Introduction
A double-lumen tube (DLT) is an endotracheal tube designed to isolate the lungs anatomically and physiologically.[1] Double-lumen tubes (DLTs) are the most commonly used tubes to provide independent ventilation for each lung. One-lung ventilation (OLV) or lung isolation is the mechanical and functional separation of the 2 lungs to allow selective ventilation of only one lung. The other lung that is not being ventilated passively deflates or is displaced by the surgeon to facilitate surgical exposure for non-cardiac operations in the chest such as thoracic, esophageal, aortic and spine procedures. It can also be used during minimally invasive cardiac surgery and in disease processes affecting 1 lung to prevent soiling from the contralateral lung. DLTs also allows bronchial toilet without interrupting ventilation.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
For successful placement of a DLT, it is important to understand the anatomy of the trachea and bronchi. In humans, the trachea arises at the level of the cricoid cartilage and extends up to carina the narrowest portion of the airway in adults, where it bifurcates into right and left main stem bronchus. The average length of the adult trachea is 12 cm and comprises 18 to 22 C-shaped cartilaginous rings anterolaterally, the ends of which are linked posteriorly by the superficial membranous wall and the trachealis muscle.
The right mainstem bronchus lies in a more vertical plane, is shorter (averages 1.9 cm in men and 1.5 cm in women) and larger than the left main stem bronchus. The left mainstem bronchus lies in a more horizontal plane and averages about 4.9 cm in men and 4.4 cm in women.
The left lung is 10% smaller than the right lung and comprises 2 lobes, the superior and inferior lobes, while the right lung comprises three lobes — the superior, middle and inferior lobes. Each of the lobes is divided by connective tissue into anatomical compartments known as bronchopulmonary segments, supplied by segmental (tertiary) bronchus and artery. Each bronchopulmonary segment is functionally and anatomically discrete and can be resected (segmentectomy) without affecting each other. In general, each lung has 10 bronchopulmonary segments.
Ventilation and perfusion of the lungs are well-matched anatomically, with dependent portions of the lungs receiving both greater blood flow (perfusion) because of gravity and greater ventilation because of the gravitational effect of lung compliance. The initiation of OLV stops all ventilation to one lung, which creates an obligatory shunt (i.e., that lung is perfused but not ventilated). because the left lung is smaller, there is less shunt when the left lung is collapsed.
Indications
A DLT is indicated for surgeries or procedures requiring lung isolation.[2][3]
Absolute Indications
- Preventing damage or contamination of the healthy lung
- Prevent spillage of contamination from a lung abscess
- Prevent spillage of blood from one lung to another in pulmonary hemorrhage
- Control of distribution of ventilation
- Reduction of flow through a broncho-pleural or broncho-pleural cutaneous fistula where low resistance to flow from one lung may make it difficult to ventilate another lung.
- Bronchial disruption from trauma
- Severe unilateral lung disease: Major cyst or bulla
- Surgical exposure in video-assisted thoracoscopic surgery (VATS)
- Single lung lavage: Treatment for pulmonary alveolar proteinosis or cystic fibrosis
Relative Indications
- Deflation of one lung to provide motionless field and better surgical exposure for:
- Thoracic aortic surgery
- Mediastinal surgery
- Esophageal surgery
- Open pulmonary resection (lobectomy or pneumonectomy)
Contraindications
Due to the larger size and more complex design than the single lumen tube (SLT), intubation with a DLT can be a challenge, even in a patient with a normal airway. Use of a DLT is therefore relatively contraindicated in a patient with[4]:
- A difficult airway
- A preexisting trachea or stoma
- A tracheal constriction
- Limited mouth opening
Distorted airway anatomy due to tortuosity or lesion extending into the airway is a contraindication to placement of DLT. In certain instances, such as where conversion to an SLT may be needed at any time during surgery or the need to re-intubate for postoperative mechanical ventilation is warranted, it is advisable to choose an SLT with a bronchial blocker for lung isolation. The need to re-intubate with an SLT may be risky due to the presence of airway edema.
DLTs specially designed for patients with a tracheostomy (double-lumen tracheostomy tube set) are commercially available. They have the same design as conventional DLTs but are shorter and curved between the intratracheal and extra tracheal parts.[5][6] however, its use is limited.
