Introduction
Intracranial hemorrhage encompasses 4 broad types of hemorrhage[1][2][3]:
- Epidural hemorrhage
- Subdural hemorrhage
- Subarachnoid hemorrhage (SAH)
- Intraparenchymal hemorrhage: A hemorrhage involving the cerebral hemispheres.
The first two are called extra-axial hemorrhage, and the latter are intra-axial. Each type of hemorrhage differs concerning etiology, findings, prognosis, and outcome. This article provides a broad overview of the types of intracranial hemorrhage.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Epidural Hemorrhage
An epidural hematoma is arterial or venous in origin. The classical arterial epidural hematoma occurs after blunt trauma to the head, typically the temporal region. This type of bleeding may also occur after a penetrating head injury. Typically, a skull fracture with damage to the middle meningeal artery causes arterial bleeding into the potential epidural space. Although the middle meningeal artery is classically described, any meningeal artery can lead to arterial epidural hematoma.[4]
A venous epidural hematoma occurs after a skull fracture, and the venous bleeding from the skull fracture fills the epidural space. Venous epidural hematomas are common in pediatric patients.
Subdural Hemorrhage
Subdural hemorrhage occurs when blood enters the subdural space, which is anatomically the arachnoid space. Commonly, subdural hemorrhage occurs after a vessel traversing between the brain and skull is stretched, broken, or torn and begins to bleed into the subdural space. These most commonly occur after a blunt head injury but may also occur after penetrating head injuries or spontaneously.[5][6]
Subarachnoid Hemorrhage
A subarachnoid hemorrhage refers to bleeding into the subarachnoid space. Subarachnoid hemorrhage is divided into traumatic versus non-traumatic subarachnoid hemorrhage. A second categorization divides subarachnoid hemorrhage into an aneurysmal and non-aneurysmal subarachnoid hemorrhage. Aneurysmal subarachnoid hemorrhage occurs after the rupture of a cerebral aneurysm. Non-aneurysmal subarachnoid hemorrhage is bleeding into the subarachnoid space without identifiable aneurysms. Non-aneurysmal subarachnoid bleeding most commonly occurs after trauma with a blunt head injury with or without penetrating trauma or sudden acceleration changes to the head.[7]
Intraparenchymal Hemorrhage
Intraparenchymal hemorrhage is bleeding into the brain parenchyma. A wide variety of reasons cause hemorrhage, including, but not limited to, hypertension, arteriovenous malformation (AVM), amyloid angiopathy, aneurysm rupture, tumor, coagulopathy, infection, vasculitis, and trauma.
Epidemiology
Epidural Hemorrhage
Epidural hematomas are present in approximately 2% of head injury patients and account for 5% to 15% of fatal head injuries. Approximately 85% to 95% of epidural hematomas have an overlying skull fracture. 3.1 million people worldwide require surgery for traumatic epidural hemorrhage every year.[8]
Subdural Hemorrhage
The incidence of subdural hematoma is estimated to be between 5% and 25% of patients with a significant head injury. It is present in an annual incidence of 1 to 5 cases per 100,000 per year, with a male-to-female ratio of 2:1. The incidence of subdural hematomas increases throughout life.
Subarachnoid Hemorrhage
Subarachnoid hemorrhage accounts for approximately 5% of all strokes and has an incidence of approximately 2 to 25 per 100,000 person-years for those over the age of 35. The incidence trends slowly as patients age and may be more frequent in females than males (1.15:1 for the female-to-male ratio).
Intraparenchymal Hemorrhage
Intraparenchymal hemorrhage accounts for 10% to 20% of all strokes. Intraparenchymal hemorrhage incidence increases for those aged 55 and older, with an increasing incidence as age increases. Some controversy exists regarding gender differences, with a slight male predominance.
Pathophysiology
Epidural Hemorrhage
Epidural hematomas occur when blood dissects into the potential space between the dura and the inner table of the skull. Most commonly, this happens after a skull fracture (85% to 95% of cases). Damage to an arterial or venous vessel may occur, which causes blood to dissect into the potential epidural space, resulting in the epidural hematoma. The most commonly damaged vessel is the middle meningeal artery underlying the temporoparietal region of the skull.
Subdural Hemorrhage
Subdural hematoma has multiple causes, including head trauma, coagulopathy, vascular abnormality rupture, and spontaneous. Most commonly, head trauma causes motion of the brain relative to the skull, which can stretch and break blood vessels traversing from the brain to the skull. If the blood vessels are damaged, they bleed into the subdural space. Chronic subdural hematoma usually results secondary to trauma that results in bleeding from bridging veins. Subsequent neovascularization and leaking from the outer membrane result in the expansion of the hematoma.
