Introduction
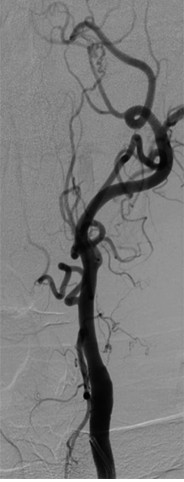
Acute arterial occlusion is synonymous with acute limb ischemia and is considered a vascular emergency (see Image. Occlusion of the Internal Carotid Artery). Acute limb ischemia is a sudden loss of limb perfusion for up to 2 weeks after the initiating event. Acute arterial occlusion can occur in any upper and lower extremities peripheral artery. Acute occlusion can lead to a limb or life-threatening ischemia. Diagnostic measures, treatment, and management depend on the affected artery and the patient's medical history. Acute arterial occlusion is time-sensitive and, left untreated, can quickly progress to infarction and loss of limb and life. Acute arterial occlusion is associated with increased morbidity, significant disability, and emergent operation in high-risk patients.[1][2][3] A patient with acute arterial occlusion will generally present pain in the involved muscle group, aggravated by exertion. This phenomenon is called intermittent claudication when a patient feels pain in the involved limb while walking.[4] The most typical area of arterial occlusion is the distal superficial femoral artery, resulting in claudication in the calf muscle area.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The most common cause of acute limb ischemia is in situ thrombotic occlusion. It is more common in the lower extremities, and the initiating event is a preexisting history of peripheral artery disease (PAD). Thrombotic occlusions can occur in an upper and lower extremities segment but most commonly affect the superficial femoral artery. Patients with a preexisting PAD history tend to have the well-established development of collateral vessels, creating variability in symptoms and severity. Other causes include embolic occlusion from the left heart, aorta, and iliac vessels and penetrating or blunt trauma.[5]
Epidemiology
Published studies regarding the true incidence of acute limb ischemia are lacking. However, in a prospective population-based study in Oxford, England, over a 10-year time frame, the incidence of critical limb ischemia was determined to be 22 per 100,000 per year. Acute limb ischemia affects older men and women equally, with a median age of 75. Risk factors include age, smoking, diabetes, obesity, sedentary lifestyle, family history of vascular disease, high cholesterol, and high blood pressure. Non-traumatic ischemia of the lower extremities is more common than the upper extremities and is more likely to result in limb loss. Atherosclerosis affects around 10% of the Western population over 65 years. With the number of older people expected to increase by 22% by 2040, atherosclerosis will become a huge financial concern in medicine. The estimated PAD prevalence in the general US population was 4.3%, which means in 2000, around 5 million people in the US had PAD. That number rises with age; therefore, the increasing older population means more people are affected by PAD.[6]
Pathophysiology
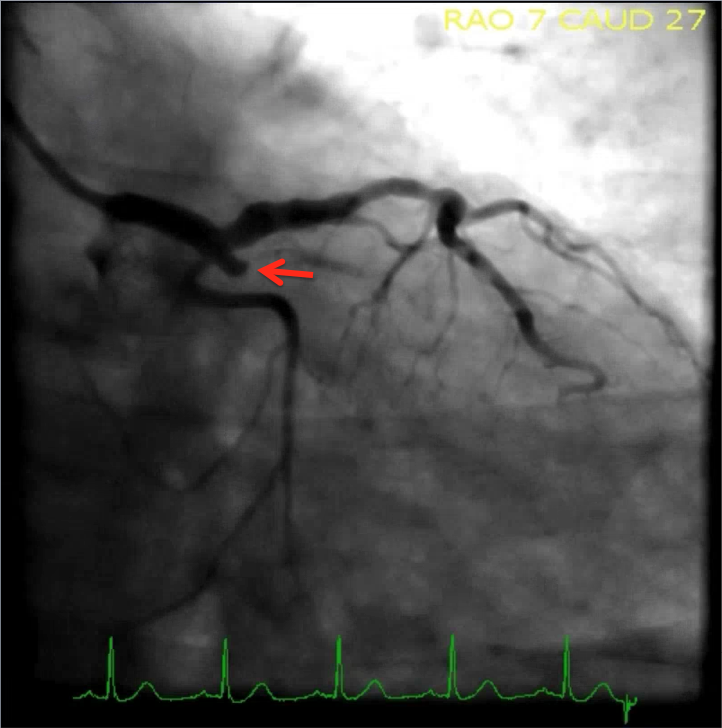
In situ thrombosis most commonly affects the femoral or popliteal arteries, while emboli most widely lodge in aortic, iliac, femoral, and popliteal bifurcations. Once arterial blood flow is impeded, under-perfused tissues switch to anaerobic metabolism, producing lactate, causing acidosis and increasing free radicals (see Image. One Hundred Percent Proximal Circumflex Artery Occlusion, TIMI flow 0). Prolonged and untreated, this state will cause the hypoxic muscle to run out of its ATP stores. This is followed by impaired calcium/sodium pump and sodium/potassium-ATPase functioning, leading to intracellular calcium leakage into the myocytes. Increasing free calcium negatively interacts with the muscle's myosin, actin, and proteases and eventually causes muscle fiber necrosis. In addition, intracellular potassium, phosphate, creatine kinase, and myoglobin are released into the systemic circulation due to the necrotic muscle.
