal puncture, Superficial keratectomy |
|
|
|
Corneal Tear |
Self-sealed tear without infiltrating, observation with topical antibiotics, with infiltrate- Topical antibiotics or antifungals based on infiltrate characteristics |
Seidel's positive- Corneal Tear suturing with 9-0 0r 10-0 nylon sutures |
|
3 |
Sclera |
Scleral Tear |
Topical steroids and lubricants |
Scleral Tear suturing with 10-0 nylon in OT |
|
|
|
IOFB |
Topical steroids and lubricants |
IOFB removal and Scleral tear suturing with 10-0 nylon in O.T. with or without surface vitrectomy |
|
4 |
Anterior chamber |
Hyphema |
Topical steroids, antiglaucoma medications, cycloplegics, and lubricants
|
Non-resolving cases or more than 50% hyphema or raised intraocular pressure- anterior chamber wash |
|
|
|
Anterior chamber exudates and fibrinous membrane |
Topical antibiotics and antifungals for exudates based on clinical characteristics and topical steroids, cycloplegics, and lubricants for fibrinous membrane |
Anterior chamber wash, Intracameral antibiotics, or antifungals |
|
5 |
Iris |
Iridodialysis |
Bed rest, topical antiglaucoma drugs, oral acetazolamide (avoided in patients with sickle cell disease); avoid aspirin, heparin,/warfarin |
Associated large hyphema – anterior chamber wash. Surgical repair using 10-0 prolene sutures |
|
6 |
Pupil |
Traumatic mydriasis (iridoplegia) |
Opaque contact lenses or sunglasses |
Persistent symptoms – surgical repair |
|
|
|
Traumatic miosis |
Observation, short term cycloplegics |
|
|
|
|
Pupillary margin rupture
|
Observation for localized sphincter tear, accommodation difficulty/excessive glare - opaque contact lenses or sunglasses |
Persistent symptoms affecting daily routine activities- surgical repair |
|
7 |
Ciliary body |
Ciliary body detachment |
Cycloplegics, topical or systemic steroids, laser photocoagulation of ciliary body |
|
|
8 |
Lens |
Cataract/ Rosette cataract |
Observation if visually insignificant. Refractive correction should be tried. |
Visually significant – cataract extraction with IOL as a primary or secondary procedure |
|
|
|
Vossius ring |
Observation |
Associated cataract - cataract extraction with IOL as a primary or secondary procedure |
|
|
|
Subluxation |
Observation or refractive correction |
<5 clock hours – CTR with IOL, 5-7 clock hours – CTR +CTS or Cionni with IOL 7-9 clock hours – Cionni with 2 eyelets or Cionni with 1 eyelet + CTS + IOL >9 clock hours – cataract extraction +SFIOL |
|
|
|
Dislocation |
- |
Anterior – sclerocorneal lens extraction + secondary IOL implantation. Posterior - Pars plana vitrectomy + lens removal + secondary IOL implantation |
|
9 |
Globe |
Globe Rupture
|
Topical preservative-free antibiotics hourly, plus systemic antibiotics. An eye shield or other protective device |
Surgical repair based on location and extent of the injury |
|
10 |
Optic nerve |
Optic Nerve Avulsion
|
- |
- |
|
|
|
Traumatic Optic Neuropathy
|
ONTT protocol- Systemic corticosteroids |
Optic nerve decompression |
|
11 |
Vitreous |
Vitreous hemorrhage
|
Observation, head elevation |
Non-resolving and vision-threatening – pars plana vitrectomy |
|
|
|
Vitreous detachment |
Observation |
Associated |
|
|
|
Vitreous opacities |
Observation |
If vision-threatening needs pars plana vitrectomy |
|
|
|
Vitreous prolapse |
Minimal vitreous in AC- Observation |
Vitreous blob, vitreous in the tunnel- needs anterior vitrectomy |
|
12 |
Choroid |
Choroidal rupture |
Observation |
Observation |
|
|
|
Choroidal hemorrhage |
Observation |
If vision-threatening- pars plana vitrectomy |