Subarachnoid Hemorrhage
Subarachnoid hemorrhage most commonly occurs after trauma, where cortical surface vessels are injured and bleed into the subarachnoid space. Non-traumatic subarachnoid hemorrhage is most commonly due to the rupture of a cerebral aneurysm. When an aneurysm ruptures, blood can flow into the subarachnoid space. Other causes of subarachnoid hemorrhage include AVM, use of blood thinners, trauma, or idiopathic causes.
Intraparenchymal Hemorrhage
Non-traumatic intraparenchymal hemorrhage often occurs secondary to hypertensive damage to cerebral blood vessels, which eventually burst and bleed into the brain. Other causes include rupture of an AVM, rupture of an aneurysm, arteriopathy, tumor, infection, or venous outflow obstruction. Penetrating and non-penetrating trauma may also cause intraparenchymal hemorrhage. The most common location of a spontaneous intracerebral hemorrhage (ICH) is the putamen, which is usually associated with uncontrolled hypertension.[9]
History and Physical
Epidural Hemorrhage
Patients with epidural hematoma report a history of a focal head injury, such as blunt trauma from a hammer or baseball bat, fall, or MVC. The classic presentation of an epidural hematoma is a loss of consciousness after the injury, followed by a lucid interval and then neurologic deterioration. This classic presentation occurs only in less than 20% of patients. Other common symptoms include severe headache, nausea, vomiting, lethargy, and seizure.
Subdural Hemorrhage
A history of either major or minor head injury can be found in cases of subdural hematoma. In older patients, a subdural hematoma can occur after trivial head injuries, including bumping of the head on a cabinet or running into a door or wall. An acute subdural can present with recent trauma, headache, nausea, vomiting, altered mental status, seizure, and/or lethargy. A chronic subdural hematoma can present with a headache, nausea, vomiting, confusion, decreased consciousness, lethargy, motor deficits, aphasia, seizure, or personality changes. A physical exam may demonstrate a focal motor deficit, neurologic deficits, lethargy, or altered consciousness.
Subarachnoid Hemorrhage
A thunderclap headache (sudden severe or worst headache of life) is the classic presentation of subarachnoid hemorrhage. Other symptoms include dizziness, nausea, vomiting, diplopia, seizures, loss of consciousness, or nuchal rigidity. Physical exam findings may include focal neurologic deficits, cranial nerve palsies, nuchal rigidity, or decreased or altered consciousness.
Intraparenchymal Hemorrhage
Non-traumatic intraparenchymal hemorrhages typically present with a history of sudden onset of stroke symptoms, including a headache, nausea, vomiting, focal neurologic deficits, lethargy, weakness, slurred speech, syncope, vertigo, or changes in sensation.
Evaluation
The initial evaluation, which encompasses a primary survey, prioritizes assessing the airway, breathing, and circulation. In addition, a comprehensive neurological examination is warranted to assess for focal neurological deficits.
Glasgow Coma Scale Score [10]
The Glasgow Coma Scale (GCS) helps quickly rate the severity of a patient's neurologic injury. The 3 components of this score are:
- Eye-opening (ranging from 1 to 4)
- Best verbal response (ranging from 1 to 5)
- Best motor response (ranging from 1 to 6)
TBI can be classified based on GCS as mild (13 to 15), moderate (9 to 12), and severe (8 or less).
Laboratory Studies
- Complete blood count to check for thrombocytopenia
- Coagulation studies (PTT, PT/INR) for coagulopathy
- A basic metabolic panel for electrolyte abnormalities
Imaging
A non-contrast computed tomography (CT) scan of the head is the imaging modality unless additional modalities are indicated for further evaluation.
Epidural Hemorrhage [11][12][13]
If intracranial pressure (ICP) increases, a Cushing response (hypertension, bradycardia, and bradypnea) may occur as compensation. The characteristic imaging finding is a hyperdense extra-axial lens-shaped (biconvex) opacity. Historically, cerebral angiography could locate the shift in cerebral blood vessels, but cerebral angiography is supplanted by CT imaging.
Subdural Hemorrhage
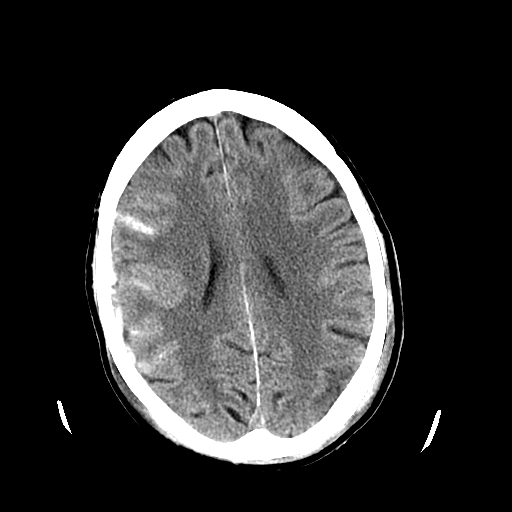
An acute subdural hematoma is typically hyperdense, while a chronic subdural is hypodense. A subacute subdural may be isodense to the brain and more challenging to identify (see Image. Subdural Hematoma Detected on Head CT).
