Introduction
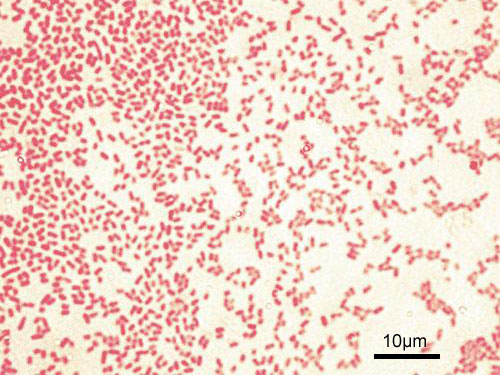
Pseudomonas aeruginosa is a gram-negative, aerobic, non-spore forming rod that is capable of causing a variety of infections in both immunocompetent and immunocompromised hosts.[1] Its predilection to cause infections among immunocompromised hosts, extreme versatility, antibiotic resistance, and a wide range of dynamic defenses makes it an extremely challenging organism to treat in modern-day medicine.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Pseudomonas aeruginosa is commonly found in the environment, particularly in freshwater. Reservoirs in urban communities include hot tubs, jacuzzis, and swimming pools. It can cause a wide array of community-acquired infections like folliculitis, puncture wounds leading to osteomyelitis, pneumonia, otitis externa, and many others. It is commonly an opportunistic pathogen and is also an important cause of nosocomial infections like ventilator-associated pneumonia, catheter-associated urinary tract infections, and others. Reservoirs in the hospital setting include potable water, taps, sinks, toothbrushes, icemakers, disinfecting solutions, sanitizers, soap bars, respiratory therapy equipment, endoscopes, and endoscope washers.[1][2]
Epidemiology
Pseudomonas aeruginosa infections are common in individuals with an immunocompromised state such as cystic fibrosis, bronchiectasis, neutropenia, burns, cancer, AIDS, organ transplant, uncontrolled diabetes mellitus, and ICU admissions. Individuals with invasive devices e.g., indwelling catheters or endotracheal tubes, are also at risk due to the organism's unique ability to form biofilms that are difficult to detect.[2]
Pathophysiology
Pseudomonas aeruginosa possesses many mechanisms for antibiotic resistance and a variety of virulence factors that collectively account for the broad-spectrum of infections it causes and the increasingly challenging treatment for the resulting antimicrobial resistance. Multiple mechanisms have been identified for Pseudomonas antibiotic resistance, examples are intrinsic antibiotic resistance, efflux systems, and antibiotic-inactivating enzymes.[3] Intrinsic antibiotic resistance is the ability to restrict membrane permeability to antimicrobials. Efflux systems allow the bacterium to direct harmful or toxic compounds outside the cell membrane. Additionally, many isolates possess beta-lactamases and extended-spectrum beta-lactamases (ESBLs). The ability of Pseudomonas bacteria to form a biofilm is also an important mechanism with which it can increase antibiotic resistance and resist host defenses.[2][3] This is especially important in cystic fibrosis patients, where most patients acquire the infection in the first year of life either from the environment or from healthcare facilities (inpatient or outpatient settings).
History and Physical
Pseudomonas aeruginosa causes a wide spectrum of infections with varying severity, examples include:
- Pseudomonas folliculitis is characterized by a maculopapular pruritic rash, axillary lymphadenopathy, breast tenderness, and fever. It is associated with the use of hot tubs, jacuzzis, and pools.[4]
- Puncture wounds in the foot, especially in children, can lead to infection with Pseudomonas. A classical scenario is a nail or glass injury through rubber shoes or soles. Local tenderness, purulent discharge, other signs of infection are found; however, delay in the presentation and diagnosis due to lack of symptoms initially may predispose to serious complications like osteomyelitis and septic arthritis.[5]
- In cystic fibrosis exacerbations, pseudomonal coverage is always needed. Chronic infection with Pseudomonas aeruginosa occurs in more than 60% of adults with cystic fibrosis and is linked to higher mortality.[2][6]
- In patients with burns, Pseudomonas infections were found to decline and are replaced by gram-positive organisms and other emerging gram-negative organisms e.g., Aeromonas hydrophila.[7] In pseudomonal burn infections, a blue-green purulent discharge may be found, among other signs of local and systemic inflammation, and it may progress to sepsis and septic shock.
