Introduction
Esophageal perforations and tears present a significant and complex challenge for the therapeutic team, necessitating an interprofessional approach for successful management. These injuries can occur in 3 distinct anatomical compartments—cervical, thoracic, and abdominal—each with a range of often nonspecific symptoms. This variability in presentation can lead to significant delays in diagnosis, complicating the management of the condition. Despite advancements in diagnostic technologies and therapeutic strategies, esophageal perforations and tears remain life-threatening, with mortality rates reaching up to 50%.
The incidence of esophageal perforation in the United States is approximately 3 per 100,000 individuals, with intrathoracic perforations being the most common, accounting for 54% of cases. Cervical esophageal perforations follow at 27%, while intraabdominal perforations comprise 19%.[1][2][3][4] Iatrogenic causes, particularly those related to endoscopic procedures, are the leading contributors to esophageal perforation, responsible for 59% of cases. In contrast, traumatic external injuries rarely result in esophageal perforation; however, when foreign objects are involved, fish bones are the most frequent cause, accounting for 12% of cases.
The concurrence of esophageal perforation and mediastinal abscesses is relatively rare, but when it occurs, it can lead to severe complications such as thoracic abscess, sepsis, and septic shock, with mortality rates as high as 66%. The critical importance of prompt identification and diagnosis cannot be overstated, as studies show that delays in diagnosis significantly increase mortality rates. Treatment strategies for esophageal perforations, particularly those complicated by mediastinal abscesses, often involve surgical intervention or drainage, underscoring the need for a timely and coordinated therapeutic approach.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The esophagus, a 25 cm-long fibromuscular tube, extends from the pharynx to the stomach, beginning at the level of the C6 vertebra in the neck and descending through the mediastinum before passing through the diaphragm at the T10 vertebra. This vertical structure includes 3 anatomical constrictions that are significant in the context of esophageal perforations—the cricopharyngeal sphincter, located approximately 15 cm from the upper incisor teeth; the crossing of the aortic arch and the left main bronchus at about 23 cm; and the lower esophageal sphincter at 40 cm, where the esophagus passes through the diaphragm.
The esophagus is anatomically divided into 3 regions—the cervical esophagus, the thoracic esophagus, and the abdominal esophagus. Each segment receives its blood supply from distinct arteries: the cervical portion is supplied by the inferior thyroid artery, the thoracic portion by the bronchial and esophageal branches of the descending thoracic aorta, and the abdominal portion by the left phrenic and gastric arteries. Understanding the anatomical course and blood supply of the esophagus is crucial for identifying potential perforation sites and determining the implications for surgical management.
Iatrogenic Perforations
Iatrogenic perforations are the most common cause of esophageal perforations and are predominantly associated with medical procedures, especially during diagnostic and therapeutic endoscopy. While the risk of perforation is generally low during diagnostic endoscopy using flexible endoscopes, it increases significantly during therapeutic interventions. Procedures such as pneumatic dilation, hemostasis, stent placement, foreign body extraction, cancer palliation, and endoscopic ablation techniques are all associated with a heightened risk of esophageal perforation.
The anatomical sites most commonly affected by iatrogenic perforations are the hypopharynx and the distal esophagus, corresponding to the first and third anatomical constrictions, respectively. Additionally, invasive surgical procedures such as fundoplication and esophageal myotomy carry a risk of iatrogenic perforation, particularly in the distal esophagus.[6][7][8] Although rare, iatrogenic perforations can result in significant morbidity, necessitating prompt diagnosis and management.
Spontaneous Ruptures
Spontaneous ruptures, commonly referred to as Boerhaave syndrome, are the leading cause of noniatrogenic esophageal perforations, accounting for approximately 15% of all cases. These ruptures occur due to a sudden increase in intraesophageal pressure combined with negative intrathoracic pressure, often triggered by forceful vomiting, retching, or straining. The result is a longitudinal tear, typically located on the posterolateral wall of the esophagus just above its diaphragmatic hiatus. The left side of the esophagus is more frequently affected than the right, with 90% of spontaneous ruptures occurring on the left. These ruptures can vary significantly in size, ranging from 0.6 to 8.9 cm, and are medical emergencies requiring immediate attention.
