Introduction
The systolic performance of the heart is determined by 3 factors: preload, afterload, and contractility. The direct relationship between preload and cardiac output was formulated in the early 1900s based on the work of Otto Frank and Ernest Starling. It led to the well-known Frank-Starling curves. Gordon et al. helped to elucidate the underlying mechanism for this phenomenon in their 1966 experiments involving sarcomere length-tension relationships. During this same period, extensive research demonstrated an inverse relationship between afterload and systolic performance, which is accepted today. This means that cardiac output decreases as the afterload on the heart increases and vice versa. Despite this simple concept, there has been substantial controversy over the best way to represent cardiac afterload.
The afterload of any contracting muscle is defined as the total force that opposes sarcomere shortening minus the stretching force that existed before contraction. Applying this definition to the heart, afterload can be most easily described as the "load" against which the heart ejects blood. The load on individual fibers can be expressed as left ventricular wall stress, which is proportional to [(LV Pressure x LV Radius)/ LV wall thickness], or [(P x r)/h]. However, the true equation is complex because it depends on the shape of the cardiac chamber, which is affected by several factors that are changing over time. Therefore, afterload cannot be represented by a single numerical value or described only regarding pressure. Arterial pressure (diastolic, mean, or systolic) is frequently used as a surrogate measure, but perhaps the best available techniques involve measuring systemic arterial resistance by various invasive and noninvasive methods. Several mathematical models have been developed using arterial impedance and pressure-flow relationships to characterize afterload better, but these are complex and less often utilized in practice. The inverse relationship between afterload and cardiac output is important in understanding the pathophysiology and treatment of several diseases, including aortic stenosis, systemic hypertension, and congestive heart failure.[1][2][3]
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
The afterload is the amount of pressure that the heart needs to exert to eject the blood during ventricular contraction. This is recorded as the systolic pressure of the heart. The changes in the afterload affect the stroke volume, end-systolic volume, end-diastolic volume, and left ventricular end-diastolic pressure. Afterload is increased due to an increase in systemic vascular resistance and aortic pressure increase. An increase in the afterload leads to a decrease in the heart's stroke volume and an increase in the end-systolic volume. This also indirectly affects the heart's cardiac output due to a reduction in the stroke volume of the heart. A Frank-Starling curve gives a relationship between stroke volume and left ventricular end-diastolic pressure. The pressure-volume loops explain the effects of afterload on the end-systolic volume and the end-diastolic volume.[4][5]
Mechanism
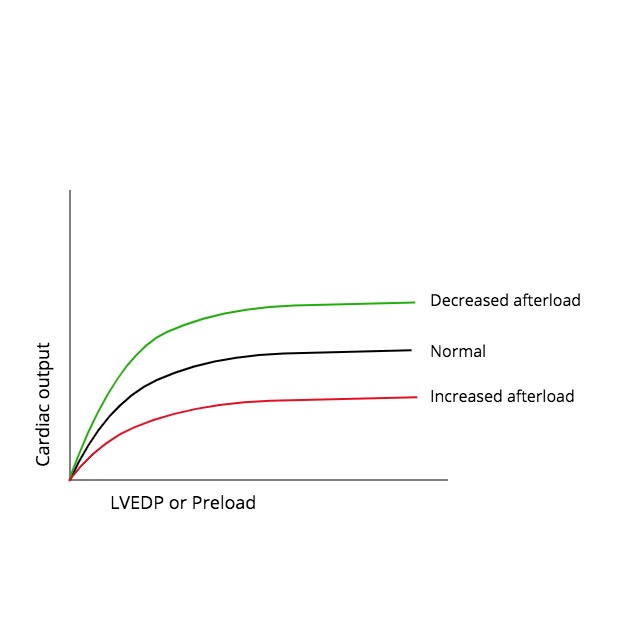
The relationship between afterload and cardiac output is somewhat intuitive as one would expect the flow to increase as the load against which the heart contracts decreases. Several researchers during the 1960s and 1970s sought to develop this understanding at the cellular level. Experiments by Sonnenblick on isolated cat papillary muscle strips demonstrated that the extent and velocity of muscle shortening decrease as the load on the muscle is increased. A major limitation of this study was its basic design employing the use of isolated muscle strips. Monroe and French overcame this by using isolated whole-preparation dog hearts to show an inverse relationship between peak aortic flow and arterial impedance. Ross et al. took this one step further and examined the effects of changing LV afterload in anesthetized dogs by injecting or withdrawing blood from the aorta between systolic contractions. They reported similar findings to the previous studies giving further support for an inverse relationship between afterload and cardiac output due to alterations in sarcomere shortening. Figure 1 is a graphic representation of the effect of increases or decreases in afterload on the cardiac output, which is illustrated by shifting the baseline Frank-Starling curve downward or upward, respectively.[6][7][8]