- Patients with diabetes are more likely to develop malignant otitis externa caused by Pseudomonas and present with otalgia and otorrhea. Examination frequently reveals granulation tissue inside the ear canal.[8]
- Populations at-risk are extremely susceptible to pneumonia caused by Pseudomonas. Pseudomonas pneumonia should be considered in any patient who has signs and symptoms of pneumonia and who is immunocompromised.[9]
- While patients with an organ transplant in general, are susceptible to all systemic pseudomonal infections, kidney transplant patients are at increased risk of recurrent pseudomonal urinary tract infections.[10]
- Other examples include endophthalmitis, endocarditis, meningitis, and many others.[11]
Evaluation
Lesion culture from patients with folliculitis after the use of hot tubs frequently grow Pseudomonas aeruginosa.[4] In puncture wounds and malignant otitis externa, clinicians should look for early signs of deep tissue involvement. Imaging may be needed to exclude soft tissue, bone, and joint involvement.[5] In systemic infections, routine laboratory and imaging workup are needed in addition to blood, urine, and tissue cultures if necessary. Due to the high prevalence of antibiotic resistance, the determination of sensitivity to different antimicrobials in pseudomonal infections is extremely important as they guide therapy.
Treatment / Management
Clinicians should consider pseudomonal infections in all at-risk patient groups and exert a high level of suspicion in severe infections leading to respiratory failure, septic shock, or any ICU admission. Hot tub folliculitis is generally self-limited, and no intervention is required, although antipseudomonal antibiotics may be needed.[4] In puncture wounds, in addition to regular staph and strep coverage, clinicians should consider pseudomonal coverage, especially if there are signs of deep infection.[5] Extended courses of IV antibiotics and surgical debridement may be needed.[8] In respiratory failure, pneumonia, sepsis, septic shock, and all systemic infections requiring an ICU admission, Pseudomonas infections should be considered upon presentation. The local antibiogram is extremely important to guide empiric therapy until sensitivity results are available. In addition to broad-spectrum antibiotic coverage, double pseudomonal coverage may be needed in cases of septic shock, respiratory failure requiring mechanical ventilation, ICU admissions, and the presence of one or more risk factors for multi-drug resistant organisms.[9] Some agents from multiple antibiotic groups have pseudomonal coverage. Carbapenems (e.g., meropenem), cephalosporins (e.g., ceftazidime, cefepime), aminoglycosides (e.g., gentamicin, tobramycin, and amikacin), and fluoroquinolones (e.g., ciprofloxacin and levofloxacin) are generally used as first-line therapy until culture and sensitivity results are available.(B3)
Differential Diagnosis
Hot tub folliculitis should be differentiated from other causes of rash and skin infections. Malignant otitis externa is often confused with other ear infections. Bone involvement leading to osteomyelitis in malignant otitis externa and pseudomonal puncture wounds may need more aggressive interventions for diagnosis e.g., tissue or bone biopsy to differentiate other causes of infection. In systemic infections, other organisms that can cause overwhelming infections and sepsis should always be considered. Broad coverage is needed initially until culture and sensitivity results are obtained.
Prognosis
Fortunately, some pseudomonal infections are self-limited e.g., hot tub folliculitis.[4] Others may be more challenging but still have good outcomes, as is the case with pseudomonal osteomyelitis secondary to puncture wounds. However, long-term radiographic evidence persists in those cases.[5] In cases of pneumonia requiring mechanical ventilation, septic shock, and burn infections, the prognosis varies and is largely dependant on the severity of the underlying disease process and the availability of antimicrobial agents that remain with pseudomonal activity.[11]
Complications
Osteomyelitis of foot bones and septic arthritis may complicate foot puncture wounds.[5] Cranial nerve neuropathies can occur in advanced malignant otitis externa with severe skull base osteomyelitis.[8] Systemic pseudomonal infections can lead to respiratory failure, shock, and death.
Deterrence and Patient Education
Patients should be educated about the types of infections that Pseudomonas can cause and the risks associated with these infections.
Enhancing Healthcare Team Outcomes
Generally, clinicians should avoid prescribing antibiotics unless necessary. This prevents unnecessary costs, and prevents the emergence of resistant strains of bacteria, as is the case with all multi-drug resistant bacteria, including Pseudomonas. Targeted infection control practices aiming at the prevention of pseudomonal infections, especially in the hospital setting, are becoming increasingly important.[1] Analysis of various mechanisms of antibiotic resistance will be beneficial in determining the epidemiology and improve infection control.[12] An interprofessional team approach is needed to provide care to patients with known systemic Pseudomonas aeruginosa infections. Inclusion of infectious disease, orthopedic surgery, and plastic surgery early in the management of the patients provides better outcomes and long-term results in terms of morbidity and mortality.