Traumatic Perforations
Although rare, traumatic injuries to the esophagus are potentially life-threatening. These injuries can result from penetrating trauma, such as gunshot or stab wounds, or from blunt trauma. Penetrating injuries are more common and tend to result in direct perforation of the esophagus. In contrast, blunt trauma is often associated with more severe injuries, such as cardiac contusion or aortic dissection, which can obscure the presence of an esophageal perforation. Both types of traumatic injuries require rapid diagnosis and intervention to prevent catastrophic outcomes.
Foreign Body-Induced Perforations
Esophageal perforations secondary to foreign body impaction are rare but carry significant risk, particularly when the foreign object exerts prolonged pressure on the esophageal wall. The distal third of the esophagus is the most common site for impaction, often predisposed by underlying conditions such as peptic stricture, achalasia, or esophagitis. Impaction in the middle third is frequently associated with strictures or obstructive neoplasms. The prolonged presence of a foreign body can lead to pressure necrosis, resulting in ischemia of the affected segment and subsequent perforation.[9] Early identification and removal of the foreign body are crucial to prevent these complications.
Epidemiology
Esophageal perforations and tears are rare but serious medical conditions associated with significant mortality and morbidity. They occur at a rate of approximately 3 per 100,000 individuals in the United States and can affect patients across all age groups, although certain populations are at higher risk. Iatrogenic perforations, the most common cause, are frequently observed in older adults due to their higher likelihood of undergoing diagnostic and therapeutic endoscopic procedures. Spontaneous ruptures, often linked to excessive alcohol consumption and forceful vomiting, are more common in middle-aged males. Traumatic perforations, typically resulting from violent incidents or accidents, are more prevalent in younger adults, particularly males.
The anatomical distribution of esophageal perforations is as follows: 55% occur in the intrathoracic esophagus, 25% in the cervical esophagus, and 20% in the abdominal esophagus. This distribution has important implications for diagnosis and treatment, as the location of the perforation can significantly influence clinical presentation and outcomes.
A systematic review of 1319 studies on acute esophageal perforations, published between 2005 and 2015, analyzed key outcomes such as mortality, diagnostic intervals, anatomical location, and management strategies. The review included 52 studies comprising 2830 cases, with an average patient age of 58.4. The mortality rate across these studies was 13.3%, based on data from 1644 patients. Delays in diagnosis were significant, with 58.1% of patients admitted within 24 hours of perforation. Thoracic perforations were the most common, occurring in 72.6% of patients. Iatrogenic causes accounted for 46.5% of perforations, highlighting the need for meticulous procedural practices.
Initial conservative management was used in 51.3% of cases, while computed tomography (CT) scans, radiographs, and endoscopy were the primary diagnostic tools, confirming diagnoses in 38.7%, 36.6%, and 37.4% of cases, respectively. Sepsis was present in 23.3% of cases at admission, underscoring the severe complications that can result from delayed diagnosis.[10]
Pathophysiology
Esophageal perforations and tears signify a severe disruption of the esophageal wall, triggering a cascade of life-threatening physiological events. Understanding the underlying pathophysiology is essential for timely diagnosis and effective management.
Anatomical and Structural Considerations
The esophagus has several layers—the mucosa, submucosa, muscularis propria, and adventitia. The absence of a serosal layer makes the esophagus particularly vulnerable to perforation and limits its ability to contain perforations once they occur. Esophageal perforations can arise in any of the 3 natural constrictions of the esophagus, as mentioned below.
- Cervical constriction: This is near the cricopharyngeal sphincter at the level of the C6 vertebra, approximately 15 cm from the upper incisors.
- Thoracic constriction: This is where the esophagus is crossed by the aortic arch and left main bronchus, approximately 23 cm from the upper incisors.
- Diaphragmatic constriction: This is where the esophagus pierces the diaphragm at the T10 vertebra, approximately 40 cm from the upper incisors.
