Introduction
Upper blepharoplasty, whether performed for cosmetic reasons or functional reasons, is one of the most frequent operations performed on the face. Eyes and eyelids are the central features of the face that are seen by others and by patients every time they look into a mirror. We also converse by looking from eye-to-eye. This explains the popularity of products designed for use on brows, upper lids, lower lids, and eyelashes.
Definition
Upper blepharoplasty constitutes the surgical repair or reconstruction of the upper eyelid including management of upper eyelid skin, orbital septum, any underlying ptosis, and excess or deficient preaponeurotic and medial orbital fat. Blepharoplasty may be performed for cosmetic or reconstructive reasons, often both. [1]
Dermatochalasis refers to laxity or redundancy of eyelid skin and muscle. It is caused by changes due to loss of elastic tissues, thinning of the epidermis, weakening of connective tissue in eyelids, mechanical forces (rubbing), and aging. Genetic influences are also strong.
Steatoblepharon (from the Greek steatos meaning "relating to fat") is the prominence of eyelid fat pads and applies to the upper and lower eyelids. Steatoblepharon may be associated with weakening of the orbital septum and the overlying orbicularis muscle and skin. Dermatochalasis and steatoblepharon are usually noticed in the fourth decade but sometimes earlier.
Etymology
The word blepharoplasty is derived from the Greek blepharon which means "eyelid" and plassein which means "to form."
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Surface Anatomy
It is essential to understand the topography of upper eyelids. The eyelid skin crease is where the levator aponeurosis attaches to the subdermal tissues via anterior branches: immediately above this is the eyelid fold which usually "hides" the upper eyelid skin crease. Between the skin crease and the upper eyelid margin is the tarsal platform. Ideally, the ratio of the tarsal platform to the distance between the upper lid crease and the brow should be 1:1.618 (Golden ratio or phi). [2] The same ratio applies to many other facial proportions. Excessive removal of fat can change this ratio to 1:1 which is aesthetically displeasing. The upper lid fold that comes over the crease is also essential to give a 3-dimensional structure to the upper eyelid. Excessive removal of fat or skin can efface this fold, giving an unnatural appearance.
Temporal hooding is a common finding because of a combination of temporal brow ptosis and lateral dermatochalasis. Assessment will allow the surgeon to determine the need to reposition the brow tail or if direct lid surgery alone can address such temporal hooding. The degree of dermatochalasis can be more pronounced in certain diseases like thyroid eye disease, following trauma, the Ehlers-Danlos syndrome, blepharochalasis, xanthelasmata, angioneurotic edema, amyloidosis and elastolysis (Cutis laxa).[3]
From the inferior border of the brow to the upper eyelid margin, the distance should be no less than 20 mm. Often this needs to be 25 to 30 mm, depending upon age, gender, and position of the brow. Finally, the lash curve needs to be assessed to ensure a healthy and attractive lash curve is preserved or created with appropriate upper eyelid surgery.
Cross-Sectional Anatomy
Eyelid Lamellae
At the level of the tarsal plate, the upper eyelid has an anterior lamella of the upper eyelid skin and orbicularis oculi muscle. Upper eyelid skin measures about 850 microns in thickness and does not significantly become thinner with age. However, the eyelid skin does lose its elasticity with age. Pretarsal skin tends to be smooth in youth but will acquire lines with age related to loss of elastin and also weakened attachments to the skin from the levator aponeurosis. The posterior lamella at this level is composed of the tarsal plate and tarsal conjunctiva.
Above the tarsal plate, the anterior lamella is made of skin and orbicularis muscle with a fine layer of fat under the orbicularis. The middle lamella is made of the orbital septum, and the posterior lamella of the levator aponeurosis, Muller’s muscle, and conjunctiva. [4]
Tarsal Plates
The upper tarsal plates span the upper eyelids becoming the ligamentous medial and lateral canthal tendons. The upper tarsal plates are about 10 mm in height although it has been shown that there is a statistical difference in the average tarsal height of Caucasians (10.1 mm) when compared to Japanese tarsal height (8.2 mm). [5] Tarsal plates are about 1 mm in thickness.
Orbital Septum
The orbital septum is a multi-layered structure that arises from the arcus marginalis and inserts on the inferior levator aponeurosis. Its insertion is lower in Asian eyelids. Behind the orbital septum is the preaponeurotic fat. The medial septum over the nasal fat is thinner than the rest of the septum: this covers the nasal upper eyelid fat pad. The septum is the surgeon's friend as the levator is protected by the preaponeurotic fat, in front of which is the orbital septum.