Clinical Significance
Conditions in which there are chronic elevations in afterload, such as aortic stenosis and systemic hypertension, generate a cascade of adaptive responses, which can be both beneficial and ultimately detrimental. Initially, cardiac output is maintained through various regulatory mediators that increase inotropy. However, the ventricle responds to chronic elevations in afterload by concentric hypertrophy, causing increased wall thickness and decreased chamber diameter. This reduces internal wall stress at the expense of ventricular compliance leading to diastolic dysfunction (heart failure with preserved ejection fraction), which can further deteriorate into systolic dysfunction (heart failure with reduced ejection fraction).[9][10]
Afterload reduction agents are an essential component in treating congestive heart failure with reduced ejection fraction as these patients have elevated systemic resistance due to the neurohormonal response to the decreased cardiac output. They are also frequently used in the management of systemic hypertension. These drugs typically act by dilating the arterial system, which reduces the total load on the contracting heart and increases systolic performance. The arterial dilators fall under the broader category of vasodilators, consisting of arterial, venous, and mixed-acting drugs. Venous dilators reduce preload by pooling blood in the highly compliant venous system and are an important part of treating angina. The preload reducing properties of venodilators lead to a reduction in cardiac output and arterial pressure. Most drugs have mixed arterial and venous action, and the relative balance between these determines the effect on cardiac output.[11]
Several classes of vasodilators are frequently used in practice and deserve a brief mention of their mechanism:
- Ace Inhibitors are one of the first-line medications for managing hypertension and improving mortality in congestive heart failure with reduced ejection fraction. Their exact mechanism in CHF is considered complex, but it is accepted that they inhibit the formation of angiotensin II, which decreases vascular tone and improves systolic function. Ace inhibitors also prevent the formation of aldosterone-mediated by angiotensin II, which decreases preload by reducing sodium and water reabsorption.
- Nitroglycerin, isosorbide dinitrate/ mononitrate, and sodium nitroprusside belong to a subclass of vasodilators known as nitrodilators that work by increasing nitric oxide (NO) within the vascular smooth muscle and play a pivotal role in the management of angina and myocardial infarction. NO activates guanylyl cyclase, leading to cGMP formation, which induces vascular relaxation through several mechanisms: decreasing intracellular calcium, activation of potassium channels inducing hyperpolarization, activation of cGMP dependent protein kinase that activates myosin light chain phosphatase. Nitroglycerin and isosorbide dinitrate/ mononitrate are considered organic nitrates because enzymatic conversion is required to generate nitrogen oxide, and they act primarily on the venous system to reduce preload with limited arterial dilation. Sodium nitroprusside is slightly different in that it releases NO without undergoing enzymatic conversion. It acts primarily on the arterial resistance vessels, which provide useful afterload reducing properties in hypertensive emergency and severe heart failure.[12]
- Hydralazine provides powerful afterload reducing properties and is thought to act solely as an arterial dilator through direct action on the vascular endothelium leading to NO generation. The full mechanism of hydralazine is complex and not completely understood.
- Sympatholytics include alpha one selective (prazosin) and non-selective alpha-blockers (phenoxybenzamine), which are used to manage primary hypertension or hypertensive emergency secondary to pheochromocytoma respectively. Sympatholytics act to reduce afterload by inhibiting the binding of norepinephrine to post-junctional alpha receptors preventing them from causing smooth muscle contraction. The effect is more significant on the arterial system, but they also have some venodilating properties.