Mechanisms of Perforation and Tear Formation
Esophageal perforations and tears can arise from various etiologies, including iatrogenic, spontaneous, traumatic, and foreign body-related factors. These can be broadly categorized into intraluminal and extraluminal injuries, as mentioned below.
Intraluminal injuries: These injuries originate from within the esophagus and may result from the factors mentioned below.
- Instrumentation: Iatrogenic perforations, the most common cause, occur during diagnostic or therapeutic endoscopic procedures. The risk is heightened during interventions such as pneumatic dilation, stent placement, or foreign body extraction.
- Ingestion of foreign bodies or caustic substances: Sharp objects such as fish bones can perforate the esophagus, while caustic substances cause chemical burns leading to perforation.
- Esophagitis and carcinoma: Chronic inflammation or malignancy can weaken the esophageal wall, making it susceptible to rupture.
- Infection or barotrauma: Conditions such as severe vomiting can cause a sudden increase in intra-esophageal pressure, leading to spontaneous rupture (Boerhaave syndrome).
Extraluminal injuries: External forces can cause extraluminal injuries, as mentioned below.
- Traumatic injuries: Penetrating trauma, such as stab or gunshot wounds, directly disrupts the esophageal wall, while blunt trauma can indirectly cause perforation by compressing the esophagus against rigid structures such as the spine or trachea.
- Surgical accidents: Iatrogenic injuries can also result from invasive surgical maneuvers, such as fundoplication or esophageal myotomy.[11][12]
Pathophysiological Consequences
The immediate consequence of esophageal perforation is the breach of the esophageal wall, which allows the contents of the esophagus and stomach to leak into surrounding structures. This leakage can lead to various complications, as mentioned below, depending on the location of the perforation.
Chemical mediastinitis and superinfection: Leakage of gastric contents, saliva, biliary fluid, and other secretions into the mediastinum can cause chemical burns, resulting in chemical mediastinitis. This condition is characterized by inflammation, mediastinal emphysema, and subsequent necrosis. Within hours of a full-thickness tear, polymicrobial bacterial translocation and invasion can occur, leading to sepsis and, if untreated, potentially death. The absence of a serosal layer in the esophagus exacerbates these processes, allowing rapid spread of infection and inflammation.
Pleural effusion: After esophageal perforation, pleural effusion often develops. This may be a sympathetic effusion, where the pleura remains intact, or an exudative effusion, occurring when the mediastinal pleura ruptures and contaminated gastric fluid is drawn into the pleura by negative intrathoracic pressure. The development of pleural effusion further complicates the clinical picture and can indicate the severity of the perforation.
Sepsis and septic shock: If the perforation is not promptly recognized and treated, the inflammatory response can escalate to systemic inflammation, leading to sepsis. Sepsis is a life-threatening condition characterized by widespread tissue damage and organ failure, and it can ultimately result in death. Septic shock, the most severe form of sepsis, occurs when blood pressure drops to dangerously low levels and multiple organs begin to fail.
History and Physical
The clinical manifestations of esophageal perforations are highly variable and depend on several critical factors, including the etiology and anatomical location of the perforation, the degree of contamination, the involvement of nearby mediastinal structures, and the time elapsed between perforation and the initiation of treatment.[13][14] A thorough history and physical examination are essential for early recognition and significantly impact patient outcomes.
History
Patients with esophageal perforations may present with a diverse range of symptoms, which are often influenced by the location and cause of the perforation. Key historical elements to consider when evaluating a suspected esophageal perforation include:
- Recent medical procedures
- Alcohol consumption and vomiting
- Trauma
- Ingestion of foreign bodies or caustic substances
- Sudden onset of pain
Physical Examination
The physical findings in esophageal perforation vary significantly depending on the location of the perforation—cervical, intrathoracic, or intraabdominal—and the extent of contamination and secondary injury. Common findings associated with each perforation location are listed below.
- Cervical esophageal perforations include:
- Neck pain, odynophagia, and dysphagia
- Dysphonia
- Neck crepitus
- Tenderness
- Thoracic esophageal perforations include:
- Retrosternal chest pain
- Chest wall crepitus
- Mediastinal crackles (Hamman sign)
- Signs of pleural effusion, such as dyspnea, tachypnea, dullness to percussion, and decreased tactile fremitus, may be exhibited by patients. These signs indicate potential complications, including pleural effusion, which can further complicate thoracic esophageal perforations.