Equipment
DLTs have 2 endotracheal tubes (ETT) that are "bonded" together, to allow each tube to ventilate a specific lung. The DLT can be left-sided or right-sided depending on the main stem bronchus which its distal (longer) lumen is designed to fit in. The longer lumen (bronchial lumen) is designed to reach the main stem bronchus while the shorter lumen (tracheal) ends in the distal trachea. [Figure 1] There are several types of double lumen tubes. However, all are similar in design and made of Polyvinyl chloride. Most DLTs have color-coded cuffs and pilot balloons. The bronchial cuff, which is typically a high-pressure low volume cuff, and its pilot balloon are blue, while the tracheal cuff which is a high volume low-pressure cuff, and its pilot balloon are clear.[7][8]
The DLT is supplied in a package containing the tube with a stylet, connector, and suction catheters. Depending on the manufacturer, they may also come with an apparatus to provide continuous positive airway pressure (CPAP) to the non-ventilated lung. There are different manufacturers.
When seen in cross-section, each tube is D shaped. They come in different sizes — 26 Fr, 28 Fr, 32 Fr, 35 Fr, 37 Fr, 39 Fr, and 41 Fr.[9][10] A 26 Fr DLT can be used in children over the age of 8 years. [10]Placing a larger DLT may cause trauma to the airway and placing too small a DLT may fail to provide lung isolation requiring cuff hyperinflation as a result which can cause trauma and ischemia to the airway. Smaller tubes are also more likely to migrate distally and may be difficult to suction and ventilate through.
The margin of safety is higher for the placement of left-sided DLT due to the longer length of the left main stem bronchus. Placement of a right-sided DLT is more challenging with a lower safety margin due to the short length of the right mainstem bronchus and the origination of the right-upper lobe bronchus 1.5 to 2 cm from the carina.[11] Right-sided DLT, as a result, incorporates a modified cuff, or slot on the endobronchial side that allows ventilation of the right upper lobe. Placement of a right-sided DLT needs to be positioned to align with the takeoff of the right upper lobe. (Figure 1)
Reviewing a chest x-ray, CT scan, or MRI before placing a right-sided DLT may help to locate the position of the right upper lobe take off from the right mainstem bronchus.
Because of the higher safety margin, a left-sided DLT is commonly used. However, right-sided DLT may be preferred when it is important to avoid manipulation of left bronchus or when left bronchus is narrowed or has anatomical variations, left pneumectomy, left lung transplant, left mainstem bronchus stent or suspected disruption of the left tracheobronchial tree.
Personnel
Personnel responsible for the placement of a DLT for lung isolation include an anesthesiologist, certified registered nurse anesthetist (CRNA), or certified anesthesiologist assistant (CAA). A resident physician anesthesiologist, a student nurse anesthetist or student anesthesiologist assistant may place a DLT under the supervision of an anesthesiologist.
Preparation
When preparing the DLT for use, both the trachea and bronchial cuffs should be inflated to check for leaks and symmetrical cuff inflation. Consider adding water-soluble lubricant to the stylet and insert the stylet into the bronchial side, ensuring that the stylet is not protruding beyond the tube. The connector, which connects DLT to the ventilator circuit, should be assembled and ready before intubation. A fiberoptic Bronchoscope should be available to confirm the position of the DLT.[12] Knowledge of the tracheobronchial anatomy is very helpful in confirming the correct placement of the DLT. See Figure. Optimal Position of Right- and Left-Sided Double Lumen Tubes.
There is a lack of objective guidelines in the proper selection of DLT sizes; 39-Fr and 41-Fr tubes are used for adult males while 35-Fr and 37-Fr DLTs are used for adult females. A properly-sized DLT is one in which the main body of the tube passes without resistance through the glottis and advances easily within the trachea and in which the bronchial component passes into the intended bronchus without difficulty.[13]
Technique or Treatment
There are 2 techniques used for the insertion of a DLT:
- Blind insertion
- Fiberoptic guided placement
For blind insertion of a DLT, first, perform a direct laryngoscopy and visualize the vocal cords. Visualization of the vocal cords is important as these tubes are large and placement more challenging than placing an SLT. Once the vocal cords are visualized, gently advance the DLT with the tip of the bronchial concave curve facing anteriorly through the vocal cords until the bronchial cuff passes through the cords. The tube is then turned 90 degrees to the left when using a left-sided DLT, and to the right when using a right-sided DLT, and advanced until it meets resistance. Once the DLT is well positioned, inflate the tracheal cuff and ensure ventilation of both lungs by both inspection and auscultation. Verify correct placement by checking ventilation through the bronchial lumen. First, inflate the bronchial cuff 1ml at a time until leak stops. Clamp off gas flow through the tracheal lumen at the Y connector and open the tracheal sealing cap to air. Check whether you can isolate the other lung through the tracheal lumen, by clamping off the gas flow through the bronchial lumen.[14]
The DLT can also be positioned using fiberoptic bronchoscopy. Using a fiberoptic bronchoscope through the bronchial lumen and guiding the DLT over fiber-optic scope increases the accuracy of placement.