Under resting circumstances, normal blood flow to peripheral muscle groups averages around 300 to 400 mL/min.[7] Once a person starts exercising, blood flow increases in active muscle groups as much as 10-fold due to the rise in compensatory vasodilation and cardiac output at the tissue level. This leads to an increase in oxygen demand. When exercise stops, blood flow returns to baseline within minutes. An atherosclerotic blood vessel leads to stenosis, which can cause occlusion at some point. In atherosclerosis, each stenotic segment reduces the pressure on the head experienced by peripheral muscle groups. Subsequently, at rest, the blood pressure at the ankle is lower than that measured in a healthy individual. This reduction in blood pressure becomes more significant once physical activity starts, leading to a greatly diminished distal blood pressure. Homocysteine is also an underlying factor that causes atherosclerosis, which leads to occlusion and ischemia.[8]
History and Physical
The classic presentation of acute arterial occlusion involves the "6 Ps": pallor, pain, paresthesia, paralysis, pulselessness, and poikilothermia.[9] These clinical manifestations can occur anywhere distal to the occlusion. Most patients initially present with pain, pallor, pulselessness, and poikilothermia. Pain is often localized and less severe when the limb is dependent. As the ischemia prolongs, paresthesia replaces pain, and the final stages of injury cause paralysis. Patients with embolic occlusion tend to have an abrupt onset with more severe symptoms, as collateralization of the vasculature has not occurred at this point. It is essential to realize that symptoms can develop for hours to days and present as new or recurring. Low kidney function has been linked with the development of arterial occlusive disease. A study conducted in Japan found advanced chronic kidney disease to be an independent risk factor.[10]
Evaluation
Initial evaluation of acute arterial occlusion begins with a physical exam. A detailed physical examination should assess for changes in temperature along the affected extremity. A comparison should always be made with the unaffected side. A complete bilateral pulse exam should be conducted with manual palpation, and an arterial Doppler exam should be included when the deficient pulse is noted.[11] Muscle strength and sensation testing should also be assessed. When occlusion has been identified, confirmatory testing with a CT angiogram is generally conducted as it is quicker and more readily available.[12] However, the time required to order, perform and interpret imaging must be balanced against the urgency for treatment to preserve life and limb. Since most episodes of acute limb ischemia present to the emergency department, an immediate vascular surgery consult must be initiated. The severity of ischemia can be further assessed with the physical exam, utilizing the Rutherford classification of acute limb ischemia. Finding the cause of occlusion is also essential. For example, a patient with a history of atrial fibrillation with abrupt initial symptoms is more likely to have an embolic occlusion than a patient with a history of PAD and claudication more prone to having a thrombotic source.[13]
Treatment / Management
Cases of limb-threatening ischemia require emergent vascular surgery consult. The surgical approach is directed at the reperfusion of the affected extremity. This can be accomplished by surgical bypass, endarterectomy, or embolectomy. Results are variable and will ultimately depend on the duration of the ischemia and the extent of occlusion. Catheter-directed thrombolysis by an interventional radiologist is becoming more common and is reserved for patients with a salvageable limb (Rutherford class II, IIa, and IIb). Patients presenting with profound paralysis and absent pain with inaudible arterial and venous pulses are considered to have irreversible damage and will require amputation. Surgical treatment options are typically reserved for more severe cases or where nonsurgical management fails. These options include the following:
- Open bypass surgery
- Endovascular therapy, such as stenting, balloon angioplasty, or atherectomy
Whereas open surgery was a popular treatment option 2 decades ago, endovascular therapy for PAD has become increasingly popular since then.[14] While the patient waits for surgical or interventional radiology assessment, initial therapy should include fluid resuscitation, pain control, and administration of unfractionated heparin to minimize thrombus propagation. The general goal of anticoagulation is to increase partial thromboplastin by a factor of 2.0 to 2.5 above baseline. Management after revascularization requires close and frequent observation. Prolonged ischemia of greater than 4 hours increases the risk of compartment syndrome and must be monitored with hourly neurovascular checks.[15][16][17]
Differential Diagnosis
Acute arterial occlusion can present in a variety of ways and can mimic several underlying pathological processes. Whenever a patient presents with pain and other relevant features of arterial ischemia, the following differentials should be considered:
- Arterial embolus
- Acute arterial thrombosis
- Aortic dissection
- Chronic exertional compartment syndrome
- Chronic venous insufficiency
- Degenerative disk disease
- Osteoarthritis
- Spinal stenosis
- Thromboangiitis obliterans
- Varicose vein surgery
Staging
The Society for Vascular Surgery has created a classification of an acutely ischemic limb:
- Class I: Non-threatened extremity; elective revascularization may or may not be necessary
- Class II: Threatened extremity; immediate revascularization is indicated to prevent tissue loss
- Class III: Ischemia has progressed to infarction, and salvage of the extremity is not possible
Prognosis
A study conducted on a group of patients with arterial occlusive disease reported that two-thirds of the patients required surgery at the beginning of their hospitalization for ongoing severe ischemia. While the mortality due to acute thrombosis was lower, the risk of major amputation was found to be 35%. They concluded that vascular reconstruction should not be delayed in acute arterial ischemia secondary to thrombosis.[18]
Complications
The following is a list of complications that patients can develop as a result of acute arterial occlusion:
- Compartment syndrome[19]
- Amputation
- Necrosis and gangrene
- Bleeding
- Stroke
- Myocardial infarction
- Death
Postoperative and Rehabilitation Care
Once the acutely ischemic limb has been managed, these patients need to be monitored in the ICU. If the patient has peripheral vascular disease or atrial fibrillation, aspirin or an oral anticoagulant may be required. The cause of the ischemic limb must be investigated to prevent a recurrence. Since many of these patients are frail, physical therapy should be involved in restoring function.
Deterrence and Patient Education
It is advisable to make the patients aware of the possible risk factors and how to manage them. The following is a list of factors that can help prevent major occlusive events:
- Discontinue smoking[20]
- Control hypertension
- Manage diabetes
- Maintain a healthy weight
- Remain compliant with medications
Pearls and Other Issues
Reperfusion injury may result in the target limb after therapy. This can include profound edema, causing increased compartmental pressures. Signs and symptoms of reperfusion injury include severe pain, focal weakness, and hypoesthesia. In addition, laboratory studies may reveal elevated creatine kinase and myoglobinuria. Most cases of compartment syndrome secondary to reperfusion injury involve the anterior compartment of the leg; therefore, assessment of peroneal nerve function is critical. Reperfusion injury can also cause cardiac, renal, and pulmonary complications, making prompt recognition and treatment just as important as the initial diagnosis of acute arterial occlusion.