- Abdominal esophageal perforations include:
- Epigastric pain: This often radiates to the shoulder, and this pain may be associated with nausea and vomiting, thereby reflecting the irritation of the diaphragm.
- Signs of peritonitis: When perforation leads to peritoneal contamination, patients may present with acute abdomen characterized by severe abdominal pain, guarding, and rigidity.
- Systemic signs of complications: As the perforation progresses, systemic signs of severe complications, such as mediastinitis or sepsis, may emerge, as listed below.
- Fever
- Tachycardia
- Tachypnea
- Hypotension
- Cyanosis
Evaluation
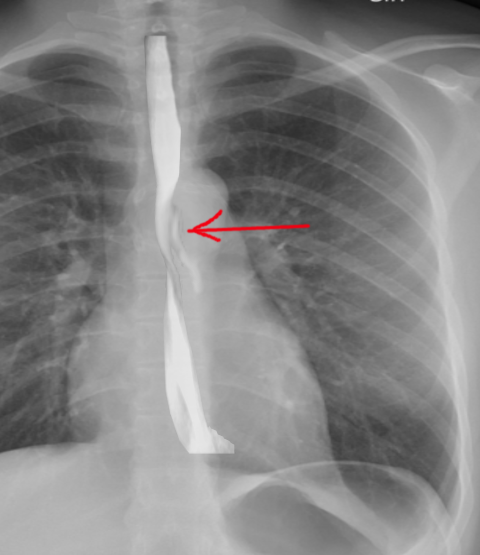
The evaluation of esophageal perforations and tears requires a systematic approach that integrates clinical assessment with imaging studies to confirm the diagnosis and determine the extent of the injury. Given the potentially life-threatening nature of these conditions, prompt and accurate evaluation is essential for guiding appropriate management (see Image. Perforation of the Esophagus).
Plain Radiography
Plain radiography is often the first imaging modality used when esophageal perforation is suspected. While it may not directly visualize the esophageal tear, it can provide critical indirect evidence of perforation:
- Subcutaneous emphysema: In cases of cervical esophageal rupture, air escaping into the soft tissues of the neck can cause subcutaneous emphysema, which appears as radiolucent streaks on plain films.
- Pneumomediastinum: Air in the mediastinum is a hallmark of thoracic esophageal perforation and may appear as radiolucent areas around the heart and great vessels, which is often accompanied by a widening of the mediastinal shadow.
- Free air under the diaphragm: For abdominal esophageal perforations, plain radiographs may show free air under the diaphragm, indicating perforation into the peritoneal cavity.
- Pleural effusion and hydropneumothorax: These findings may be present on chest radiographs if the perforation has contaminated the pleural space. A hydropneumothorax, characterized by air and fluid in the pleural space, can be particularly suggestive.
- Air in prevertebral space: This can indicate the presence of air leaking into the soft tissues around the vertebral column, often associated with esophageal perforation.
Contrast Esophagography
Contrast esophagography is the preferred diagnostic test for confirming esophageal perforation. This test involves the administration of contrast material to visualize the esophagus and detect any leakage indicative of a perforation.
- Leakage of contrast material: The hallmark sign of esophageal perforation on contrast esophagography is the extravasation of contrast material outside the lumen of the esophagus, which confirms the presence of a tear.
- Dye extravasation: This confirms the diagnosis and helps delineate the location and extent of the rupture, which is critical for surgical planning.
- Choice of contrast agent: Barium-based contrast agents are more accurate and specific than water-soluble contrasts. However, due to the risk of barium-induced chemical mediastinitis, water-soluble agents are generally preferred if there is a risk of leakage into the mediastinum. These agents are safer, although slightly less sensitive.
Computed Tomography
A CT scan of the chest and abdomen is a valuable tool in the evaluation of esophageal perforations, particularly when the diagnosis is uncertain or when complications are suspected.
