Introduction
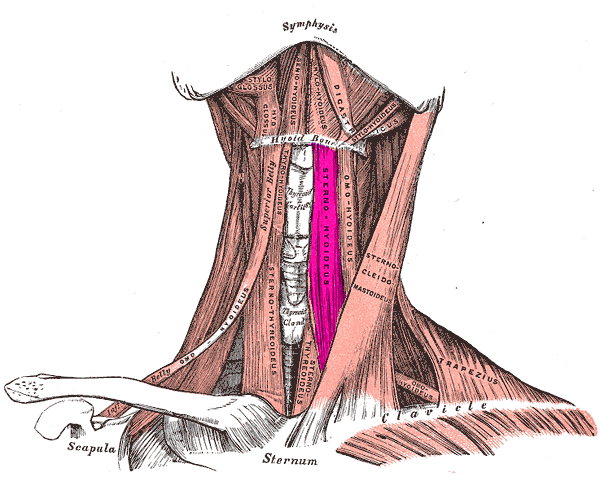
The anterior neck region is made up of many structures that are crucial in maintaining essential functions for life. The skin is the most superficial organ in the neck region, and it functions as a barrier to the underlying structures. The fat in the neck region acts as cushioning for the surrounding structures. As for the anterior neck muscles, they manifest movements to the head and neck. The muscles in the anterior neck region can further separate into the suprahyoid muscles and the infrahyoid muscles. The hyoid bone demarcates these muscles into a superior group and an inferior group. Contraction of the suprahyoid muscles will elevate the hyoid bone while contraction of the infrahyoid muscles will depress the hyoid bone. These muscles contract in the different phases of speaking, chewing, and swallowing. But both the suprahyoid muscles and the infrahyoid muscles also act as a barrier to protect the trachea, thyroid gland, and the esophagus.
One of the muscles grouped into the infrahyoid muscles is the sternohyoid muscle. The first root word of sternohyoid is "sterno," this equates to the sternum while the last root word is "hyoid," which references the hyoid bone. The simplicity of the name of this muscle is that its name explains the regions that it originates from and to which it attaches. As for the actions of the sternohyoid muscle, it contributes to the depression of the hyoid bone.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
In the neck region, there is a group of muscles located inferior to the hyoid bone called the infrahyoid muscles. This group of muscles contains the omohyoid muscle, the sternohyoid muscle, the sternothyroid muscle, and the thyrohyoid muscle. Due to the origins and attachments of the infrahyoid muscles, they function to depress the hyoid bone when they contract. This group of muscles also contribute to the protection of the trachea, esophagus, blood vessels, and thyroid gland.
As for the sternohyoid muscle, it is a flat muscle located on both sides of the neck. This muscle originated from the medial edge of the clavicle bone, sternoclavicular ligament, and posterior side of the manubrium. The sternohyoid muscle then ascends the neck and attaches to the body of the hyoid bone. The sternohyoid muscle also has a continuation muscle that attaches the thyroid to the hyoid bone via the thyrohyoid muscle. The primary function of the sternohyoid muscle is to work in sync with the other infrahyoid muscles to depress the hyoid bone. The hyoid bone is depressed during jaw opening for speak, mastication, and swallowing. The sternohyoid muscle also participates as a minor contributor to head motions.[1]
Embryology
Most muscle tissue in the human body derives from the mesenchymal tissue of the mesodermal germ layer. The mesenchymal tissue will differentiate into muscles, blood vessels, and connective tissue. The sternohyoid muscle will form from the mesenchymal tissue in the neck region during fetal development.
Muscle embryology is a process called myogenesis. This process involves the myoblast cells derived from the mesodermal germ layer. These myoblast cells will elongate and fuse to form muscle fibers called myotubes. This induction of this process occurs via fibroblast growth factor (FGF). The myotubes will grow and proliferate until they terminally differentiate into myocytes. The myocytes will be the muscle cell that is present in all types of muscles.