Fat Pads
The upper eyelid has 2 fat pads which are separated by a loose septum. The medial fat pads of the upper and lower lids are paler than the other fat pads. The more yellow color of the central fat pad in the upper eyelid may be because of higher amounts of beta-carotene and lutein in this fat compared to the medial fat pad.[6] More endothelial-lined vessels and fibrous septae are found in the central upper lid fat pad compared to the medial fat pad.[7]
Levator Aponeurosis
The levator palpebrae superioris muscle, innervated by the superior division of the third cranial nerve (oculomotor nerve), becomes an aponeurosis soon after turning downwards at the Whitnall’s ligament. The aponeurosis inserts into the anterior surface of the upper third of the tarsal plates with insertions also going to the skin which form the eyelid crease.
Muller’s Muscle
Muller’s muscle is supplied by the sympathetic system. It arises from the levator muscle and inserts into the superior border of the tarsal space. Just above the tarsal plate, lies the superior peripheral marginal arcade on Müller’s muscle.
Lacrimal System
The lacrimal gland consists of the palpebral lobe and the orbital lobe. Both these glands send ductules into the superolateral fornix where the aqueous secretions are released. The lacrimal gland is not usually visible but may become prominent as a "lateral fat pad" if it prolapses forwards.
Canthal Tendons
The medial canthal tendon is a complex structure with superior and inferior limbs as well as reflections anteriorly and posteriorly.
The lateral canthal tendon attaches the tarsal plates to the lateral orbital rim with 2 main limbs: the anterior limb attaches to the anterior orbital rim and fuses with the lateral orbital condensation. The posterior limb inserts into the Whitnall's tubercle 3 to 4 mm behind the orbital rim, just above the horizontal. A further condensation inferiorly attaches at about 45 degrees to just inside the inferolateral orbital rim, about 3 to 4 mm behind the rim and has been called a "lateral tarsal strap." There is some debate about whether this is a truly distinct structure, as opposed to the infero-lateral retinaculum that is seen below the lateral canthal tendon and the structure that is properly released whenever elevating the lateral lower eyelid attachment.
Indications
Upper Blepharoplasty
An upper blepharoplasty may be indicated for functional reasons.[3]
- Excess laxity with temporal hooding can interfere with superior and supero-temporal vision and may make the patient constantly raise their brows or the chin in order to see. Patients may complain specifically of having difficulty driving and seeing traffic lights. Formal visual fields are sometimes carried out to objectively show the superior field constriction, although many believe this is a waste of precious resources as it rarely changes medical management or affects the outcome.
- Constant use of the frontalis muscle in the presence of dermatochalasis and ptosis may give rise to frontal headaches.
- Eye irritation may be caused by eyelash ptosis or entropion because of the dermatochalasis.
- Skin-on-skin irritation may cause dermatitis
- Down-gaze ptosis is the droop of the upper eyelids that occurs because of redundant upper eyelid skin and interferes with reading.
Cosmetic Blepharoplasty
Most patients seeking cosmetic blepharoplasty are seeking a more defined skin crease and an improvement in the fat prominence in the upper eyelids. Depending upon the changes, upper blepharoplasty is often performed with browlifts.
Contraindications
The presence of dry eyes, thyroid disease and proptosis and clotting disorders are relative contraindications. There are different degrees of dry eyes. When a patient has severe dry eyes, it is wise to counsel the patient to avoid blepharoplasty as even a moderate increase in corneal exposure can make the patient's dryness significantly worse. In the presence of thyroid orbitopathy with proptosis, blepharoplasty may create lagophthalmos with corneal and visual problems. Clotting disorders have to be managed individually and with the help of their physicians. Patients who have had one or more previous blepharoplasty procedures (which we see increasingly commonly), should be examined carefully for the available skin and orbicularis function as well as any lagophthalmos before suggesting further blepharoplasty. Finally, there is a subset of patients who have photophobia: it is best to avoid blepharoplasty in these patients.[8]
Equipment
No specialized equipment is needed for upper blepharoplasty other than standard plastic surgery and oculoplastic surgery instrument set.
Personnel
Upper blepharoplasty may be performed with straight local anesthesia with or without monitored sedation. These procedures can be performed safely in an office, surgical center or hospital operating theater. The surgeon must be familiar with the procedure of blepharoplasty and also have the experience and knowledge to address any preoperative and postoperative complications that may arise.