|
|
|
Choroidal detachment |
Observation |
Non-resolving serous or hemorrhagic choroidal detachment will need scleral drainage |
|
|
|
Traumatic choroiditis |
Steroids with lubricants |
- |
|
13 |
Retina |
Berlin's Edema (Commotio Retinae) |
Observation |
- |
|
|
|
Retinal Tear |
Laser photocoagulation |
Cryopexy or Pars plana vitrectomy with Endolaser |
|
|
|
Retinal detachment |
- |
Cryopexy or Pars plana vitrectomy with Endolaser, Silicon oil tamponade |
|
|
|
Traumatic Proliferative Retinopathy |
- |
Pars plana vitrectomy with PVR release |
|
|
|
Retinal hemorrhage |
Observation |
If vision-threatening- pars plana vitrectomy |
|
14 |
Macula |
Macular edema |
Topical steroids + NSAID's
|
Intravitreal anti-VEGF, Steroids |
|
|
|
Pigmentary degeneration |
Observation |
Observation |
|
|
|
Macular hole |
Early-stage 1- wait for spontaneous closure |
Large macular hole- Pars plana vitrectomy and ERM peeling |
|
|
|
Macular cyst |
Observation |
If vision-threatening- cyst excision |
|
|
|
Macular scar |
Observation |
Observation |
Differential Diagnosis
The differential diagnosis of blunt trauma to the eye includes
- Globe rupture
- Retrobulbar hematoma
- Traumatic glaucoma
- Hyphema
- Orbital blowout fracture with entrapment
- Foreign body
- Scleral disruption
- Vitreous hemorrhage
Prognosis
The prognosis of blunt eye trauma depends heavily on the sequela of the trauma. One study showed that ocular trauma, in general, resulted in monocular blindness in one-quarter of patients.[76] In kids, research has shown that visual acuity is generally better in blunt ocular injury compared to penetrating ocular injury, although rates of glaucoma may be higher in blunt ocular trauma.[77] However, if the eye is ruptured, blunt ocular trauma may lead to the worst visual prognosis since that most likely means the trauma occurred at a high velocity. Other factors that may lead to a worse visual prognosis include a relative afferent pupillary defect, absence of a red reflex, initial visual acuity worse than 20/200, and an eyelid laceration.[78] In another study, in patients with commotio retinae or sclopetaria retinae from blunt ocular trauma, a quarter of patients had visual acuity worse than 20/30 in the eye that had the trauma.[79] Visual acuity is worse after blunt ocular trauma if there is a hyphema, retinal detachment, and/or vitreous hemorrhage.[37] Traumatic optic neuropathy also portends a poor visual outcome.[80]
The extent of the initial injury and the injury mechanism often predict whether poor outcomes might be expected. To give the best prognosis of an individual's visual prognosis, the Ocular Trauma Score is a verified method to predict the functional outcome of an eye after trauma.[81]
Complications
Depending on the type and extent of the trauma to the eye, complications may vary based on the location and depth of injury.
- Conjunctival Tear
- Corneal Tear
- Corneal infiltrates
- Corneal scarring
- Hyphema
- Hypopyon
- Anterior chamber exudates
- Fibrinous membrane
- Iridodialysis
- Iris prolapse
- Traumatic Mydriasis
- Iridoplegia
- Angle-closure glaucoma
- Post-traumatic glaucoma
- Subluxated lens
- Dislocated lens
- Subluxated IOL
- Dislocated IOL
- Posterior capsular rupture
- Zonular dialysis
- Cataracts
- Retinal Tear
- Retinal detachment
- Choroidal detachment
- Choroidal rupture
- Traumatic optic neuropathy
- Optic nerve avulsion
- Endophthalmitis
- Panophthalmitis
Varying degrees of vision loss may also occur. Enucleation may be required in severe trauma not amenable to ophthalmologic surgical repair.