Blood Supply and Lymphatics
The external carotid artery is the vessel that perfuses the structures in the face and neck. The external carotid artery adequately perfumes the head, face, and neck through several arterial branches. One of the branches formed is the superior thyroid artery. After the superior thyroid artery branches from the external carotid artery. It descends towards the thyroid gland. As the superior thyroid artery makes its way to the thyroid gland, it will perfuse the structures with which it comes in contact. One of the structures that the superior thyroid artery passes is the sternohyoid muscle. The sternohyoid muscle will receive its arterial blood supply from the superior thyroid artery.[1][2][3]
The lymphatic drainage of the sternohyoid muscles divides into two separate paths since its a paired muscle. The right sternohyoid muscle will drain lymph fluid into the supraclavicular or cervical lymph nodes while the left sternohyoid muscle drains its lymph into the left supraclavicular or cervical lymph nodes. The right supraclavicular and cervical lymph nodes will then drain the lymph into the right lymphatic duct. The left supraclavicular and cervical lymph nodes will drain the lymph into the thoracic duct. Both the right lymphatic duct and the thoracic duct will drain the lymph back into the central circulation.[4]
Nerves
The nerve innervation to the sternohyoid muscle derives from the first, second, and third cervical nerve roots (C1-C3). These nerve roots form a plexus called the ansa cervicalis. The ansa cervicalis provides motor innervation to the sternohyoid muscle. The ansa cervicalis nerve also innervates the omohyoid muscle, the sternohyoid muscle, and the thyrohyoid muscle.[5]
Muscles
The sternohyoid muscle is a part of a group of muscles called the infrahyoid muscles. This group of muscles contains four main muscles: the omohyoid muscle, the sternohyoid muscle, the sternothyroid muscle, and the thyrohyoid muscle. The primary function of this group of muscles is to depress the hyoid bone during speech and swallowing.
Physiologic Variants
The sternohyoid muscle may vary in size, length, and thickness in different individuals. The origins and attachments of the sternohyoid may also vary slightly. In some cases, the sternohyoid was found to be one muscle instead of a paired muscle. The sternohyoid muscle has also been found to originate from the omohyoid muscle's tendon instead of the sternum. Interestingly, some individuals completely lack the presence of the sternohyoid muscle.
Surgical Considerations
Since the sternohyoid muscle is in the anterior neck region, neck surgery involving the region below the hyoid bone will also involve the sternohyoid muscle. Since the sternothyroid muscle and the other infrahyoid muscles provide a muscular barrier to the trachea, esophagus, thyroid gland, and parathyroid glands.[6] The sternohyoid muscle is retracted or dissected away in laryngectomies, tracheostomies, thyroidectomies, and parathyroidectomies. In thyroid and parathyroid surgeries, the sternohyoid muscle has to be retracted or dissected away. The thyroid and parathyroids are beneath the infrahyoid muscles. The sternohyoid muscle has been used as a muscle flap for reconstructive surgeries also. Using the sternohyoid muscle as a flap for reconstruction in tracheostomies and laryngectomies have shown to improve postoperative outcomes. The sternohyoid muscle flap can transfer to a different region.[7][8][9][10][11]
Clinical Significance
The sternohyoid muscle has implications in pathologies affecting the neck region. It has classically been difficult for health care provides to differentiate the causes of anterior neck pain or swellings. Since the sternohyoid muscle is one of the structures located in the anterior neck region, it could be a possible etiology to neck pain or swelling. In sternohyoid muscle syndrome, there is a mass present in the lateral neck region that disappears with swallowing. Classically this condition is caused by omohyoid muscle syndrome, but research has found that the sternohyoid muscle can also be the cause of the swelling.[12]