Preparation
A detailed history of the medical health is essential both, for the assessment of the safety of undertaking blepharoplasty as well as choosing the level of anesthesia for the patient. To that end, the medical history should review illnesses such as diabetes mellitus, hypertension, thyroid disease, respiratory diseases, dermatologic diseases, kidney disease, recurrent edema, and any bleeding disorders. Medications and supplements need to be reviewed as many drugs can increase the risk of bleeding. The list of drugs that can result in excessive bleeding is long. Smoking and alcohol use are evaluated as even in a relatively simple procedure like an upper blepharoplasty smoking can affect the healing of tissues. A review of antiplatelet and anticoagulant medication is vital with a discussion with the patient's primary physician who monitors these to ensure that it is safe to withhold these for 1 week before surgery and for up to a week following surgery.
A review of the psychiatric history and any evidence of a narcissistic personality disorder, body dysmorphic disorder or tendency to histrionic behavior should be noted. Where necessary, the patient should be referred to a psychologist or psychiatrist.
Ophthalmic History
Previous ocular surgery, including any refractive surgical procedures, need to be reviewed as many such patients will be predisposed to an increased need for lubrication. Blepharitis and meibomian gland dysfunction increase with age and especially in patients of Northern European origins: any current problems and how they are managed should be considered. Patients will often seek a repeat blepharoplasty but may not remember having had it done before, so an accurate history and examination are essential. Any current or history of dryness is obtained: specifically, patients should be asked if they use artificial tear drops and if so how many times a day they need drops.
Examination
Examination of upper eyelids should always include a review of the forehead, brows and upper eyelids. Underlying ptosis also needs to be assessed. It is well-recognized that when upper eyelid surgery is performed with or without ptosis repair, the position of the brows will drop, unmasking the brow ptosis, especially in men.[9] The symmetry of the upper eyelids or lack of it needs to be measured and documented. The amount of upper eyelid skin excess, it’s thickness, evidence of any inflammation or presence of skin lesions should be noted. It is important to look for and document facial (brow, eyelid but also forehead and cheek) asymmetry. In Asians and certain other populations, epiblepharon may be present and should be noted as the placement of the upper eyelid incision will affect the eventual scar and result. Patients may have one or more (primary, secondary, tertiary) skin creases and the creases may be asymmetric.
A formal Schirmer's test with topical anesthetic may be performed. However, it is no longer considered to be necessary because the results have not been found to be entirely reliable. [10] [11] However, review of the blink, closure, lower eyelid laxity (the distraction and snap-back tests) and assessment of the corneal tear film is needed. The Bell's phenomenon is assessed as 15% of the population will have a neutral or negative Bell's phenomenon.
Tarsal platform and eyelid crease: central to any blepharoplasty is the creation of an eyelid skin crease, below which is the tarsal show or tarsal platform. The skin crease is defined by the insertion of the anterior fibers of the levator aponeurosis into the dermis through the orbicularis oculi muscle. The skin crease height varies depending upon ethnicity, age, and gender. Men's upper eyelid crease is generally lower than that in women. However, even within a particular ethnic group, the skin crease height varies. We assess younger photographs of patients to get an idea of where the skin crease looked suitable for the patient. In Asian races, the skin crease will be very low (1 to 3 mm) because of the much lower insertion of the orbital septum on the levator aponeurosis and weaker dermal attachments by the levator aponeurosis. Aging causes a decrease in skin elasticity, weakening of the aponeurotic attachments to the tarsal as well as the dermis, and an overall reduction in the periorbital fat, which should all be assessed. Hollowing of the periorbital tissues together with the elevation of the skin crease and “skeletonization” of the orbit in advanced age can occur.
Corneal reflex-lid margin distance in Caucasians measures 3.5 to 4 mm. If it is below 3 mm or there is asymmetry, ptosis should be measured and corrected. Levator function should always be measured; normal is more than 12 mm.
The upper eyelid has a medial and central fat pad. These fat pads can be accentuated by pushing gently on the globe with the eyelids closed or on the lower eyelid. The central fat pad often spreads laterally, but any lateral “bulge” should be assumed to be that of the lacrimal gland which may prolapse forwards with age. The medial fat pad which is a lighter color than the central fat pad is more rounded and medial to the levator aponeurosis separated by a weak septum from the central fat pad. The central fat pad sits on the levator aponeurosis. The lacrimal gland is in the lacrimal sac fossa in the superolateral orbit. There is also preseptal retro-orbicularis fat present which can contribute to upper eyelid fullness. Any lateral upper eyelid bulge should be noted as it may be a prolapsed lacrimal gland. Understanding these anatomical details allows one to examine the various bulges on the upper eyelid accurately.
Brow position and assessment of the brow fat pad is essential. A full brow gives a youthful look. Rarely is it necessary to remove the brow fat pad. Secondary laxity causing some degree of droop of the brow fat (retro-orbicularis oculi fat) can occur, necessitating a surgical repositioning rather than removal.