- Periesophageal fluid collections: Fluid collections around the esophagus, pleural effusions, or ascites can be detected on CT, indicating the spread of infection or inflammation from the perforation.
- Esophageal thickening: Thickening of the esophageal wall may suggest underlying pathology, such as inflammation or neoplasia, that has led to the perforation.
- Pneumomediastinum: While similar to plain radiography, CT offers greater detail in detecting pneumomediastinum, allowing for a more precise assessment of the extent and location of air within the mediastinum.
- Intraabdominal collections: In cases of abdominal esophageal perforation, CT can identify intraabdominal abscesses or other collections that may require percutaneous or surgical drainage.
Treatment / Management
Esophageal perforations and tears are medical emergencies with high mortality rates, ranging from 36% to 50%, even with prompt intervention. The treatment approach is multifaceted and must be tailored to the patient's clinical condition, the timing of diagnosis, and the extent of the injury. Optimized initial resuscitation and timely decision-making between surgical and nonsurgical management are crucial for improving patient outcomes.[15][16](A1)
Initial Management
- Unstable patients or those with multiple comorbidities should be admitted to the intensive care unit (ICU).
- Hemodynamic monitoring, volume resuscitation, and stabilization should be implemented.
- The patient should be kept nil per os (NPO).
- Total parenteral nutrition should be initiated.
- Intravenous broad-spectrum antibiotics and antifungals should be administered.
- Intravenous proton pump inhibitors can be initiated.
- Percutaneous drainage of any fluid collections should be performed.
- The need for operative versus nonoperative management should be assessed.
- A feeding jejunostomy tube may be considered.
Standard Care of Management
- Endoscopic stent placement: Endoscopic stent placement can be an effective nonsurgical option for selected stable patients. Stents cover esophageal perforations, facilitating defect healing. However, potential complications include stent migration, malpositioning, or failure to seal the defect adequately.
- Drainage with or without debridement: Surgical drainage, sometimes accompanied by debridement, is essential for managing contamination and preventing infection spread. In many cases, adequate drainage allows the perforation to heal without additional surgical intervention.
Surgical Management
Surgical intervention is often necessary, particularly in cases with extensive contamination, significant tissue necrosis, or delayed diagnosis.
- Primary repair with debridement: For patients diagnosed within 24 hours of perforation, debridement of all devitalized tissue followed by primary repair of the esophageal defect is often feasible. This repair is typically reinforced with a vascularized pedicle flap, such as the serratus anterior, latissimus dorsi, or diaphragm, to support healing.
- Emergent surgical stenting, debridement, or drainage: In cases of extensive leakage, significant necrosis, or large fluid collections, emergent surgical intervention is required. This may involve the placement of a stent, additional debridement, or extensive drainage to restore esophageal integrity and prevent further complications.
- Esophageal diversion or resection: In severe cases where primary repair is not feasible due to extensive contamination, tissue friability, or preexisting esophageal disease (eg, inoperable malignancy), diversion procedures or esophageal resection may be necessary. This involves creating a proximal esophagostomy and a feeding gastrostomy or jejunostomy to bypass the esophagus while allowing nutritional support.
- Feeding jejunostomy or gastrostomy: Postoperative healing may be supported by placing a feeding jejunostomy or gastrostomy tube, which allows the esophagus to rest while ensuring the patient receives adequate nutrition. This is particularly important in cases with substantial extraluminal leakage.
- Oral feeding and follow-up: Oral feeding is typically resumed once the patient is stable, and a contrast esophagram study confirms the integrity of the esophagus and the absence of any leakage.