Enhancing Healthcare Team Outcomes
Patients with acute ischemic limbs need an interprofessional approach, in collaboration with an interprofessional team consisting of a vascular surgeon, interventional radiologist, nurse, infectious disease, and critical care. Early therapy is critical if one wants to salvage the limb. In addition, most of these patients have other comorbidities like heart disease, obstructive lung disease, diabetes, and obesity, which also affect survival. The patient is best managed in the ICU, where a nurse can closely monitor the vital signs and peripheral pulses. The American College of Radiology has established evidence-based guidelines to determine the type of imaging in these patients.[5][21] For those not deemed surgical candidates, catheter-directed thrombolysis may be undertaken. To prevent additional morbidity, the pharmacist must be fully aware of all the indications and contraindications of this therapy. For those who undergo thrombolysis or angiogram, the nurse is responsible for monitoring the leg for viability and bleeding in the groin, where access to the artery is obtained. Open communication channels between all team members are crucial to positive patient outcomes, as is accurate and updated patient record-keeping.
Outcomes
The outcomes for patients with an acutely ischemic limb are guarded. Even if the limb is salvaged, these patients have other comorbidities, which can lead to a heart attack, renal failure, stroke, or wound infection. Unless an interprofessional team is involved, the mortality for these individuals remains high. Expert opinion is highly recommended when these patients present to the emergency room because the earlier the comorbidity is managed, the lower the risk of complications.[22][23]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Curtis W, Yano M. Acute non-traumatic disease of the abdominal aorta. Abdominal radiology (New York). 2018 May:43(5):1067-1083. doi: 10.1007/s00261-018-1525-0. Epub [PubMed PMID: 29492609]
Sedghi Y, Collins TJ, White CJ. Endovascular management of acute limb ischemia. Vascular medicine (London, England). 2013 Oct:18(5):307-13. doi: 10.1177/1358863X13505643. Epub 2013 Oct 4 [PubMed PMID: 24097417]
Level 3 (low-level) evidenceWalker TG. Acute limb ischemia. Techniques in vascular and interventional radiology. 2009 Jun:12(2):117-29. doi: 10.1053/j.tvir.2009.08.005. Epub [PubMed PMID: 19853229]
Hamburg NM,Creager MA, Pathophysiology of Intermittent Claudication in Peripheral Artery Disease. Circulation journal : official journal of the Japanese Circulation Society. 2017 Feb 24; [PubMed PMID: 28123169]
Engledow AH, Crinnion JN. Acute lower limb ischaemia. Hospital medicine (London, England : 1998). 2002 Jul:63(7):412-5 [PubMed PMID: 12187601]
Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004 Aug 10:110(6):738-43 [PubMed PMID: 15262830]
Level 2 (mid-level) evidenceSaltin B, Rådegran G, Koskolou MD, Roach RC. Skeletal muscle blood flow in humans and its regulation during exercise. Acta physiologica Scandinavica. 1998 Mar:162(3):421-36 [PubMed PMID: 9578388]
Malinow MR. Plasma homocyst(e)ine and arterial occlusive diseases: a mini-review. Clinical chemistry. 1995 Jan:41(1):173-6 [PubMed PMID: 7813076]
Obara H, Matsubara K, Kitagawa Y. Acute Limb Ischemia. Annals of vascular diseases. 2018 Dec 25:11(4):443-448. doi: 10.3400/avd.ra.18-00074. Epub [PubMed PMID: 30636997]