At a minimum, the following measurements and assessments are made:
- Brow ptosis: Absent or present, mild, moderate or severe. Presence or absence of lateral brow ptosis (leading to secondary dermatochalasis)
- Brow shape
- Corneal reflex-lid margin distance (MRD-1). Normal measurement is 3.5 mm to 4 mm
- Levator function (more than 12 mm)
- Eyelid curve and height
- Pupils (any anisocoria)
- Ocular movements
- Examine the corneal surface (pterygia, scars, evidence of LASIK or radial keratotomy, conjunctival blebs, corneal dystrophies)
- Tear breakup time (BUT) and Schirmer’s test are often performed but the exact reliability is unknown.
- Bell's phenomenon. If the patient has a neutral Bell’s phenomenon or a negative one, conservative blepharoplasty is indicated.
- Lagophthalmos: May indicate underlying thyroid disease or prior eyelid surgery.
- Proptosis or enophthalmos. These can give rise to pseudo ptosis or eyelid retraction
- Hypertrophic or redundant orbicularis muscle
- Scleral show
- Examine the lower eyelid for laxity, position and canthal laxity.
- Beware of underlying blepharospasm which can give rise to orbicularis hypertrophy and redundancy and associated dermatochalasis and also an appearance of ptosis because of the tonic squeezing of the eyelids.
- Look for tarsal laxity (floppy eyelid syndrome). Patients will have a rubbery tarsal plate which may need horizontal shortening before being elevated.
- Consider blepharochalasis when the patient presents with recurrent eyelid swelling, often unilateral. There will be associated eyelid atrophy. Patients will eventually develop ptosis, steatoblepharon and excessively thin eyelid skin. This condition shows lymphedema with epithelial atrophy and loss of elastic fibers, but there is no pathognomonic histopathological finding.
- Fluid retention in the upper and lower eyelids (and festoons) are often seen in patients with kidney failure and in patients on CPAP machines.
- Hereditary angioedema should be suspected if there is intermittent swelling of the eyelids: C1-esterase inhibitor levels are assessed.
Technique or Treatment
Markings
The upper eyelid skin crease should be marked either where it is or where the desired skin crease should be. It should be remembered that the final skin crease often ends up higher than the marked skin crease. Symmetry is important. The degree of skin excision is variable and is marked with a lateral raise in the incision. The amount of orbicularis muscle resection again has to be determined based upon numerous factors and the same applies to fat removal. More conservative blepharoplasty with tissue preservation (fat and muscle) has become more popular to retain or recreate normal periorbital fullness.
The medial extent of the markings are no more medial than the punctum, and the lateral markings are kept within the lateral orbital rim. A medial “W” plasty may be necessary if there is a more profound degree of skin removal necessary. The degree of skin removal will be judged depending upon the position of the brow and with consideration of any brow elevation. Some surgeons mark the amount of skin to be removed by pinching the skin with the patient lying down. This can be a useful technique to ensure that not too much skin is removed. We generally prefer to mark the removal of the skin with the patient sitting up. Adjustment can then be made during the surgery. Certainly, at least 10 mm should be left between the upper incision and the inferior border of the brow. The normal distance between the lid margin and the inferior border of the brow is more than 25 mm in the unoperated adult face. Although guidelines have been given (leave at least 20 mm between the upper lid margin and the inferior border of the brow, for example), we find that this amount varies and depends upon numerous factors, including whether a concurrent brow repositioning is being performed, history of prior surgery, orbicularis strength, Bell’s phenomenon, any underlying eye dryness, among others.
The shape of the excision is such that more tissue is resected laterally with the maximal resection being at the lateral canthus. Modifications in the incision designs have been made with even more tissue being removed laterally in some patients with brow ptosis where no brow elevation is being performed but the temporal hooding needs to be improved. Surgeons have shown acceptable results using this technique.[12] Incisions carried low laterally will affect innervation of the orbicularis oculi muscle with resultant lagophthalmos.