Subarachnoid Hemorrhage
Patients with subarachnoid hemorrhage can rapidly deteriorate and may need emergent intubation. If the patient is given contrast during imaging, this may obscure the subarachnoid hemorrhage. Acute subarachnoid hemorrhage is typically hyperdense on CT imaging (see Image. Head CT Revealing Subarachnoid Hemorrhage). If the CT scan is negative and a strong suspicion of subarachnoid hemorrhage exists, a lumbar puncture (LP) should be considered. The LP results may show xanthochromia. An LP performed before 6 hours of the subarachnoid hemorrhage may fail to show xanthochromia. Additionally, LP results may be confounded if a traumatic tap is encountered.
Identifying the cause of non-traumatic subarachnoid hemorrhage helps guide further treatment. Standard workup includes either a CT angiogram (CTA) of the head and neck, magnetic resonance angiography (MRA) of the head and neck, or diagnostic cerebral angiogram of the head and neck to look for an aneurysm, AVM, or another source of subarachnoid hemorrhage.
Intraparenchymal Hemorrhage
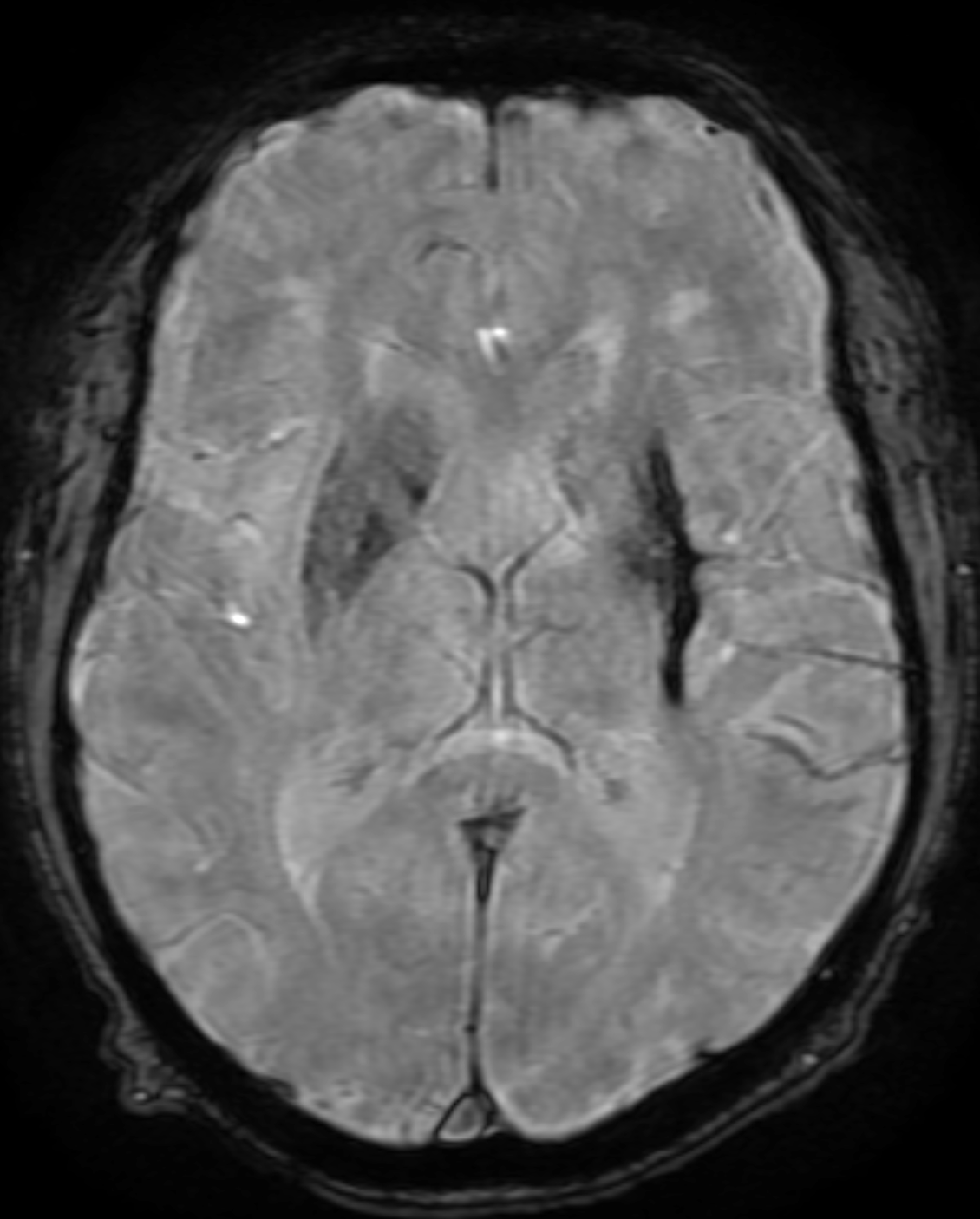
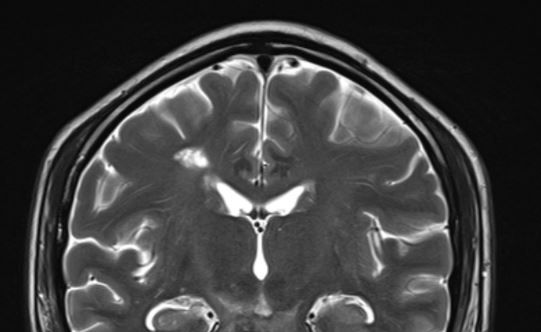
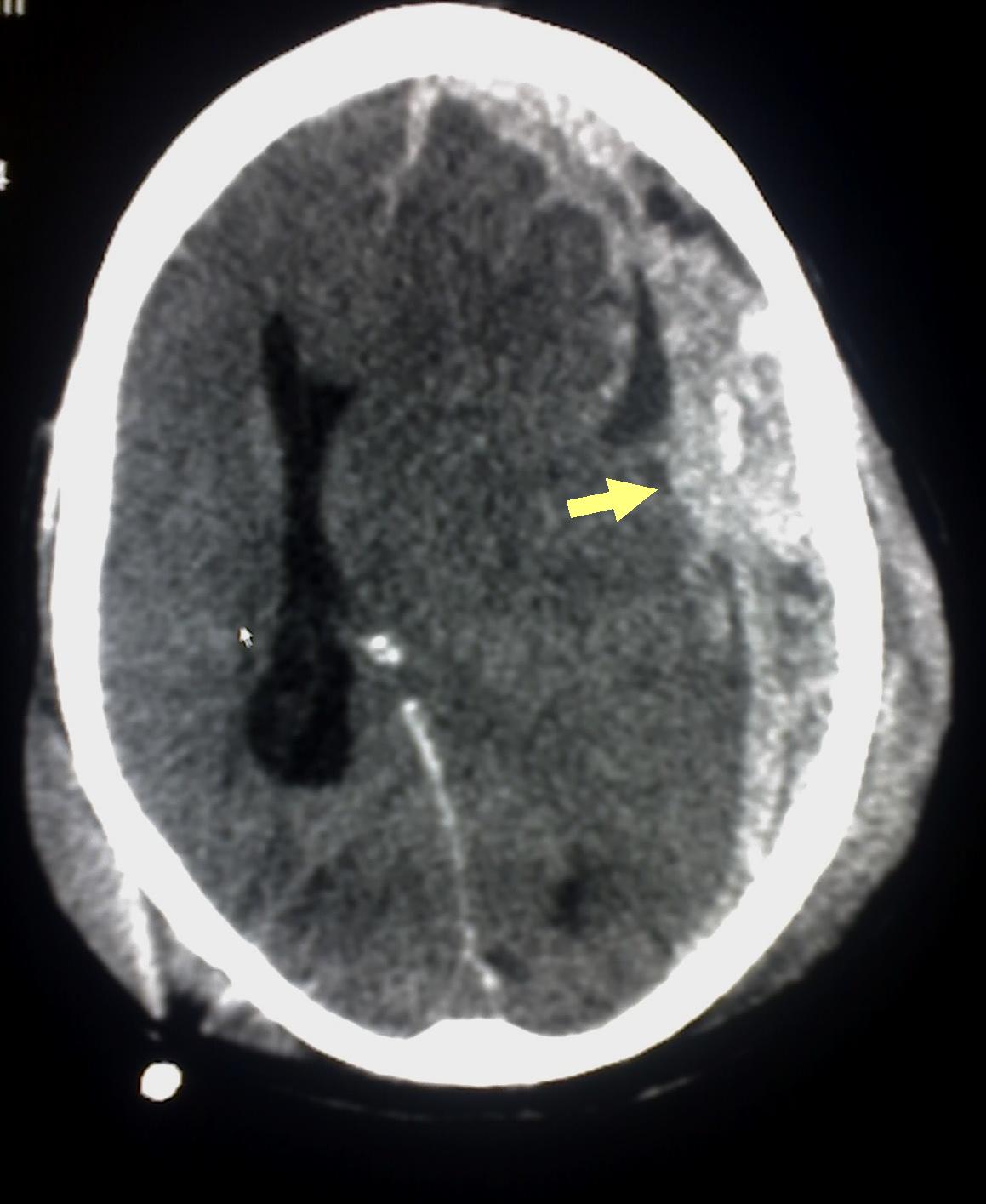
The imaging should be able to identify acute intraparenchymal hemorrhage as a hyperdensity within the parenchyma. Depending on the history and physical and imaging findings, a magnetic resonance imaging (MRI) scan of the brain with and without contrast should be considered. Head CT can also identify intraparenchymal hemorrhage (see Image. Intracerebral Hemorrhage with Intraventricular Bleeding) within specific regions (see Image. Intracranial Hemorrhage in the Caudate Region).