Postoperative and Rehabilitation Care
Based on the indication, all patients undergoing surgical intervention should be managed with post-operative medication (antibiotics, antifungals, steroids, or oral anti-inflammatory, antibiotics). The patient should be closely followed up to prevent any significant complications.[82]
Consultations
All cases of blunt eye trauma presenting to the clinic or casualty should be evaluated in detail by the ophthalmologist. Patients requiring surgical intervention or expert opinion should be referred to corneal, external disease, trauma specialist, and a retina specialist for targeted management and good visual outcome. Non-resolving glaucoma cases will need expert inputs from glaucoma surgeons. Patients with traumatic cataract subluxated or dislocated nucleus should be managed by a cataract and IOL surgeon.[2]
Deterrence and Patient Education
Patients should be educated on the importance of wearing eye protection when doing any activity where ocular trauma commonly occurs. This includes sports and riding motorized vehicles, among many other things. Eye protection has been found to reduce severe ocular injuries in combat operations.[83] Patients should be encouraged to wear ocular protection at all times if they are monocular due to trauma to the eye with vision potentially leading to blindness. Many cases of ocular trauma occur within the home, so consideration should be made to educating patients on ocular protection at all times, and not just traditional high-risk activities such as sports.[84]
Pearls and Other Issues
- Avoid any unnecessary manipulation of the globe (including tonometry) to prevent any extrusion of intraocular contents.
- Obtain appropriate imaging to rule out concomitant bony injury or intracranial trauma.
- Provide analgesia and antiemetics to prevent Valsalva maneuvers that may worsen globe rupture or retrobulbar hematoma.
- A protective rigid eye shield should be utilized to prevent any additional injury; eye patches are contraindicated.
- Provide prophylactic antibiotics to help prevent endophthalmitis.
- Seek emergent Ophthalmology consultation for definitive measures, but do not delay lateral canthotomy for patients with known retrobulbar hematoma.
Enhancing Healthcare Team Outcomes
Eye trauma is prevalent, resulting in loss of vision in many people. Without vision, one becomes handicapped, and getting a suitable job is difficult. In many cases, ocular eye injury is preventable, and the onus is on all clinicians to educate patients on eye safety. An interprofessional team is probably the best way to educate and monitor patients with eye trauma. Because of a serious shortage of eye surgeons, most patients are followed up by the primary care provider or nurse practitioner as outpatients.
Eye trauma commonly presents to the emergency department. However, in the ED, besides a superficial exam including a visual acuity test, analysis of deeper injury to the eye is not always possible. Hence, healthcare workers, including nurse practitioners, should always consult with the ophthalmologist on call to assess the eye.
The emergency department physician may treat superficial lacerations around the eye, but all patients with vision loss should be referred to the ophthalmologist. During follow-up, the nurse practitioner and primary care provider should communicate with the eye surgeon if there are any vision-related problems.
Missing eye injuries can lead to permanent visual loss and may include prolonged litigation.