Yamasaki S, Izawa A, Koshikawa M, Saigusa T, Ebisawa S, Miura T, Shiba Y, Tomita T, Miyashita Y, Koyama J, Ikeda U. Association between estimated glomerular filtration rate and peripheral arterial disease. Journal of cardiology. 2015 Nov:66(5):430-4. doi: 10.1016/j.jjcc.2015.01.011. Epub 2015 Apr 13 [PubMed PMID: 25881730]
Katzen BT. Clinical diagnosis and prognosis of acute limb ischemia. Reviews in cardiovascular medicine. 2002:3 Suppl 2():S2-6 [PubMed PMID: 12556737]
Olinic DM, Stanek A, Tătaru DA, Homorodean C, Olinic M. Acute Limb Ischemia: An Update on Diagnosis and Management. Journal of clinical medicine. 2019 Aug 14:8(8):. doi: 10.3390/jcm8081215. Epub 2019 Aug 14 [PubMed PMID: 31416204]
O'Connell JB, Quiñones-Baldrich WJ. Proper evaluation and management of acute embolic versus thrombotic limb ischemia. Seminars in vascular surgery. 2009 Mar:22(1):10-6. doi: 10.1053/j.semvascsurg.2008.12.004. Epub [PubMed PMID: 19298930]
Rowe VL, Lee W, Weaver FA, Etzioni D. Patterns of treatment for peripheral arterial disease in the United States: 1996-2005. Journal of vascular surgery. 2009 Apr:49(4):910-7. doi: 10.1016/j.jvs.2008.11.054. Epub [PubMed PMID: 19341885]
Khan MI, Nadeem IA. Revascularization Of Late-Presenting Acute Limb Ischaemia And Limb Salvage. Journal of Ayub Medical College, Abbottabad : JAMC. 2016 Apr-Jun:28(2):262-266 [PubMed PMID: 28718559]
Shin HS, Kyoung KH, Suh BJ, Jun SY, Park JK. Acute limb ischemia: surgical thromboembolectomy and the clinical course of arterial revascularization at ankle. The International journal of angiology : official publication of the International College of Angiology, Inc. 2013 Jun:22(2):109-14. doi: 10.1055/s-0033-1336827. Epub [PubMed PMID: 24436594]
Nelson JA. Compartment pressure measurements have poor specificity for compartment syndrome in the traumatized limb. The Journal of emergency medicine. 2013 May:44(5):1039-44. doi: 10.1016/j.jemermed.2012.09.040. Epub 2013 Jan 12 [PubMed PMID: 23321294]
Cambria RP, Abbott WM. Acute arterial thrombosis of the lower extremity. Its natural history contrasted with arterial embolism. Archives of surgery (Chicago, Ill. : 1960). 1984 Jul:119(7):784-7 [PubMed PMID: 6732488]
Gourgiotis S, Villias C, Germanos S, Foukas A, Ridolfini MP. Acute limb compartment syndrome: a review. Journal of surgical education. 2007 May-Jun:64(3):178-86 [PubMed PMID: 17574182]
Powell JT. Vascular damage from smoking: disease mechanisms at the arterial wall. Vascular medicine (London, England). 1998:3(1):21-8 [PubMed PMID: 9666528]
Expert Panel on Vascular Imaging:, Weiss CR, Azene EM, Majdalany BS, AbuRahma AF, Collins JD, Francois CJ, Gerhard-Herman MD, Gornik HL, Moriarty JM, Norton PT, Ptak T, Reis SP, Rybicki FJ, Kalva SP. ACR Appropriateness Criteria(®) Sudden Onset of Cold, Painful Leg. Journal of the American College of Radiology : JACR. 2017 May:14(5S):S307-S313. doi: 10.1016/j.jacr.2017.02.015. Epub [PubMed PMID: 28473087]
Akagi D, Hoshina K, Akai A, Yamamoto K. Outcomes in Patients with Critical Limb Ischemia due to Arteriosclerosis Obliterans Who Did Not Undergo Arterial Reconstruction. International heart journal. 2018 Sep 26:59(5):1041-1046. doi: 10.1536/ihj.17-592. Epub 2018 Aug 11 [PubMed PMID: 30101855]
Schaumeier MJ, Hawkins AT, Hevelone ND, Sethi RKV, Nguyen LL. Association of Treatment for Critical Limb Ischemia with Gender and Hospital Volume. The American surgeon. 2018 Jun 1:84(6):1069-1078 [PubMed PMID: 29981651]