Other imaging to consider include CTA, MRA, or diagnostic cerebral angiogram to look for cerebrovascular causes of the intraparenchymal hemorrhage. Diagnostic cerebral angiography is indicated for all patients with ICH except those aged more than 45 with preexisting hypertension in thalamic, putaminal, or posterior fossa hemorrhage.[14] Cavernomas are angiographically occult and can be picked up incidentally or present with small parenchymal hemorrhage resulting in headaches, neurological deficits, or seizures. They have a characteristic "popcorn" or "berry" appearance on MRI scans with a rim of signal loss due to haemosiderin (see Image. Popcorn-Like Appearance of a Cavernoma).
Different intensities of blood products in different sequences of MRI scans[15]:
-
Hyperacute (<12 hours)
T1 Isointense T2 hyperintense Gradient echo - hypointense rim
-
Acute (12 hours to 2 days)
T1 IsointenseT2 hypointenseGradient echo - a hypointense rim that gradually progresses to the center
-
Early subacute (2 to 7 days)
T1 hyperintenseT2 hypointenseGradient echo - hypointense
-
Late subacute (8 days to 1 month)
T1 hyperintenseT2 hyperintenseGradient echo - hyperintense with rim of low-intensity
-
Chronic (>1 month)
T1 hypointenseT2 hypointenseGradient echo - slit-like hyperintense or isointense core surrounded by a hypointense rim
The most common type of intracranial hemorrhage in neonates is germinal matrix hemorrhage or periventricular-intraventricular hemorrhage (PVIH). PVIH is classified into the following grades (Papile):[16]
-
Grade I: Restricted to subependymal region/germinal matrix seen in the caudothalamic groove
-
Grade II: Extending into normal-sized ventricles and typically filling <50% of the ventricular volume
-
Grade III: Extensive hemorrhage with distension/dilation of the ventricles
-
Grade IV: Parenchymal involvement - has the highest mortality
Other
Asymptomatic striatocapsular slit-like hemorrhage has been studied as a severity marker in patients with hypertensive angiopathy (see Image. Chronic Hypertensive Hemorrhage).[17]
Remote cerebellar hemorrhage (RCH) typically occurs after supratentorial craniotomy and is less likely after spinal surgery. RCH occurs remotely near the surgical site and without an underlying pathologic lesion.[18]
Treatment / Management
Immediate neurosurgical consultation is recommended for all hemorrhages, but mainly if alarming signs such as airway compromise, respiratory failure, or hemodynamic instability exist.
Epidural Hemorrhage [19][20][21](A1)
Definitive treatment is an evacuation of the hematoma and stopping the bleeding source. Some smaller epidural hematomas may be managed non-surgically and monitored for resolution.
Conservative management is attempted if the patient satisfies all of the following criteria and has mild symptoms[22]:
- Epidural hematoma volume of less than 30 mL
- A clot diameter of less than 15 mm
- Midline shift of less than 5 mm
- GCS greater than 8 and, on physical examination, shows no focal neurological symptoms.
Subdural Hemorrhage
Definitive treatment is an evacuation, but depending on the size and location, some subdural hematomas may be monitored for resolution. Non-surgical management options include repeat imaging to ensure subdural stability, anticoagulation reversal, platelet transfusions for thrombocytopenia or dysfunctional platelets, observation with frequent neurologic assessments for deterioration, and/or controlling hypertension. The use of steroids is still controversial.
Surgical management options include a twist drill hole, burr hole(s), and craniotomy for evacuation. Data suggests that a twist drill hole has the lowest surgical complication rate with the highest recurrence rate. A craniotomy has the highest surgical complication rate with the lowest recurrence rate of the surgical options, and burr hole(s) evacuation falls somewhere between a twist drill hole and a craniotomy for complication and recurrence rate.
Subarachnoid Hemorrhage
If the patient is on anticoagulation or antiplatelet agents, reversal is prioritized. Management is typically conservative with close assessments of vitals and neurologic status. In obtunded patients, a need for ICP monitoring and/or external ventricular drain (EVD) is common. Patients should be monitored for hydrocephalus or cerebral swelling. Repeat imaging can verify the improvement of the traumatic subarachnoid hemorrhage. Sometimes, aneurysmal rupture or incompetence of other intracranial vascular malformations can masquerade as traumatic subarachnoid hemorrhage. If no history of trauma is evident, then a non-traumatic etiology is considered.
In non-traumatic subarachnoid hemorrhage, the next steps vary depending on the etiology of the bleeding but can include treatment of an aneurysm, AVM, or other underlying pathology. Additionally, a low threshold for an EVD exists due to the risk of hydrocephalus.