Finally, all clinicians should educate patients on eye safety, such as wearing face helmets and safety goggles when working with splashing liquids or flying debris.[85] [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Scott R. The injured eye. Philosophical transactions of the Royal Society of London. Series B, Biological sciences. 2011 Jan 27:366(1562):251-60. doi: 10.1098/rstb.2010.0234. Epub [PubMed PMID: 21149360]
Mutie D, Mwangi N. Assessing an eye injury patient. Community eye health. 2015:28(91):46-8 [PubMed PMID: 26989310]
Al-Thowaibi A,Kumar M,Al-Matani I, An overview of penetrating ocular trauma with retained intraocular foreign body. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2011 Apr [PubMed PMID: 23960924]
Level 3 (low-level) evidenceRajsic S,Breitkopf R,Bachler M,Treml B, Diagnostic Modalities in Critical Care: Point-of-Care Approach. Diagnostics (Basel, Switzerland). 2021 Nov 25; [PubMed PMID: 34943438]
Jung HC,Lee SY,Yoon CK,Park UC,Heo JW,Lee EK, Intraocular Foreign Body: Diagnostic Protocols and Treatment Strategies in Ocular Trauma Patients. Journal of clinical medicine. 2021 Apr 25 [PubMed PMID: 33923011]
Kumar K, Figurasin R, Kumar S, Waseem M. An Uncommon Meridional Globe Rupture due to Blunt Eye Trauma. Case reports in emergency medicine. 2018:2018():1808509. doi: 10.1155/2018/1808509. Epub 2018 Sep 18 [PubMed PMID: 30319823]
Level 3 (low-level) evidenceKurien NA,Peter J,Jacob P, Spectrum of Ocular Injuries and Visual Outcome Following Firework Injury to the Eye. Journal of emergencies, trauma, and shock. 2020 Jan-Mar [PubMed PMID: 32395048]
Scheufele TA,Blomquist PH, spectrum of ocular trauma at an urban county hospital. Texas medicine. 2004 Dec [PubMed PMID: 15685908]
Ababneh LT, Mohidat H, Abdelnabi H, Kana'an MF, Tashtush NA, El-Mulki OS, Aleshawi AJ. Hospital-Based Ocular Trauma: Factors, Treatment, And Impact Outcome. Clinical ophthalmology (Auckland, N.Z.). 2019:13():2119-2126. doi: 10.2147/OPTH.S223379. Epub 2019 Oct 31 [PubMed PMID: 31802841]
Haavisto AK,Sahraravand A,Puska P,Leivo T, Toy gun eye injuries - eye protection needed Helsinki ocular trauma study. Acta ophthalmologica. 2018 Nov 2 [PubMed PMID: 30390370]
Jolly R,Arjunan M,Theodorou M,Dahlmann-Noor AH, Eye injuries in children - incidence and outcomes: An observational study at a dedicated children's eye casualty. European journal of ophthalmology. 2019 Sep [PubMed PMID: 30270661]
Level 2 (mid-level) evidenceSen E,Celik S,Inanc M,Elgin U,Ozyurt B,Yılmazbas P, Seasonal distribution of ocular conditions treated at the emergency room: a 1-year prospective study. Arquivos brasileiros de oftalmologia. 2018 Apr [PubMed PMID: 29846426]
Puodžiuvienė E,Jokūbauskienė G,Vieversytė M,Asselineau K, A five-year retrospective study of the epidemiological characteristics and visual outcomes of pediatric ocular trauma. BMC ophthalmology. 2018 Jan 18 [PubMed PMID: 29347941]
Level 2 (mid-level) evidenceKumar S,Blace N, Retrobulbar Hematoma StatPearls. 2022 Jan [PubMed PMID: 35015442]
Vingopoulos F,Wang Y,Grob S,Li CYL,Eliott D,Kim LA,Vavvas DG,Miller JB, Open Globe Injury with Intraocular Foreign Body. Journal of vitreoretinal diseases. 2021 Jul 1; [PubMed PMID: 34386688]