Volume Augmentation
Attention, of late, has quite correctly turned to volume augmentation rather than just subtractive surgery.[13] It is not uncommon to have volume loss of the brow fat as well as the middle fat pad. The medial fat pad is often prominent. This is probably because the central fat pad gets pulled back together with the levator aponeurosis and the orbital septum with the inevitable enophthalmos that occurs with age and posterior movement of the orbital fat. The medial fat pad does not sit on the levator aponeurosis and becomes more prominent. The orbital septum is also less substantial over the medial fat pad, allowing the anterior dislocation of the fat. Fat grafting may be performed or fat may be preserved and transposed into the hollow areas.[14]
Anesthesia
Upper blepharoplasty may be performed with straight local anesthesia or under conscious sedation. Local anesthesia injection with lidocaine and epinephrine subcutaneously with care being taken not to inject too deeply so the levator muscle is not affected. Patients may move suddenly when injections are being performed. Therefore, steadying the head and injecting with the needle pointing away from the globe are two techniques that can help prevent this. We usually inject 1.5 mL per side and top up the anesthetic through the procedure. Most patients will need additional injections when operating upon the medial fat pad and along the incision lines when closing the wounds.
Incisions
Incisions may be made with a 15 Bard-Parker blade, an electrocautery, a CO2 laser or a radiofrequency needle.
Removal of Orbicularis
Stretching of the skin can cause some degree of redundancy of the orbicularis oculi muscle but care must be taken to remove conservative amounts of orbicularis muscle. Pretarsal orbicularis must always be preserved. A variable amount of orbicularis over the preseptal region is removed, depending upon the patient’s age, the degree of redundancy and whether any brow lifting is being performed. Removal of a small strip of orbicularis, together with work on the septum and fat (see below) can create a more defined crease.
The Orbital Septum
In some cases, the orbital septum may not need to be opened. Simple cautery to the surface of the septum does not give long-term tightening as there is tissue restitution over time. In most cases, the orbital septum is opened and planned fat removal is performed.
Fat
Unsatisfactory blepharoplasty results may be seen if the medial fat pad is not adequately debulked.[15] On the other hand, if the central fad pad is removed aggressively, an “A frame” deformity with a hollow superior sulcus will form. In some patients, especially when a repeat blepharoplasty or revision blepharoplasty is being performed, fat transposition may be performed to reacquire the natural sub brow fullness of a healthy, attractive eyelid. On rare occasions, a pedicle from the medial fat pad can be brought to the central zone if there is volume deficiency there. The art of blepharoplasty is to know how much to remove, how much to preserve and how much to reposition.
Closure can be with interrupted 6-0 catgut sutures which allow for a good wound but 6-0 nylon or prolene may also be used.
Postoperative Care
We put patients on topical erythromycin eye ointment twice a day to the sutures and use of artificial tears as needed. Most patients do not need prescription analgesics. Anticoagulants are usually recommenced by day 2. We have patients ice their eyelids on-and-off for the first 24 hours and have them sleep with the head up for two nights. Patients may wash/bathe/shower and get their sutures wet in the shower the next day.
Complications
All patients will have some degree of bruising and swelling, which may last up to 2 weeks. If upper eyelids are being operated upon because of a ptosis and also with blepharoplasty, some degree of dryness is inevitable. Most patients will need topical lubrication with drops during the day. Some patients need a topical lubricating ointment at night.
Eyelid Sensation
As the eyelid margin is supplied by branches of the supraorbital nerve centrally and laterally and the supratrochlear nerve medially, upper eyelid incisions will result in decreased sensation along the eyelid margin for six to eight weeks. Although most patients recover by 8 weeks, some numbness can persist for longer.[16] Females will recognize the numbness when they apply makeup on the eyelid margin.
Lagophthalmos and Dry Eyes
Early in the postoperative period, almost every patient will experience some degree of lagophthalmos. However, within a few days, this settles and there is complete closure of the eyelids. This is where the experience of the surgeon is important as a number of factors affect the height of the upper eyelid and its ability to close. Peroperatively, local anesthetic injections will partially paralyze the orbicularis muscle, giving the levator a mechanical functional advantage. If there is diffusion of any anesthetic into the levator and Müller’s muscle, the lid elevation will be affected. Most surgeons will aim for a slight lagophthalmos on the table, especially when ptosis correction is also undertaken. Topical lubricants with drops and ointment are useful for the first few days to weeks until the lagophthalmos resolves.
Even without lagophthalmos, the patient may experience dryness of the eyes. This is because the lid blink and degree of closure (firmness of closure) are affected in the first few weeks after surgery. Furthermore, any other underlying conditions that contribute to dryness (Meibomian gland disease, blepharitis, acne rosacea, lower lid laxity, etc) will exacerbate the postoperative dryness. It is important to monitor the corneas. On occasion, it may be necessary to place temporary punctal plugs in the lower puncta. These can be removed once the postoperative dryness is resolved.
Tearing
Tearing because of relative dryness of the cornea may occur for a few days. Topical ointment like Refresh pm ointment or Soothe ointment at night helps. During the daytime, if there is dryness, use of Celuvisc or Genteal gel are useful.