Intraparenchymal Hemorrhage
Blood pressure should be monitored to decrease the risk of further hemorrhage. The treatment depends on the etiology of the hemorrhage. Treatment options are variable and include aggressive surgical evacuation, craniectomy, catheter-based dissolution, or observation. Surgical evacuation is controversial for some forms of intraparenchymal hemorrhage.
Although many intraparenchymal hemorrhages are secondary to cerebrovascular disease and hypertension, the surgeon should anticipate encountering underlying pathology, including an aneurysm, AVM, and/or tumor, when evacuating an intraparenchymal hemorrhage. Surgical evacuation is usually recommended for cerebellar hematomas larger than 3 cm in diameter[23], and an EVD is placed before the evacuation if hydrocephalus is evident.
Sometimes, evacuating the hematoma may be more detrimental than the hematoma itself, and a craniectomy is performed to promote cerebral swelling. Several catheter-based systems can dissolve the hemorrhage. Minor and non-operable hemorrhages may be non-surgically managed with blood pressure control, the reversal of anticoagulation or antiplatelet agents, and neuroprotective strategies to prevent and/or mitigate secondary cerebral injury.
The indications for surgical resection in cavernomas include:[24]
- Multiple hemorrhages in eloquent areas, or
- Single hemorrhage in a non-eloquent area associated with deteriorating neurological deficits
- Severe symptoms, such as cardiac or respiratory instability, and
- Cavernomas within 2 mm from the pial surface
Differential Diagnosis
The differential diagnoses of intracranial hemorrhage include:
- Infection: Subdural empyema may mimic a subdural hemorrhage
- Recent contrast administration
- Subdural hygroma: May appear similar to chronic subdural hemorrhage
- Tumors: Meningioma may mimic an extradural hemorrhage
Prognosis
The prognosis depends on several factors, including the age of the patient, comorbidities, consumption of antiplatelets or anticoagulants, Glasgow coma scale score at presentation, size of pupils at presentation, location of the bleed, presence of other injuries, and time delay for surgical intervention, if needed.
The ICH score is clinically significant for ICHs.
The ICH Score is the sum of individual points assigned as follows:[25]
- GCS score:
- 3 to 4=2 points
- 5 to 12=1 point
- 13 to 15=0 point
- Age 80 or older:
- Yes=1 point
- No=0 point
- Infratentorial origin:
- Yes=1 point
- No=0 point
- ICH volume:
- ≥30 cm3 =1 point
- <30 cm3 =0 point
- Intraventricular hemorrhage:
- Yes=1 point
- No=0 point
The mortality rate is calculated based on the ICH score as follows:
- 0 points: 0%
- 1 point: 13%
- 2 points: 26%
- 3 points: 72%
- 4 points: 97%
- 5 points: 100%
- 6 points: 100% (estimated)
Complications
The main complications associated with intracranial hemorrhage include neurological deficits, brain herniation, infarcts, rebleeds, vasospasm, seizures, and death.
Deterrence and Patient Education
Patients should be educated on the importance of rehabilitation and medication compliance during recovery. They cannot drive unless cleared.
Enhancing Healthcare Team Outcomes
Patients presenting with bleeding in the central nervous system are optimally treated by an interprofessional healthcare team comprising a neurologist, neurosurgeon, radiologist, intensivist, neurosurgery nurses, physical therapist, pulmonologist, and various allied health specialists such as speech, occupational, and physical therapists. Admission to the intensive care unit (ICU) is often necessary for many of these patients, and their care is tailored based on the severity of physical and neurological deficits. Factors including the type and extent of the bleed, patient age, comorbidities, and the severity of neurological deficits upon admission influence prognosis.[26][7][27]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
Subdural Hematoma Detected on Head CT. Abusive head trauma or shaken baby syndrome may cause subdural hematoma (arrow), indicating bleeding between the dura mater of the meninges and the brain, as detected on the head CT of a patient.
Glitzy queen00, (Public Domain), via Wikimedia Commons.
(Click Image to Enlarge)
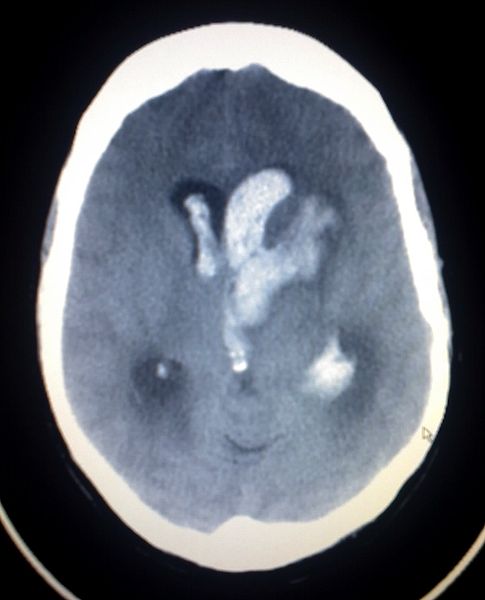
Intracerebral Hemorrhage With Intraventricular Bleeding. Intracerebral hemorrhage is observed with intraventricular bleeding on the head CT of a patient.