Once inserted, the DLT is connected to the ventilator circuit via the DLT connector, and the detection of ETCO2 confirms placement in the trachea after both cuffs are inflated to seal leaks. No more than 3 mL of air should be required to create a seal in the bronchial cuff. Cuff pressures should be measured to prevent airway injury. Confirmation of correct positioning of the DLT can be done by auscultation or with fiberoptic bronchoscopy. Auscultation and bilateral chest wall movement is first confirmed. On clamping the endobronchial lumen limb connector, breath sounds should be absent from the corresponding side of the lung if the endobronchial lumen is in the correct bronchus. On clamping the endotracheal limb connector and ventilating through the endobronchial lumen, breath sounds should be absent from the opposite side of the chest.
Once the DLT is in place, confirm correct placement by inserting the fiberoptic scope through the tracheal lumen to verify that the bronchial lumen is in the correct main-stem bronchus and there is no bronchial cuff herniation.[15][12]
Though the tracheal lumen confirm that:
- The endobronchial portion is in the correct main bronchus. Left-sided DLT should be in the left main bronchus, and right-sided DLT should be in the right main bronchus.
- The bronchial rings should be anterior with the longitudinal fibers posterior to help with side identification.
- The bronchial cuff should be just visible without cuff herniation over the carina when inflated.
- The right upper lobe (RUL) bronchus should be identifiable via the right main bronchus with 3 lobar branches (apical, anterior and posterior).
Next, the fiberoptic bronchoscope is advanced through the endobronchial lumen.
- For a left-sided DLT, identify the origins of the left upper and lower bronchi (confirm that the tip of the endobronchial orifice is not occluding the left upper or lower bronchi).
- For a right-sided DLT, identify good alignment between the opening slot of the endobronchial lumen relative to the takeoff of the right upper lobe bronchus (to allow ventilation of the right upper lobe bronchus).
- Identify the bronchus intermedius and the right lower lobe bronchus distally.
Fiberoptic bronchoscopy is the gold standard for confirmation of correct placement of a DLT. Auscultation alone is unreliable as an indicator of proper DLT placement.[16]
Troubleshooting techniques for DLT insertion include:
- Using a bronchoscope to cannulate the bronchus and railroading the tube over the scope. Always place the scope in the bronchial (longer) lumen.
- A stylet should be used when placing a DLT.
- Always check placement when changes to the patient's position have been made, or changes have been made between normal ventilation and isolated lung ventilation.
- To assist in cannulating the bronchus, rotate tube toward bronchus that is to be cannulated, turn the patient's head to the opposite side and gently slide the tube down until resistance is felt.
To initiate one-lung ventilation, the bronchial cuff is inflated, the lung to be isolated is clamped off at the corresponding connector, the connector is then opened to the atmosphere to allow lung collapse. Lung collapse is most rapid if initiated at end expiration.
Intraoperatively the bronchial cuff should be kept deflated (unless needed to avoid the spread of blood or infection) and should be inflated only during the time of lung isolation to minimize bronchial mucosal injury.
Complications
The most lethal complication arising from the use of a DLT is airway rupture from traumatic placement.[17][18] Injury to tongue, lips, and teeth may also occur from laryngoscopy. A majority of airway injuries were associated with undersized DLTs, particularly in females who received a 35-Fr or 37-Fr DLT.[19] Undersized DLTs tend to migrate too far distally into the main stem bronchus, or that the endobronchial cuff requires a larger amount of air when smaller tubes are used predisposing to mucosal ischemia.
Other complications include hypoxemia due to tube malposition, displacement, tube occlusion from secretions or blood. Inadvertent entrapment of the DLT in suture lines during procedures have also been reported.