Differential Diagnosis
The differential diagnoses for esophageal perforations and tears include:
- Acute aortic dissection
- Acute coronary syndrome
- Acute pericarditis
- Aspiration pneumonitis and pneumonia
- Bacterial pneumonia
- Emergent management of pancreatitis
- Empyema and abscess pneumonia
- Mallory-Weiss tear
- Myocardial infarction
- Peptic ulcer disease
- Pneumothorax
- Pulmonary embolism
Prognosis
The prognosis of esophageal perforations and tears remains guarded due to the high morbidity and mortality associated with the condition. Despite advancements in surgical and nonsurgical management, outcomes are heavily influenced by several critical factors. Timing of diagnosis and intervention is paramount; early detection and prompt treatment are essential in reducing mortality, as delays significantly increase the risk of severe complications such as sepsis, mediastinitis, and multiorgan failure. The underlying cause of the perforation also plays a crucial role, with perforations resulting from malignant conditions or extensive necrosis generally having poorer prognoses due to the challenges of successful repair. Additionally, the expertise of the treatment center is vital, as high-volume centers with specialized teams tend to achieve better outcomes. This underscores the importance of experience and multidisciplinary care in managing these complex cases.
Surgical intervention, including esophagectomy, primary repair, or surgical drainage, is often required to manage esophageal perforations effectively. Studies by Veziant et al, Singh and Rizk, and Nassour and Fang have demonstrated that while these surgical strategies can be life-saving, they are also associated with significant risks. For instance, esophagectomy, which may be necessary in cases of extensive damage or malignancy, is linked to high postoperative morbidity and mortality, particularly within the first 90 days after surgery.[17][18][19] Veziant et al's analysis of European data from 2012 to 2021 highlighted that high-volume centers—those managing more than 8 cases of esophageal perforation annually—reported better outcomes, with fewer deaths among patients experiencing complications within 90 days of the perforation.[17] This suggests that experience and specialized care can significantly impact patient survival and recovery.
Minimally invasive techniques, such as esophageal stenting and endoscopic procedures, have been explored as alternatives to open surgery. However, these approaches come with challenges. Although less invasive, esophageal stenting carries risks, including stent migration and misplacement, which can lead to further complications. Reviews by Schmitz et al, Brinster et al, and Axtell et al have highlighted these issues, emphasizing the importance of careful patient selection and technique refinement to improve outcomes.[20][21][22]
Endoscopic vacuum therapy (EVT) is an emerging treatment modality for esophageal perforations that offers a promising organ-preserving alternative. EVT has demonstrated particular effectiveness in cases of iatrogenic perforations, Boerhaave syndrome, and other nonsurgical upper gastrointestinal causes. Initial studies report a success rate of 89%, highlighting its potential as a less invasive option compared to traditional surgical methods. As experience with EVT increases and its indications are refined, it is anticipated to become a more widely adopted treatment, potentially improving outcomes for patients with esophageal perforations.[23]
Despite advances in surgical techniques, minimally invasive approaches, and novel therapies such as EVT, esophageal perforations continue to be associated with significant morbidity and mortality. Achieving optimal outcomes necessitates early diagnosis, careful patient selection for appropriate treatments, and management at specialized centers with expertise in esophageal perforations. Ongoing research and refinement of these approaches are crucial for improving long-term prognosis and patient outcomes in this life-threatening condition.
Complications
If left untreated, esophageal perforation can result in several serious complications, including:
- Pneumothorax
- Pleural effusion
- Mediastinitis
- Infection
- Septicemia
- Subcutaneous emphysema
- Necrosis
- Shock
- Death
Deterrence and Patient Education
Deterrence and patient education are essential in reducing the risk of esophageal perforations and tears, especially given the difficulty in preventing these rare but serious injuries. Although complete prevention may not always be feasible, educating patients about the risks and symptoms associated with esophageal perforations can significantly improve outcomes by encouraging timely medical intervention.
Patients who have recently undergone esophageal surgery or had a tube placed in their esophagus should be informed about the potential symptoms of perforation, including chest pain, difficulty swallowing, or breathing problems. They should understand the importance of seeking immediate medical attention if they experience these symptoms or suspect an esophageal perforation. Early detection and prompt treatment are crucial in reducing the risk of severe complications and improving prognosis, making patient awareness a critical factor in managing this condition effectively.
Educating patients on the importance of communication with their healthcare providers and ensuring they are aware of the signs to watch for can be crucial in preventing delays in diagnosis and intervention, ultimately leading to better outcomes in cases of esophageal perforations and tears.