Glitzy queen00, Public Domain, via Wikimedia Commons.
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Kohli R, Chaturvedi S. Epidemiology and Clinical Manifestations of Immune Thrombocytopenia. Hamostaseologie. 2019 Aug:39(3):238-249. doi: 10.1055/s-0039-1683416. Epub 2019 Mar 13 [PubMed PMID: 30868551]
Chen SH, McCarthy DJ, Sheinberg D, Hanel R, Sur S, Jabbour P, Atallah E, Chalouhi N, Dumont A, Amenta P, Hasan D, Raper D, Liu K, Jane JA Jr, Crowley RW, Aguilar-Salinas P, Bentley J, Monteith S, Mitchell BD, Yavagal DR, Peterson EC, Starke RM. Pipeline Embolization Device for the Treatment of Intracranial Pseudoaneurysms. World neurosurgery. 2019 Jul:127():e86-e93. doi: 10.1016/j.wneu.2019.02.135. Epub 2019 Mar 6 [PubMed PMID: 30849553]
Best JG, Bell R, Haque M, Chandratheva A, Werring DJ. Atrial fibrillation and stroke: a practical guide. Practical neurology. 2019 Jun:19(3):208-224. doi: 10.1136/practneurol-2018-002089. Epub 2019 Mar 2 [PubMed PMID: 30826740]
Babu JM, Patel SA, Palumbo MA, Daniels AH. Spinal Emergencies in Primary Care Practice. The American journal of medicine. 2019 Mar:132(3):300-306. doi: 10.1016/j.amjmed.2018.09.022. Epub 2018 Oct 3 [PubMed PMID: 30291829]
Kanematsu R, Hanakita J, Takahashi T, Park S, Minami M. Radiologic Features and Clinical Course of Chronic Spinal Epidural Hematoma: Report of 4 Cases and Literature Review. World neurosurgery. 2018 Dec:120():82-89. doi: 10.1016/j.wneu.2018.08.058. Epub 2018 Aug 23 [PubMed PMID: 30145384]
Level 3 (low-level) evidenceJoubert C, Gazzola S, Sellier A, Dagain A. Acute idiopathic spinal subdural hematoma: What to do in an emergency? Neuro-Chirurgie. 2019 Apr-Jun:65(2-3):93-97. doi: 10.1016/j.neuchi.2018.10.009. Epub 2019 Feb 8 [PubMed PMID: 30744959]
Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Nakaji P, Karis JP, Wallace RC. Ten-year analysis of saccular aneurysms in the Barrow Ruptured Aneurysm Trial. Journal of neurosurgery. 2020 Mar 1:132(3):771-776. doi: 10.3171/2018.8.JNS181846. Epub 2019 Mar 8 [PubMed PMID: 30849758]
Rahimi A, Corley JA, Ammar A, Shlobin NA, Rolle M, Mekary RA, Park KB. The unmet global burden of cranial epidural hematomas: A systematic review and meta-analysis. Clinical neurology and neurosurgery. 2022 Aug:219():107313. doi: 10.1016/j.clineuro.2022.107313. Epub 2022 Jun 6 [PubMed PMID: 35688003]
Level 1 (high-level) evidenceAn SJ, Kim TJ, Yoon BW. Epidemiology, Risk Factors, and Clinical Features of Intracerebral Hemorrhage: An Update. Journal of stroke. 2017 Jan:19(1):3-10. doi: 10.5853/jos.2016.00864. Epub 2017 Jan 31 [PubMed PMID: 28178408]
Jain S, Iverson LM. Glasgow Coma Scale. StatPearls. 2024 Jan:(): [PubMed PMID: 30020670]
Marcia L, Moazzez A, Plurad DS, Putnam B, Kim DY. Utility of Repeat Head CT in Patients on Preinjury Antithrombotic Medications. The American surgeon. 2018 Oct 1:84(10):1626-1629 [PubMed PMID: 30747683]
Song K, Guan M, Li W, Jing Z, Xie X, Shi C, Liang J, Qiao H, Huang L. Acute ischemic stroke patients with diffusion-weighted imaging-Alberta Stroke Program Early Computed Tomography Score ≤ 5 can benefit from endovascular treatment: a single-center experience and literature review. Neuroradiology. 2019 Apr:61(4):451-459. doi: 10.1007/s00234-019-02177-1. Epub 2019 Feb 6 [PubMed PMID: 30725121]
Level 2 (mid-level) evidenceEtminan N, Chang HS, Hackenberg K, de Rooij NK, Vergouwen MDI, Rinkel GJE, Algra A. Worldwide Incidence of Aneurysmal Subarachnoid Hemorrhage According to Region, Time Period, Blood Pressure, and Smoking Prevalence in the Population: A Systematic Review and Meta-analysis. JAMA neurology. 2019 May 1:76(5):588-597. doi: 10.1001/jamaneurol.2019.0006. Epub [PubMed PMID: 30659573]