Maurya RP,Srivastav T,Singh VP,Mishra CP,Al-Mujaini A, The epidemiology of ocular trauma in Northern India: A teaching hospital study. Oman journal of ophthalmology. 2019 May-Aug [PubMed PMID: 31198291]
Keel S,Xie J,Foreman J,Taylor HR,Dirani M, The prevalence of vision loss due to ocular trauma in the Australian National Eye Health Survey. Injury. 2017 Nov [PubMed PMID: 28964509]
Level 3 (low-level) evidenceNégrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic epidemiology. 1998 Sep:5(3):143-69 [PubMed PMID: 9805347]
Aghadoost D. Ocular trauma: an overview. Archives of trauma research. 2014 Jun:3(2):e21639. doi: 10.5812/atr.21639. Epub 2014 Jun 29 [PubMed PMID: 25147781]
Level 3 (low-level) evidenceBi H,Cui Y,Li Y,Wang X,Zhang J, Clinical characteristics and surgical problems of ruptured globe injury. Current therapeutic research, clinical and experimental. 2013 Jun; [PubMed PMID: 24385006]
Kopecky A,Rokohl AC,Nemcansky J,Koch KR,Matousek P,Heindl LM, [Retrobulbar Haematoma - a Complication that May Impair Vision]. Klinische Monatsblatter fur Augenheilkunde. 2021 May [PubMed PMID: 31416097]
Wangsathaporn K,Tsui I, Commotio Retinae Resulting From Rubber Band Injury in Two Girls. Ophthalmic surgery, lasers & imaging retina. 2019 May 1 [PubMed PMID: 31100162]
Lucke-Wold BP,Phillips M,Turner RC,Logsdon AF,Smith KE,Huber JD,Rosen CL,Regele JD, Elucidating the role of compression waves and impact duration for generating mild traumatic brain injury in rats. Brain injury. 2017; [PubMed PMID: 27880054]
Burstein ES,Lazzaro DR, Traumatic ruptured globe eye injuries in a large urban center. Clinical ophthalmology (Auckland, N.Z.). 2013 [PubMed PMID: 23493627]
Level 3 (low-level) evidenceFriehmann A,Peled A,Ela-Dalman N,Nemet AY, Isolated Superior Rectus Muscle Hematoma Following Blunt Orbital Trauma. The Journal of craniofacial surgery. 2019 Mar/Apr [PubMed PMID: 30531284]
Vukovic AA,Poole MD,Hoehn EF,Caldwell AK,Schondelmeyer AC, Things Are Not Always What They Seem: Two Cases of Child Maltreatment Presenting With Common Pediatric Chief Complaints. Pediatric emergency care. 2019 Jun [PubMed PMID: 30489490]
Level 3 (low-level) evidenceCourt JH,Lu LM,Wang N,McGhee CNJ, Visual and ocular morbidity in severe open-globe injuries presenting to a regional eye centre in New Zealand. Clinical & experimental ophthalmology. 2019 May [PubMed PMID: 30414237]
Doshi R,Noohani T, Subconjunctival Hemorrhage 2020 Jan; [PubMed PMID: 31869130]
Vaidyanathan U, Hopping GC, Liu HY, Somani AN, Ronquillo YC, Hoopes PC, Moshirfar M. Persistent Corneal Epithelial Defects: A Review Article. Medical hypothesis, discovery & innovation ophthalmology journal. 2019 Fall:8(3):163-176 [PubMed PMID: 31598519]
Costagliola C,Romano V,Forbice E,Angi M,Pascotto A,Boccia T,Semeraro F, Corneal oedema and its medical treatment. Clinical & experimental optometry. 2013 Nov [PubMed PMID: 23679934]
Chow VW,Agarwal T,Vajpayee RB,Jhanji V, Update on diagnosis and management of Descemet's membrane detachment. Current opinion in ophthalmology. 2013 Jul; [PubMed PMID: 23665525]
Level 3 (low-level) evidenceMiller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clinical ophthalmology (Auckland, N.Z.). 2019:13():325-335. doi: 10.2147/OPTH.S157430. Epub 2019 Feb 11 [PubMed PMID: 30809089]