Malposition of the DLT can lead to life-threatening consequences. Ventilation can be severely impaired, leading to hypoxia, gas trapping, tension pneumothorax, cross-contamination of lung contents, and interference with surgical procedures.[20]
Factors predisposing to airway injury include:
- Inserting a DLT too forcefully
- Placing undersized DLTs
- Overdistention of the endobronchial cuff
- Reposition of the DLT with the cuffs inflated
- Preexisting pathology of the airway including tumors
Clinical Significance
Double lumen tubes play a crucial role in:
- Airway management during thoracic surgery
- Anatomical lung separation or isolating normal from the diseased lung in situations such as:
- Massive hemorrhage from one lung
- Whole lung lavage in patients with pulmonary alveolar proteinosis
- Avoiding spillage of purulent secretions from one lung to another
- Differential lung protective ventilation in case of lung transplantation patients
Enhancing Healthcare Team Outcomes
Double-lumen tubes are used for multiple complex surgical procedures and lung isolation in some non-surgical patients. Since malposition and displacement of these tubes can lead to life-threatening consequences, an interprofessional education is an essential component to avoid morbidity and mortality. Everyone involved in the care of patients requiring DLT placement including anesthesiologists, intensivists, resident physicians, CRNAs, AAs, nurses, and respiratory therapists in the intensive care unit must know the indications for placement, identify correct placement, confirm the position, and be able to troubleshoot complications from the placement of DLT. Daily chest x-ray and auscultation to confirm placement and bronchoscopy should be immediately available if malposition is suspected. Respiratory status should be monitored continuously, and caution should be used during the positioning and transport of patients. The need for continued placement should be addressed daily as these tubes have the potential for airway injury and should be changed to SLTs if mechanical ventilation is still needed, but lung isolation is no longer indicated.
Media
(Click Image to Enlarge)
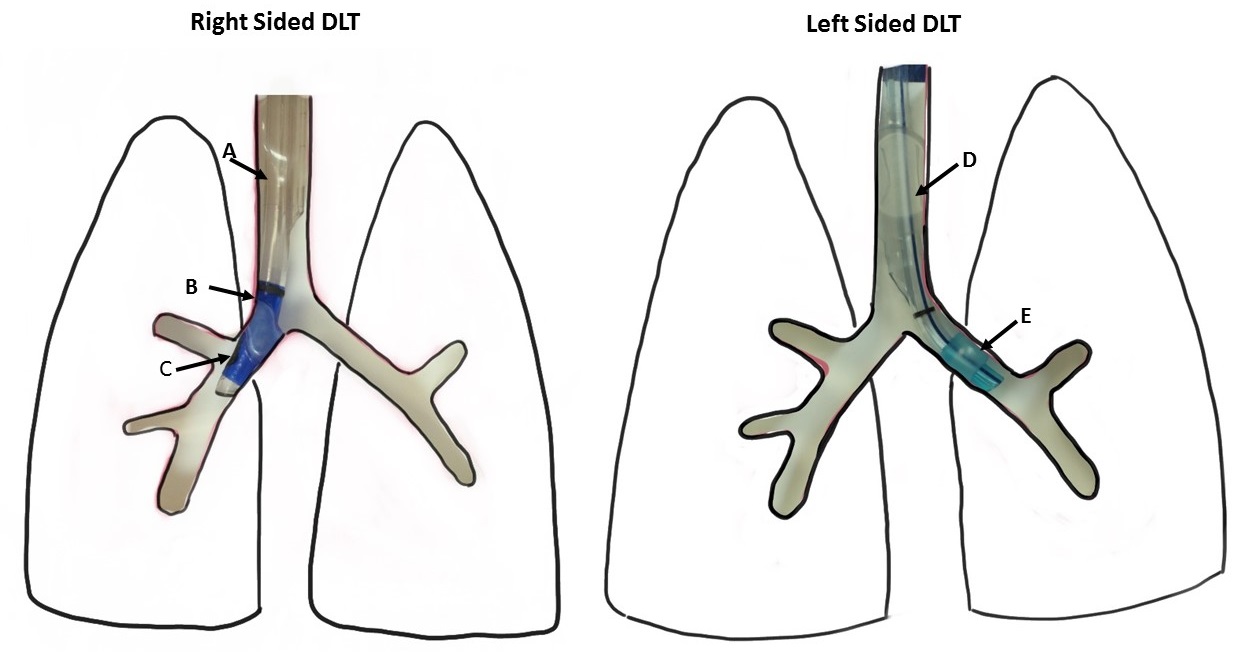
Optimal Position of Right- and Left-Sided Double Lumen Tubes. The illustration shows the tracheal cuff of the right DLT (A), the bronchial cuff of the right DLT (B), the slot of the endobronchial lumen properly aligned with the opening of the right upper lobe bronchus (C), the tracheal cuff of the Left DLT (D), and the bronchial cuff of the Left DLT (E).