Pearls and Other Issues
A systematic review underscored several critical findings: many cases were diagnosed after a delay of more than 24 hours, mortality rates exceeded 10%, and there was no clear consensus on the best therapeutic and diagnostic approaches.[10]
Enhancing Healthcare Team Outcomes
Managing esophageal perforations and tears requires high skill, strategic planning, and effective interprofessional communication. Physicians, advanced practitioners, nurses, pharmacists, and other healthcare professionals must collaborate to deliver patient-centered care that optimizes outcomes and ensures patient safety. Each healthcare team member plays a crucial role, from early recognition and diagnosis to implementing appropriate treatment strategies. Physicians and advanced practitioners are responsible for diagnosing and planning treatment, while nurses monitor patient status, administer medications, and provide critical bedside care. Pharmacists ensure the appropriate selection and dosing of antibiotics and other medications, thereby minimizing the risk of complications such as sepsis.
Effective communication and care coordination among all healthcare teams are essential for enhancing team performance and patient outcomes. Regular multidisciplinary meetings and clear, timely communication channels ensure that everyone involved in the patient's care is updated on the current treatment plan and any changes. This coordinated approach improves the quality of care and minimizes the risk of errors and treatment delays, which are crucial for managing the high-risk nature of esophageal perforations and tears. By fostering a culture of collaboration and continuous communication, the healthcare team enhances patient outcomes, promotes safety, and ensures the highest standard of care in these complex cases.
Media
References
Younes Z, Johnson DA. The spectrum of spontaneous and iatrogenic esophageal injury: perforations, Mallory-Weiss tears, and hematomas. Journal of clinical gastroenterology. 1999 Dec:29(4):306-17 [PubMed PMID: 10599632]
White RK, Morris DM. Diagnosis and management of esophageal perforations. The American surgeon. 1992 Feb:58(2):112-9 [PubMed PMID: 1550302]
Level 2 (mid-level) evidenceBadertscher P, Delko T, Oertli D, Reuthebuch O, Schurr U, Pradella M, Kühne M, Sticherling C, Osswald S. Surgical repair of an esophageal perforation after radiofrequency catheter ablation for atrial fibrillation. Indian pacing and electrophysiology journal. 2019 May-Jun:19(3):110-113. doi: 10.1016/j.ipej.2019.01.004. Epub 2019 Jan 24 [PubMed PMID: 30685314]
Level 3 (low-level) evidenceDudzinski DM, Mangalmurti SS, Oetgen WJ. Characterization of Medical Professional Liability Risks Associated With Transesophageal Echocardiography. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2019 Mar:32(3):359-364. doi: 10.1016/j.echo.2018.11.003. Epub 2019 Jan 21 [PubMed PMID: 30679140]
Zhong S, Wu Z, Wang Z. Successful Treatment of Fishbone-Induced Esophageal Perforation and Mediastinal Abscess: A Case Report and Literature Review. The American journal of case reports. 2023 Dec 18:24():e942056. doi: 10.12659/AJCR.942056. Epub 2023 Dec 18 [PubMed PMID: 38105546]
Level 3 (low-level) evidenceHuu Vinh V, Viet Dang Quang N, Van Khoi N. Surgical management of esophageal perforation: role of primary closure. Asian cardiovascular & thoracic annals. 2019 Mar:27(3):192-198. doi: 10.1177/0218492319827439. Epub 2019 Jan 21 [PubMed PMID: 30665318]