Barot RK,Karkhanis A,Shitole SC, An Unusual Traumatic Lamellar Laceration of Cornea. Journal of clinical and diagnostic research : JCDR. 2015 Jun; [PubMed PMID: 26266144]
Krauthammer M,Mandelblum J,Spierer O, Corneal Blood Staining after Complicated Cataract Surgery. Case reports in ophthalmology. 2018 Sep-Dec [PubMed PMID: 30323760]
Level 3 (low-level) evidenceWilson SL,El Haj AJ,Yang Y, Control of scar tissue formation in the cornea: strategies in clinical and corneal tissue engineering. Journal of functional biomaterials. 2012 Sep 18 [PubMed PMID: 24955637]
Jansen ME,Situ P,Begley CG,Boree D,Chalmers RL,Osborn Lorenz K,Wilson T, Characterizing Contact Lens-Related Corneal Infiltrates: A Pilot Study. Cornea. 2016 Dec; [PubMed PMID: 27560033]
Level 3 (low-level) evidence, , , [PubMed PMID: 27589050]
Walton W, Von Hagen S, Grigorian R, Zarbin M. Management of traumatic hyphema. Survey of ophthalmology. 2002 Jul-Aug:47(4):297-334 [PubMed PMID: 12161209]
Level 3 (low-level) evidenceAgrawal RV, Murthy S, Sangwan V, Biswas J. Current approach in diagnosis and management of anterior uveitis. Indian journal of ophthalmology. 2010 Jan-Feb:58(1):11-9. doi: 10.4103/0301-4738.58468. Epub [PubMed PMID: 20029142]
Balamurugan R,Gupta PC,Sharma VK,Khurana S,Ram J, Alternate iris bypass technique of iridodialysis repair. Indian journal of ophthalmology. 2020 Jun [PubMed PMID: 32461449]
Mikropoulos DG,Kymionis GD,Grentzelos MA,Voulgari N,Katsanos A,Konstas AG, Combined Pupilloplasty and Retropupillary Iris-Claw Intraocular Lens Implantation with DSAEK in a Patient with Traumatic Iridoplegia, Aphakia and Corneal Decompensation. Ophthalmology and therapy. 2019 Sep [PubMed PMID: 31317508]
Impallomeni M, Transient complete ptosis and miosis following trauma to the right eyeball in a rugby injury: where was the lesion? Journal of the Royal Society of Medicine. 1997 Nov [PubMed PMID: 9496277]
Level 3 (low-level) evidenceColeman DJ, Evaluation of ciliary body detachment in hypotony. Retina (Philadelphia, Pa.). 1995; [PubMed PMID: 8545577]
Gupta VB,Rajagopala M,Ravishankar B, Etiopathogenesis of cataract: an appraisal. Indian journal of ophthalmology. 2014 Feb; [PubMed PMID: 24618482]
Williams JC,Chambers JP,Liehr JG, Glutamyl ribose 5-phosphate storage disease. A hereditary defect in the degradation of poly(ADP-ribosylated) proteins. The Journal of biological chemistry. 1984 Jan 25 [PubMed PMID: 6693374]
Singh RB,Thakur S,Ichhpujani P, Traumatic rosette cataract. BMJ case reports. 2018 Nov 28 [PubMed PMID: 30567140]
Level 3 (low-level) evidencePraveen MR,Vasavada AR,Singh R, Phacoemulsification in subluxated cataract. Indian journal of ophthalmology. 2003 Jun [PubMed PMID: 12831145]
Level 2 (mid-level) evidenceMönestam EI, Incidence of dislocation of intraocular lenses and pseudophakodonesis 10 years after cataract surgery. Ophthalmology. 2009 Dec; [PubMed PMID: 19815277]
Level 2 (mid-level) evidenceChen X,Yao Y,Wang F,Liu T,Zhao X, A retrospective study of eyeball rupture in patients with or without orbital fracture. Medicine. 2017 Jun; [PubMed PMID: 28614230]