Other Issues
The sternohyoid muscle contributes to depression of the hyoid bone in speaking, chewing, and swallowing. If the sternohyoid muscle were to become injured, these mechanisms would become impaired. Also, if the nerve or blood perfusion to the sternohyoid muscle was to be compromised, the sternohyoid and the infrahyoid muscles could atrophy or even undergo necrosis.[13]
The close relationship between the sternohyoid muscle and the thyroid gland makes the sternohyoid muscle a site of possible metastasis in thyroid cancers. If thyroid cancer spreads, it could affect the sternothyroid gland and manifest as a nodule in the muscle.[4]
Media
(Click Image to Enlarge)
References
Mnatsakanian A, Al Khalili Y. Anatomy, Head and Neck, Thyroid Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 31082107]
Sreedharan R, Krishna L, Shetty A. Origin of superior thyroid artery: under the surgeon's knife. Jornal vascular brasileiro. 2018 Oct-Dec:17(4):290-295. doi: 10.1590/1677-5449.004218. Epub [PubMed PMID: 30787946]
Meguid EA, Agawany AE. An anatomical study of the arterial and nerve supply of the infrahyoid muscles. Folia morphologica. 2009 Nov:68(4):233-43 [PubMed PMID: 19950073]
Sun G, Wang Y, Zhu Y, Wang Y, Xu K, Wei W, Li H, Lu Z, Ji Q. Lymph node metastasis between sternocleidomastoid and sternohyoid muscle in clinically node-positive papillary thyroid carcinoma. Head & neck. 2013 Aug:35(8):1168-70. doi: 10.1002/hed.23099. Epub 2012 Aug 28 [PubMed PMID: 22927223]
Level 2 (mid-level) evidencePrades JM, Gavid M, Dubois MD, Dumollard JM, Timoshenko AT, Peoc'h M. Surgical anatomy of the ansa cervicalis nerve: which branch to use for laryngeal reinnervation in humans? Surgical and radiologic anatomy : SRA. 2015 Mar:37(2):139-45. doi: 10.1007/s00276-014-1355-x. Epub 2014 Aug 28 [PubMed PMID: 25165021]
Allen E, Fingeret A. Anatomy, Head and Neck, Thyroid. StatPearls. 2023 Jan:(): [PubMed PMID: 29262169]
Hantzakos A, Evrard AS, Lawson G, Remacle M. Posthemicricoidectomy reconstruction with a composite hyoid-sternohyoid osseomuscular flap: the Rethi-Ward technique. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2007 Nov:264(11):1339-42 [PubMed PMID: 17571274]
Level 3 (low-level) evidenceDong P, Li X, Xie J, Li L, Xu H. Modified frontolateral partial laryngectomy without tracheotomy. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2009 Jul:141(1):70-4. doi: 10.1016/j.otohns.2009.02.007. Epub 2009 Apr 9 [PubMed PMID: 19559961]
Dong P, Li X, Wang G, Chen X, Xie J, Nakashima T. Repair with sternohyoid muscle fascia after subtotal laryngectomy. The Journal of laryngology and otology. Supplement. 2009:(31):18-23. doi: 10.1017/S0022215109005039. Epub [PubMed PMID: 19460199]
Icibaci A, de Mello-Filho FV. Tracheal transplant with a prefabricated microsurgical flap. The Laryngoscope. 2009 Dec:119(12):2309-14. doi: 10.1002/lary.20538. Epub [PubMed PMID: 19768763]
Level 3 (low-level) evidenceAlam DS, Haffey T, Vakharia K, Rajasekaran K, Chi J, Prayson R, McBride J, McClennan G. Sternohyoid flap for facial reanimation: a comprehensive preclinical evaluation of a novel technique. JAMA facial plastic surgery. 2013 Jul-Aug:15(4):305-13. doi: 10.1001/jamafacial.2013.287. Epub [PubMed PMID: 23702665]
Kim JS, Hong KH, Hong YT, Han BH. Sternohyoid muscle syndrome. American journal of otolaryngology. 2015 Mar-Apr:36(2):190-4. doi: 10.1016/j.amjoto.2014.10.028. Epub 2014 Oct 22 [PubMed PMID: 25484367]
Level 3 (low-level) evidenceTecchio SA, de Mello-Filho FV, Martins Mamede RC, Llorach Velludo MA. Time necessary for neovascularization of a tracheal segment by the sternohyoid muscle. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2001 Sep:125(3):201-4 [PubMed PMID: 11555754]
Level 3 (low-level) evidence