Created by M Mehrotra, MD, and M Arthur, MD
References
Campos JH. Lung isolation techniques. Anesthesiology clinics of North America. 2001 Sep:19(3):455-74 [PubMed PMID: 11571902]
Campos JH. Current techniques for perioperative lung isolation in adults. Anesthesiology. 2002 Nov:97(5):1295-301 [PubMed PMID: 12411817]
Lewis JW Jr, Serwin JP, Gabriel FS, Bastanfar M, Jacobsen G. The utility of a double-lumen tube for one-lung ventilation in a variety of noncardiac thoracic surgical procedures. Journal of cardiothoracic and vascular anesthesia. 1992 Dec:6(6):705-10 [PubMed PMID: 1472668]
Campos JH, Lung isolation techniques for patients with difficult airway. Current opinion in anaesthesiology. 2010 Feb [PubMed PMID: 19752725]
Level 3 (low-level) evidenceMasamune T, Matsukawa T, Ookawa I, Sasuga M, Tamaki F, Kumazawa T. [Double-lumen tracheostomy tube (Tracheopart) used in two patients for one-lung ventilation under general anesthesia]. Masui. The Japanese journal of anesthesiology. 2004 Dec:53(12):1418-20 [PubMed PMID: 15682807]
Level 3 (low-level) evidenceDincq AS, Lessire S, Mayné A, Putz L. Double-lumen tubes for tracheostomized patients. Journal of cardiothoracic and vascular anesthesia. 2015 Jun:29(3):e35-6. doi: 10.1053/j.jvca.2015.02.011. Epub 2015 Feb 7 [PubMed PMID: 25863729]
Brodsky JB, Lemmens HJ. Left double-lumen tubes: clinical experience with 1,170 patients. Journal of cardiothoracic and vascular anesthesia. 2003 Jun:17(3):289-98 [PubMed PMID: 12827573]
Narayanaswamy M, McRae K, Slinger P, Dugas G, Kanellakos GW, Roscoe A, Lacroix M. Choosing a lung isolation device for thoracic surgery: a randomized trial of three bronchial blockers versus double-lumen tubes. Anesthesia and analgesia. 2009 Apr:108(4):1097-101. doi: 10.1213/ane.0b013e3181999339. Epub [PubMed PMID: 19299767]
Level 1 (high-level) evidencePedoto A. How to choose the double-lumen tube size and side: the eternal debate. Anesthesiology clinics. 2012 Dec:30(4):671-81. doi: 10.1016/j.anclin.2012.08.001. Epub [PubMed PMID: 23089502]
Fabila TS, Menghraj SJ. One lung ventilation strategies for infants and children undergoing video assisted thoracoscopic surgery. Indian journal of anaesthesia. 2013 Jul:57(4):339-44. doi: 10.4103/0019-5049.118539. Epub [PubMed PMID: 24163446]
Benumof JL, Partridge BL, Salvatierra C, Keating J. Margin of safety in positioning modern double-lumen endotracheal tubes. Anesthesiology. 1987 Nov:67(5):729-38 [PubMed PMID: 3674473]
Slinger PD. Fiberoptic bronchoscopic positioning of double-lumen tubes. Journal of cardiothoracic anesthesia. 1989 Aug:3(4):486-96 [PubMed PMID: 2520925]
Campos JH. Progress in lung separation. Thoracic surgery clinics. 2005 Feb:15(1):71-83 [PubMed PMID: 15707347]
Pennefather SH, Russell GN. Placement of double lumen tubes--time to shed light on an old problem. British journal of anaesthesia. 2000 Mar:84(3):308-10 [PubMed PMID: 10793587]
Klein U, Karzai W, Bloos F, Wohlfarth M, Gottschall R, Fritz H, Gugel M, Seifert A. Role of fiberoptic bronchoscopy in conjunction with the use of double-lumen tubes for thoracic anesthesia: a prospective study. Anesthesiology. 1998 Feb:88(2):346-50 [PubMed PMID: 9477054]
Alliaume B, Coddens J, Deloof T. Reliability of auscultation in positioning of double-lumen endobronchial tubes. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 1992 Sep:39(7):687-90 [PubMed PMID: 1394757]
Burton NA, Fall SM, Lyons T, Graeber GM. Rupture of the left main-stem bronchus with a polyvinylchloride double-lumen tube. Chest. 1983 Jun:83(6):928-9 [PubMed PMID: 6851700]
Level 3 (low-level) evidenceWagner DL, Gammage GW, Wong ML. Tracheal rupture following the insertion of a disposable double-lumen endotracheal tube. Anesthesiology. 1985 Dec:63(6):698-700 [PubMed PMID: 4061926]
Level 3 (low-level) evidenceFitzmaurice BG, Brodsky JB. Airway rupture from double-lumen tubes. Journal of cardiothoracic and vascular anesthesia. 1999 Jun:13(3):322-9 [PubMed PMID: 10392687]
Gibbs N, Giles K. Malposition of left-sided PVC double-lumen endobronchial tubes. Anaesthesia and intensive care. 1986 Feb:14(1):92 [PubMed PMID: 3954023]
Level 3 (low-level) evidence