Level 2 (mid-level) evidenceMackiewicz J,Tomaszewska J,Jasielska M, Optic nerve avulsion after blunt ocular trauma - Case report. Annals of agricultural and environmental medicine : AAEM. 2016 Jun 2 [PubMed PMID: 27294653]
Level 3 (low-level) evidenceYu-Wai-Man P, Traumatic optic neuropathy-Clinical features and management issues. Taiwan journal of ophthalmology. 2015 Mar 1 [PubMed PMID: 26052483]
Spraul CW, Grossniklaus HE. Vitreous Hemorrhage. Survey of ophthalmology. 1997 Jul-Aug:42(1):3-39 [PubMed PMID: 9265701]
Level 3 (low-level) evidenceJohnson MW. Perifoveal vitreous detachment and its macular complications. Transactions of the American Ophthalmological Society. 2005:103():537-67 [PubMed PMID: 17057817]
Level 2 (mid-level) evidenceIvanova T,Jalil A,Antoniou Y,Bishop PN,Vallejo-Garcia JL,Patton N, Vitrectomy for primary symptomatic vitreous opacities: an evidence-based review. Eye (London, England). 2016 May; [PubMed PMID: 26939559]
Kim TY,Kang HG,Kim CY,Koh HJ,Kim SS,Kim M, Delayed vitreous prolapse after cataract surgery: clinical features and surgical outcomes. Scientific reports. 2021 Aug 9 [PubMed PMID: 34373536]
Moon K,Kim KS,Kim YC, A case of expansion of traumatic choroidal rupture with delayed-developed outer retinal changes. Case reports in ophthalmology. 2013 [PubMed PMID: 24019789]
Level 3 (low-level) evidenceKuhn F,Morris R,Mester V, Choroidal detachment and expulsive choroidal hemorrhage. Ophthalmology clinics of North America. 2001 Dec [PubMed PMID: 11787743]
Ludwig CA,Shields RA,Do DV,Moshfeghi DM,Mahajan VB, Traumatic chorioretinitis sclopetaria: Risk factors, management, and prognosis. American journal of ophthalmology case reports. 2019 Jun [PubMed PMID: 30834355]
Level 3 (low-level) evidencePark JY,Nam WH,Kim SH,Jang SY,Ohn YH,Park TK, Evaluation of the central macula in commotio retinae not associated with other types of traumatic retinopathy. Korean journal of ophthalmology : KJO. 2011 Aug [PubMed PMID: 21860574]
Level 2 (mid-level) evidenceKwok JM,Yu CW,Christakis PG, Retinal detachment. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2020 Mar 23 [PubMed PMID: 32392514]
Idrees S, Sridhar J, Kuriyan AE. Proliferative Vitreoretinopathy: A Review. International ophthalmology clinics. 2019 Winter:59(1):221-240. doi: 10.1097/IIO.0000000000000258. Epub [PubMed PMID: 30585928]
Kaur B, Taylor D. Retinal haemorrhages. Archives of disease in childhood. 1990 Dec:65(12):1369-72 [PubMed PMID: 2103739]
Tranos PG, Wickremasinghe SS, Stangos NT, Topouzis F, Tsinopoulos I, Pavesio CE. Macular edema. Survey of ophthalmology. 2004 Sep-Oct:49(5):470-90 [PubMed PMID: 15325193]
Level 3 (low-level) evidenceBae K,Cho K,Kang SW,Kim SJ,Kim JM, Peripheral Reticular Pigmentary Degeneration and Choroidal Vascular Insufficiency, Studied by Ultra Wide-Field Fluorescein Angiography. PloS one. 2017 [PubMed PMID: 28114409]
Bikbova G,Oshitari T,Baba T,Yamamoto S,Mori K, Pathogenesis and Management of Macular Hole: Review of Current Advances. Journal of ophthalmology. 2019 [PubMed PMID: 31191994]
Level 3 (low-level) evidenceYalçın NG,Özdek Ş, The Relationship Between Macular Cyst Formation and Ischemia in Diabetic Macular Edema Turkish journal of ophthalmology. 2019 Sep 3; [PubMed PMID: 31486606]