Hemorrhage
Ecchymosis is not uncommon. However, a retrobulbar hemorrhage is an emergency which necessitates opening of the wound and the deeper tissues to release the hematoma.[17] Bleeding may occur from vessels within the preaponeurotic fat or from sub-orbicularis vessels just below the incision. Patients will present with pain, proptosis, nausea and vomiting and reduced vision. It should be remembered that blepharoplasty generally causes little discomfort. Therefore, any severe pain after blepharoplasty should be assumed to be because of retrobulbar hemorrhage until proven otherwise. Immediate opening of the wound with or without a canthotomy and cantholysis is necessary.
Assymetric Eyelid Creases
When making a skin crease incision, it is important to remember that the final crease often ends up about 2-mm higher. Lowering a high skin crease is difficult and the results are unpredictable.[18]
Asymmetric Height and Eyelid Adjustment
Upper eyelid blepharoplasty is an art form, and small differences are often seen in all patients. It is wise to allow all the swelling to settle to determine if additional adjustments are needed. We rarely adjust before 2 months after surgery. Adjustable upper eyelid ptosis repair was described some years ago but is very rarely used.
Blepharoplasty Refinements
Wrinkles of Upper Eyelid Skin and Sub-Brow Skin
Fine wrinkles are often seen on the tarsal platform and also between the upper lid crease and the brow. These latter lines are radial lines, which become more common with aging. “Pulling” on the upper lid skin or brow skin does not resolve these particular wrinkles. The use of the CO2 laser with one pass at 90 mj gives very nice results to these wrinkles.
Addressing Temporal Hooding
Some surgeons have recommended extending the lateral arc of the upper lid skin excision laterally and up close to the brow and have shown nice results with minimal scarring when the patient does not want to have a brow lift performed.[19] The concern is that one is extending the incision from the thin skin of the upper lid to the thick skin of the brow. Such a transition can give a scar that may be visible. This procedure should not be performed for purely cosmetic reasons where we would prefer to perform a combination of a brow lift and upper blepharoplasty. In some older patients, this is a reasonable approach.
Skin Crease Reformation
When a well-defined skin crease needs to be designed, we pick up the levator aponeurosis in the skin closure sutures. One can use buried vicryl sutures from the subcutaneous tissue to the aponeurosis or pick up the aponeurosis with the skin closure suture. Removal of a strip of the orbicularis oculi muscle and some preaponeurotic fat also allows a more defined upper eyelid skin crease.
Filling the "A" Frame Central Eyelid
As one ages, prominence of the medial fat pad and posterior dislocation of the central fat pad with stretching or disinsertion of the levator aponeurosis (and also age-related fat atrophy more posteriorly) gives a deep superior sulcus. Free fat grafts may be used to fill this space. Another options is to mobilize the upper eyelid fat pad behind the orbital septum, bring the fat forwards and suture it to the orbicularis under the incision. This gives nice results without the need for free fat grafts. The medial fat pad can also be mobilized and transposed centrally, but the whole central concavity cannot be adequately addressed using this technique.
Lateral Brow
Botulinum toxin is injected in the lateral sub-brow orbital orbicularis to give a nice lift to the brow tail. A similar resection of a small amount of orbital orbicularis oculi muscle may be performed to provide a subtle brow lift. [20]This resection does not seem to give as impressive a lift as the use of botulinum toxin, so we reserve this for subtle lifts only.
Internal Brow Lifts
"Internal brow lifts” should be considered as brow stabilizing procedures. We do not believe that you can get a long-lasting and substantial brow position and curve change by pushing the brow from below. We do not use the “internal brow lift” procedure.
Clinical Significance
Upper blepharoplasty is a commonly performed cosmetic and functional surgical procedure. However, since the eyelids protect the most important of the senses, vision, it is imperative that surgery is undertaken with careful assessment and planning. Surgeons should advise patients that they have the option of not undergoing surgery, but if they choose to have the surgery, they should provide detailed information on what the patients should expect as well as details of all possible outcomes that apply to the individual patient.