Media
(Click Image to Enlarge)
References
Kerr KG, Snelling AM. Pseudomonas aeruginosa: a formidable and ever-present adversary. The Journal of hospital infection. 2009 Dec:73(4):338-44. doi: 10.1016/j.jhin.2009.04.020. Epub 2009 Aug 21 [PubMed PMID: 19699552]
Mulcahy LR, Isabella VM, Lewis K. Pseudomonas aeruginosa biofilms in disease. Microbial ecology. 2014 Jul:68(1):1-12. doi: 10.1007/s00248-013-0297-x. Epub 2013 Oct 6 [PubMed PMID: 24096885]
Level 3 (low-level) evidencePang Z, Raudonis R, Glick BR, Lin TJ, Cheng Z. Antibiotic resistance in Pseudomonas aeruginosa: mechanisms and alternative therapeutic strategies. Biotechnology advances. 2019 Jan-Feb:37(1):177-192. doi: 10.1016/j.biotechadv.2018.11.013. Epub 2018 Nov 27 [PubMed PMID: 30500353]
Level 3 (low-level) evidenceZacherle BJ, Silver DS. Hot tub folliculitis: a clinical syndrome. The Western journal of medicine. 1982 Sep:137(3):191-4 [PubMed PMID: 7147933]
Level 3 (low-level) evidenceNiall DM, Murphy PG, Fogarty EE, Dowling FE, Moore DP. Puncture wound related pseudomonas infections of the foot in children. Irish journal of medical science. 1997 Apr-Jun:166(2):98-101 [PubMed PMID: 9159992]
Lund-Palau H, Turnbull AR, Bush A, Bardin E, Cameron L, Soren O, Wierre-Gore N, Alton EW, Bundy JG, Connett G, Faust SN, Filloux A, Freemont P, Jones A, Khoo V, Morales S, Murphy R, Pabary R, Simbo A, Schelenz S, Takats Z, Webb J, Williams HD, Davies JC. Pseudomonas aeruginosa infection in cystic fibrosis: pathophysiological mechanisms and therapeutic approaches. Expert review of respiratory medicine. 2016 Jun:10(6):685-97. doi: 10.1080/17476348.2016.1177460. Epub 2016 May 13 [PubMed PMID: 27175979]
Azzopardi EA, Azzopardi SM, Boyce DE, Dickson WA. Emerging gram-negative infections in burn wounds. Journal of burn care & research : official publication of the American Burn Association. 2011 Sep-Oct:32(5):570-6. doi: 10.1097/BCR.0b013e31822ac7e6. Epub [PubMed PMID: 21792068]
Slattery WH 3rd, Brackmann DE. Skull base osteomyelitis. Malignant external otitis. Otolaryngologic clinics of North America. 1996 Oct:29(5):795-806 [PubMed PMID: 8893217]
Makhnevich A, Feldhamer KH, Kast CL, Sinvani L. Aspiration Pneumonia in Older Adults. Journal of hospital medicine. 2019 Jul 1:14(7):429-435. doi: 10.12788/jhm.3154. Epub 2019 Feb 20 [PubMed PMID: 30794136]
Rivera-Sanchez R, Delgado-Ochoa D, Flores-Paz RR, García-Jiménez EE, Espinosa-Hernández R, Bazan-Borges AA, Arriaga-Alba M. Prospective study of urinary tract infection surveillance after kidney transplantation. BMC infectious diseases. 2010 Aug 19:10():245. doi: 10.1186/1471-2334-10-245. Epub 2010 Aug 19 [PubMed PMID: 20723254]
Bodey GP, Bolivar R, Fainstein V, Jadeja L. Infections caused by Pseudomonas aeruginosa. Reviews of infectious diseases. 1983 Mar-Apr:5(2):279-313 [PubMed PMID: 6405475]
Level 3 (low-level) evidenceAngeletti S, Cella E, Prosperi M, Spoto S, Fogolari M, De Florio L, Antonelli F, Dedej E, De Flora C, Ferraro E, Incalzi RA, Coppola R, Dicuonzo G, Francescato F, Pascarella S, Ciccozzi M. Multi-drug resistant Pseudomonas aeruginosa nosocomial strains: Molecular epidemiology and evolution. Microbial pathogenesis. 2018 Oct:123():233-241. doi: 10.1016/j.micpath.2018.07.020. Epub 2018 Jul 19 [PubMed PMID: 30031889]