Level 1 (high-level) evidenceZhu XL, Chan MS, Poon WS. Spontaneous intracranial hemorrhage: which patients need diagnostic cerebral angiography? A prospective study of 206 cases and review of the literature. Stroke. 1997 Jul:28(7):1406-9 [PubMed PMID: 9227692]
Level 3 (low-level) evidenceSiddiqui FM, Bekker SV, Qureshi AI. Neuroimaging of hemorrhage and vascular defects. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 2011 Jan:8(1):28-38. doi: 10.1007/s13311-010-0009-x. Epub [PubMed PMID: 21274683]
Starr R, De Jesus O, Shah SD, Borger J. Periventricular and Intraventricular Hemorrhage. StatPearls. 2025 Jan:(): [PubMed PMID: 30855894]
Tsai HH, Lee BC, Huang CY, Tsai LK, Tang SC, Jeng JS, Chen YF. Asymptomatic Striatocapsular slit-like Hemorrhage as a Severity Marker in Patients with Hypertensive Angiopathy. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2020 Oct:29(10):105153. doi: 10.1016/j.jstrokecerebrovasdis.2020.105153. Epub 2020 Jul 29 [PubMed PMID: 32912549]
Omer A, Engelman E, Bath K, Krauthamer AV, Pisinski L. Remote cerebellar hemorrhage: A case report. Radiology case reports. 2019 Mar:14(3):385-389. doi: 10.1016/j.radcr.2018.12.006. Epub 2019 Jan 3 [PubMed PMID: 30766645]
Level 3 (low-level) evidenceAcciarresi M, Altavilla R, Mosconi MG, Caso V. Management of intracranial haemorrhage, unruptured aneurysms and arteriovenous malformations during and after pregnancy. Current opinion in neurology. 2019 Feb:32(1):36-42. doi: 10.1097/WCO.0000000000000643. Epub [PubMed PMID: 30516646]
Level 3 (low-level) evidencePhillips SS, Mueller CM, Nogueira RG, Khalifa YM. A Systematic Review Assessing the Current State of Automated Pupillometry in the NeuroICU. Neurocritical care. 2019 Aug:31(1):142-161. doi: 10.1007/s12028-018-0645-2. Epub [PubMed PMID: 30484008]
Level 1 (high-level) evidenceMuskens IS, Hertgers O, Lycklama À Nijeholt GJ, Broekman MLD, Moojen WA. Outcomes of Retreatment for Intracranial Aneurysms - A Meta-Analysis. Neurosurgery. 2019 Dec 1:85(6):750-761. doi: 10.1093/neuros/nyy455. Epub [PubMed PMID: 30445544]
Level 1 (high-level) evidenceKhairat A, Waseem M. Epidural Hematoma. StatPearls. 2025 Jan:(): [PubMed PMID: 30085524]
Li L, Li Z, Li Y, Su R, Wang B, Gao L, Yang Y, Xu F, Zhang X, Tian Q, Zhang X, Guo Q, Chang T, Luo T, Qu Y. Surgical Evacuation of Spontaneous Cerebellar Hemorrhage: Comparison of Safety and Efficacy of Suboccipital Craniotomy, Stereotactic Aspiration, and Thrombolysis and Endoscopic Surgery. World neurosurgery. 2018 Sep:117():e90-e98. doi: 10.1016/j.wneu.2018.05.170. Epub 2018 Jun 1 [PubMed PMID: 29864571]
Mouchtouris N, Chalouhi N, Chitale A, Starke RM, Tjoumakaris SI, Rosenwasser RH, Jabbour PM. Management of cerebral cavernous malformations: from diagnosis to treatment. TheScientificWorldJournal. 2015:2015():808314. doi: 10.1155/2015/808314. Epub 2015 Jan 5 [PubMed PMID: 25629087]
Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001 Apr:32(4):891-7 [PubMed PMID: 11283388]
Level 2 (mid-level) evidenceYi HJ, Sung JH, Lee MH, Lee DH. Experience of the New FlowGate(2) Device as a Balloon Guide Catheter for Ischemic Stroke Intervention. World neurosurgery. 2019 Jun:126():e736-e742. doi: 10.1016/j.wneu.2019.02.140. Epub 2019 Mar 6 [PubMed PMID: 30851472]
Kim CH, Kim SE, Jeon JP. Meta-Analysis of Endovascular Treatment for Acute M2 Occlusion. Journal of Korean Neurosurgical Society. 2019 Mar:62(2):193-200. doi: 10.3340/jkns.2017.0299. Epub 2019 Feb 27 [PubMed PMID: 30840974]
Level 1 (high-level) evidence