Enhancing Healthcare Team Outcomes
Several different medical subspecialists commonly perform upper blepharoplasty: ophthalmologists, otolaryngologists, plastic surgeons, oculoplastic surgeons, dermatologists, and even dentists, gynecologists, and general practitioners. Without careful screening of patients, complications may occur. At the very least, undesirable outcomes may be experienced by the patient. Outcomes may be improved if all surgeons carefully consider the important aspects of blepharoplasty as discussed and the nursing staff carefully monitors the patient for postoperative complications. (Level V)
Media
(Click Image to Enlarge)
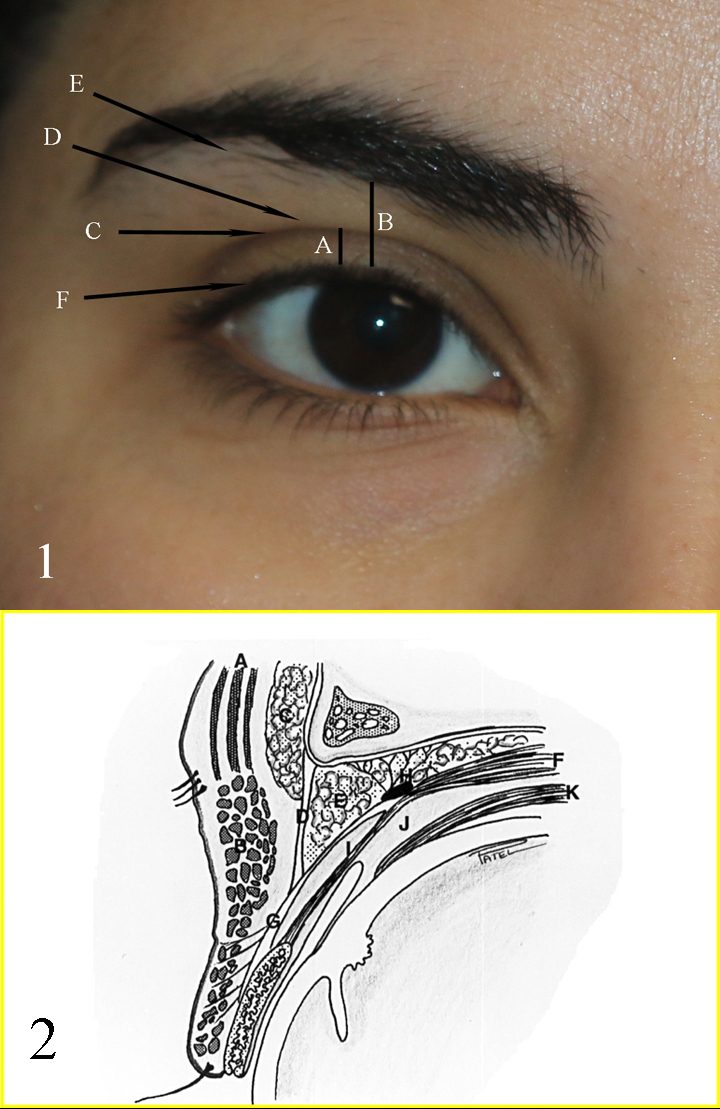
Fig 1: A: upper eyelid platform; B: Brow to Lid margin distance; C: Upper eyelid crease; D: Upper eyelid fold; E: Brow fatpad; F: Eyelid margin and eyelash curve Fig 2: A: Frontalis muscle; B: Orbicularis muscle; C: Brow fat pad; D: Orbital septum; E: Preaponeurotic fat pads; F: Levator muscle; G: Levator aponeurosis; H: Whitnall ligament; I: Muller muscle; J: Common sheath; K: Superior rectus muscle Contributed by Professor Bhupendra C. K. Patel MD, FRCS
(Click Video to Play)
References
Kwitko GM, Patel BC. Blepharoplasty Ptosis Surgery. StatPearls. 2025 Jan:(): [PubMed PMID: 29493921]
Stein R, Holds JB, Wulc AE, Swift A, Hartstein ME. Phi, Fat, and the Mathematics of a Beautiful Midface. Ophthalmic plastic and reconstructive surgery. 2018 Sep/Oct:34(5):491-496. doi: 10.1097/IOP.0000000000001167. Epub [PubMed PMID: 29952930]
Hollander MHJ, Contini M, Pott JW, Vissink A, Schepers RH, Jansma J. Functional outcomes of upper eyelid blepharoplasty: A systematic review. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2019 Feb:72(2):294-309. doi: 10.1016/j.bjps.2018.11.010. Epub 2018 Nov 22 [PubMed PMID: 30528286]
Level 1 (high-level) evidenceKashkouli MB, Abdolalizadeh P, Abolfathzadeh N, Sianati H, Sharepour M, Hadi Y. Periorbital facial rejuvenation; applied anatomy and pre-operative assessment. Journal of current ophthalmology. 2017 Sep:29(3):154-168. doi: 10.1016/j.joco.2017.04.001. Epub 2017 Apr 25 [PubMed PMID: 28913505]
Goold LA, Casson RJ, Selva D, Kakizaki H. Tarsal height. Ophthalmology. 2009 Sep:116(9):1831-1831.e2. doi: 10.1016/j.ophtha.2009.05.035. Epub [PubMed PMID: 19729100]
Level 3 (low-level) evidenceSires BS, Saari JC, Garwin GG, Hurst JS, van Kuijk FJ. The color difference in orbital fat. Archives of ophthalmology (Chicago, Ill. : 1960). 2001 Jun:119(6):868-71 [PubMed PMID: 11405838]
Manstein CH, Lucas R. Use of immunohistochemical stains to assess the variations in color of fat of the upper eyelid. Plastic and reconstructive surgery. 2005 Jan:115(1):278-81 [PubMed PMID: 15622264]
Neimkin MG, Holds JB. Evaluation of Eyelid Function and Aesthetics. Facial plastic surgery clinics of North America. 2016 May:24(2):97-106. doi: 10.1016/j.fsc.2015.12.002. Epub [PubMed PMID: 27105795]