Kolomeyer AM,Szirth BC,Nayak NV,Khouri AS, Complimentary imaging technologies in blunt ocular trauma. Oman journal of ophthalmology. 2013 May [PubMed PMID: 24082670]
Level 3 (low-level) evidenceKim JJ,Moon JH,Jeong HS,Chi M, Has decreased visual acuity associated with blunt trauma at the emergency department recovered? The Journal of craniofacial surgery. 2012 May [PubMed PMID: 22565865]
Ding C, Zeng J. Clinical study on Hypotony following blunt ocular trauma. International journal of ophthalmology. 2012:5(6):771-3. doi: 10.3980/j.issn.2222-3959.2012.06.21. Epub 2012 Dec 18 [PubMed PMID: 23275915]
. Assessing and managing eye injuries. Community eye health. 2005 Oct:18(55):101-4 [PubMed PMID: 17491766]
Campbell TD, Gnugnoli DM. Seidel Test. StatPearls. 2025 Jan:(): [PubMed PMID: 31082063]
Lin KY, Ngai P, Echegoyen JC, Tao JP. Imaging in orbital trauma. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2012 Oct:26(4):427-32. doi: 10.1016/j.sjopt.2012.08.002. Epub [PubMed PMID: 23961028]
Nemet AY,Asalee L,Lang Y,Briscoe D,Assia EI, Ocular Paintball Injuries. The Israel Medical Association journal : IMAJ. 2016 Jan [PubMed PMID: 26964276]
Hoskin AK,Yardley AM,Hanman K,Lam G,Mackey DA, Sports-related eye and adnexal injuries in the Western Australian paediatric population. Acta ophthalmologica. 2016 Sep [PubMed PMID: 26647756]
Gelston CD, Common eye emergencies. American family physician. 2013 Oct 15 [PubMed PMID: 24364572]
Zungu T,Mdala S,Manda C,Twabi HS,Kayange P, Characteristics and visual outcome of ocular trauma patients at Queen Elizabeth Central Hospital in Malawi. PloS one. 2021 [PubMed PMID: 33780448]
Ram J,Verma N,Gupta N,Chaudhary M, Effect of penetrating and blunt ocular trauma on the outcome of traumatic cataract in children in northern India. The journal of trauma and acute care surgery. 2012 Sep [PubMed PMID: 22929502]
Level 2 (mid-level) evidenceRahman I,Maino A,Devadason D,Leatherbarrow B, Open globe injuries: factors predictive of poor outcome. Eye (London, England). 2006 Dec [PubMed PMID: 16179934]
Level 2 (mid-level) evidenceQuality assurance in dentistry: executive summary, part 1. ADA Quality Assurance Project., Stern SK,Morrissey SC,Mauldin J,, Journal of the American Dental Association (1939), 1979 Jan [PubMed PMID: 23618228]
Level 2 (mid-level) evidenceKuhn F,Maisiak R,Mann L,Mester V,Morris R,Witherspoon CD, The Ocular Trauma Score (OTS). Ophthalmology clinics of North America. 2002 Jun [PubMed PMID: 12229231]
Irawati Y,Soedarman S,Arianti A,Widyasari A,Reksodiputro MH, Multiple Approaches for Managing Complex Ophthalmic Blunt Trauma: A Case Report. International medical case reports journal. 2021 [PubMed PMID: 33833590]
Level 3 (low-level) evidenceThomas R,McManus JG,Johnson A,Mayer P,Wade C,Holcomb JB, Ocular injury reduction from ocular protection use in current combat operations. The Journal of trauma. 2009 Apr [PubMed PMID: 19359977]
Level 2 (mid-level) evidenceDesai P,MacEwen CJ,Baines P,Minassian DC, Incidence of cases of ocular trauma admitted to hospital and incidence of blinding outcome. The British journal of ophthalmology. 1996 Jul [PubMed PMID: 8795369]
Level 3 (low-level) evidencePeate WF, Work-related eye injuries and illnesses. American family physician. 2007 Apr 1 [PubMed PMID: 17427615]