- Dihydropyridine calcium channel blockers also affect the peripheral vessels. They act by inhibiting the movement of calcium ions into the vascular smooth muscle cells. This has a vasodilatory effect on the vessels leading to a decrease in the systemic vascular resistance of the heart.[13]
Media
References
Filippatos TD, Liontos A, Papakitsou I, Elisaf MS. SGLT2 inhibitors and cardioprotection: a matter of debate and multiple hypotheses. Postgraduate medicine. 2019 Mar:131(2):82-88. doi: 10.1080/00325481.2019.1581971. Epub [PubMed PMID: 30757937]
Bennett VA, Aya HD, Cecconi M. Evaluation of cardiac function using heart-lung interactions. Annals of translational medicine. 2018 Sep:6(18):356. doi: 10.21037/atm.2018.08.10. Epub [PubMed PMID: 30370283]
Collins S, Martindale J. Optimizing Hypertensive Acute Heart Failure Management with Afterload Reduction. Current hypertension reports. 2018 Feb 24:20(1):9. doi: 10.1007/s11906-018-0809-7. Epub 2018 Feb 24 [PubMed PMID: 29478124]
Jain P, Hayward CS. Afterload Sensitivity of Continuous-Flow Left Ventricular Assist Devices and Abolition of Frank-Starling Forces Under Strain. Circulation. Heart failure. 2020 Feb:13(2):e006787. doi: 10.1161/CIRCHEARTFAILURE.119.006787. Epub 2020 Feb 14 [PubMed PMID: 32059631]
Salgado BC, Bhimaraj A. Physiological Concepts of Cardiogenic Shock Using Pressure-Volume Loop Simulations: A Case-Based Review. Methodist DeBakey cardiovascular journal. 2020 Jan-Mar:16(1):43-49. doi: 10.14797/mdcj-16-1-43. Epub [PubMed PMID: 32280417]
Level 3 (low-level) evidenceAvendaño-Pérez L, Soto ME, Ávila-Vanzzini N, Bracamontes-Castelo G, Ruán-Díaz JC, Alexanderson-Rosas E, Espinola-Zavaleta N. Mechanical deformation in adult patients with unrepaired aortic coarctation. The international journal of cardiovascular imaging. 2018 May:34(5):735-741. doi: 10.1007/s10554-017-1286-9. Epub 2017 Nov 30 [PubMed PMID: 29189934]
Schotola H, Sossalla ST, Renner A, Gummert J, Danner BC, Schott P, Toischer K. The contractile adaption to preload depends on the amount of afterload. ESC heart failure. 2017 Nov:4(4):468-478. doi: 10.1002/ehf2.12164. Epub 2017 Apr 19 [PubMed PMID: 29154423]
Howden EJ, Carrick-Ranson G, Sarma S, Hieda M, Fujimoto N, Levine BD. Effects of Sedentary Aging and Lifelong Exercise on Left Ventricular Systolic Function. Medicine and science in sports and exercise. 2018 Mar:50(3):494-501. doi: 10.1249/MSS.0000000000001464. Epub [PubMed PMID: 29077636]
Jernigan NL, Resta TC, Gonzalez Bosc LV. Altered Redox Balance in the Development of Chronic Hypoxia-induced Pulmonary Hypertension. Advances in experimental medicine and biology. 2017:967():83-103. doi: 10.1007/978-3-319-63245-2_7. Epub [PubMed PMID: 29047083]
Level 3 (low-level) evidenceNegishi K, Borowski AG, Popović ZB, Greenberg NL, Martin DS, Bungo MW, Levine BD, Thomas JD. Effect of Gravitational Gradients on Cardiac Filling and Performance. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2017 Dec:30(12):1180-1188. doi: 10.1016/j.echo.2017.08.005. Epub 2017 Oct 19 [PubMed PMID: 29056408]
Mills KI, Costello JM, Almodovar MC. A Review of Systemic Vasodilators in Low Cardiac Output Syndrome Following Pediatric Cardiac Surgery. Current vascular pharmacology. 2016:14(1):29-36 [PubMed PMID: 26463987]
Zayed M, Nassar H, Hasanin A, Saleh AH, Hassan P, Saad D, Mahmoud S, Abo Bakr G, Fouad E, Saleh N, Ismail M, El-Hadi H. Effects of nitroglycerin versus labetalol on peripheral perfusion during deliberate hypotension for sinus endoscopic surgery: a randomized, controlled, double-blinded trial. BMC anesthesiology. 2020 Apr 17:20(1):85. doi: 10.1186/s12871-020-01006-w. Epub 2020 Apr 17 [PubMed PMID: 32303182]
Level 1 (high-level) evidenceNaseratun N, Kobara M, Watanabe Y, Toba H, Nakata T. Comparison of effects of L/N-type and L-type calcium channel blockers on post-infarct cardiac remodelling in spontaneously hypertensive rats. Clinical and experimental pharmacology & physiology. 2020 Sep:47(9):1545-1553. doi: 10.1111/1440-1681.13329. Epub 2020 May 25 [PubMed PMID: 32323339]