Huijing MA, van der Palen J, van der Lei B. The effect of upper eyelid blepharoplasty on eyebrow position. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2014 Sep:67(9):1242-7. doi: 10.1016/j.bjps.2014.05.022. Epub 2014 May 24 [PubMed PMID: 24939828]
McKinney P, Byun M. The value of tear film breakup and Schirmer's tests in preoperative blepharoplasty evaluation. Plastic and reconstructive surgery. 1999 Aug:104(2):566-9; discussion 570-3 [PubMed PMID: 10654706]
Espinoza GM, Israel H, Holds JB. Survey of oculoplastic surgeons regarding clinical use of tear production tests. Ophthalmic plastic and reconstructive surgery. 2009 May-Jun:25(3):197-200. doi: 10.1097/IOP.0b013e3181a1d4a5. Epub [PubMed PMID: 19454930]
Level 3 (low-level) evidenceHar-Shai Y, Hirshowitz B. Extended upper blepharoplasty for lateral hooding of the upper eyelid using a scalpel-shaped excision: a 13-year experience. Plastic and reconstructive surgery. 2004 Mar:113(3):1028-35; discussion 1036 [PubMed PMID: 15108902]
Rohrich RJ, Villanueva NL, Afrooz PN. Refinements in Upper Blepharoplasty: The Five-Step Technique. Plastic and reconstructive surgery. 2018 May:141(5):1144-1146. doi: 10.1097/PRS.0000000000004439. Epub [PubMed PMID: 29697612]
Riesco B, Abascal C, Duarte A, Flores RM, Rouaux G, Sampayo R, Bernardini F, Devoto M. Autologous fat transfer with SEFFI (superficial enhanced fluid fat injection) technique in periocular reconstruction. Orbit (Amsterdam, Netherlands). 2018 Jun:37(3):191-195. doi: 10.1080/01676830.2017.1383470. Epub 2017 Oct 17 [PubMed PMID: 29040029]
Oh SR, Chokthaweesak W, Annunziata CC, Priel A, Korn BS, Kikkawa DO. Analysis of eyelid fat pad changes with aging. Ophthalmic plastic and reconstructive surgery. 2011 Sep-Oct:27(5):348-51. doi: 10.1097/IOP.0b013e3182141c37. Epub [PubMed PMID: 21490516]
Level 2 (mid-level) evidenceBlack EH, Gladstone GJ, Nesi FA. Eyelid sensation after supratarsal lid crease incision. Ophthalmic plastic and reconstructive surgery. 2002 Jan:18(1):45-9 [PubMed PMID: 11910324]
Mack WP. Complications in periocular rejuvenation. Facial plastic surgery clinics of North America. 2010 Aug:18(3):435-56. doi: 10.1016/j.fsc.2010.05.002. Epub [PubMed PMID: 20659676]
Young SM, Kim YD, Kim JH, Lang SS, Woo KI. Lowering of the High Eyelid Crease in Revision Upper Eyelid Surgery. Aesthetic plastic surgery. 2019 Feb:43(1):139-146. doi: 10.1007/s00266-018-1235-6. Epub 2018 Oct 1 [PubMed PMID: 30276454]
Beraka GJ. Extended upper blepharoplasty for lateral hooding. Plastic and reconstructive surgery. 2005 Jan:115(1):339; author reply 339-40 [PubMed PMID: 15622282]
Level 3 (low-level) evidenceArmstrong BK, Sobti D, Mancini R. Partial Orbicularis Resection for the Augmentation of Traditional Internal Brow Pexy: The "Tuck and Rise". Ophthalmic plastic and reconstructive surgery. 2016 Nov/Dec:32(6):473-476 [PubMed PMID: 27429226]