Onodera Y, Nakano T, Fukutomi T, Naitoh T, Unno M, Shibata C, Kamei T. Thoracoscopic Esophagectomy for a Patient With Perforated Esophageal Epiphrenic Diverticulum After Kidney Transplantation: A Case Report. Transplantation proceedings. 2018 Dec:50(10):3964-3967. doi: 10.1016/j.transproceed.2018.08.042. Epub 2018 Sep 8 [PubMed PMID: 30577297]
Level 3 (low-level) evidenceGhiselli A, Bizzarri B, Ferrari D, Manzali E, Gaiani F, Fornaroli F, Nouvenne A, Di Mario F, De'Angelis GL. Endoscopic dilation in pediatric esophageal strictures: a literature review. Acta bio-medica : Atenei Parmensis. 2018 Dec 17:89(8-S):27-32. doi: 10.23750/abm.v89i8-S.7862. Epub 2018 Dec 17 [PubMed PMID: 30561414]
Susai CJ, Banks KC, Alcasid NJ, Velotta JB. A clinical review of spontaneous pneumomediastinum. Mediastinum (Hong Kong, China). 2024:8():4. doi: 10.21037/med-23-25. Epub 2023 Oct 27 [PubMed PMID: 38322193]
Sdralis EIK, Petousis S, Rashid F, Lorenzi B, Charalabopoulos A. Epidemiology, diagnosis, and management of esophageal perforations: systematic review. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2017 Aug 1:30(8):1-6. doi: 10.1093/dote/dox013. Epub [PubMed PMID: 28575240]
Level 1 (high-level) evidenceDanielian SN, Tarabrin EA, Rabadanov KM, Barmina TG, Kvardakova OV, Khachatryan SA. [Post-intubation rupture of thoracic trachea in a patient with iatrogenic esophageal perforation and mediastinitis]. Khirurgiia. 2023:(1):89-93. doi: 10.17116/hirurgia202301189. Epub [PubMed PMID: 36583499]
Andrási K, Stankovics P, Kecskés L. [Diagnosis and treatment of traumatic esophageal perforation.]. Orvosi hetilap. 2023 Oct 29:164(43):1719-1724. doi: 10.1556/650.2023.32859. Epub 2023 Oct 29 [PubMed PMID: 37898911]
Milosavljevic T, Popovic D, Zec S, Krstic M, Mijac D. Accuracy and Pitfalls in the Assessment of Early Gastrointestinal Lesions. Digestive diseases (Basel, Switzerland). 2019:37(5):364-373. doi: 10.1159/000495849. Epub 2018 Dec 12 [PubMed PMID: 30540998]
Kupeli M, Dogan A. Successful Treatment of a Late Diagnosed Esophageal Perforation with Mediastinitis and Pericardial Abscess. Journal of the College of Physicians and Surgeons--Pakistan : JCPSP. 2018 Dec:28(12):972-973. doi: 10.29271/jcpsp.2018.12.972. Epub [PubMed PMID: 30501839]
Aiolfi A, Ferrari D, Riva CG, Toti F, Bonitta G, Bonavina L. Esophageal foreign bodies in adults: systematic review of the literature. Scandinavian journal of gastroenterology. 2018 Oct-Nov:53(10-11):1171-1178. doi: 10.1080/00365521.2018.1526317. Epub 2018 Nov 5 [PubMed PMID: 30394140]
Level 1 (high-level) evidenceWatkins JR, Farivar AS. Endoluminal Therapies for Esophageal Perforations and Leaks. Thoracic surgery clinics. 2018 Nov:28(4):541-554. doi: 10.1016/j.thorsurg.2018.07.002. Epub [PubMed PMID: 30268300]
Veziant J, Boudis F, Lenne X, Bruandet A, Eveno C, Nuytens F, Piessen G. Outcomes Associated With Esophageal Perforation Management: Results From a French Nationwide Population-based Cohort Study. Annals of surgery. 2023 Nov 1:278(5):709-716. doi: 10.1097/SLA.0000000000006048. Epub 2023 Jul 27 [PubMed PMID: 37497641]
Singh NP, Rizk JG. Oesophageal perforation following ingestion of over-the-counter ibuprofen capsules. The Journal of laryngology and otology. 2008 Aug:122(8):864-6. doi: 10.1017/S0022215108002582. Epub 2008 May 1 [PubMed PMID: 18452637]
Nassour I, Fang SH. Gastrointestinal perforation. JAMA surgery. 2015 Feb:150(2):177-8. doi: 10.1001/jamasurg.2014.358. Epub [PubMed PMID: 25549241]
Schmitz RJ, Sharma P, Badr AS, Qamar MT, Weston AP. Incidence and management of esophageal stricture formation, ulcer bleeding, perforation, and massive hematoma formation from sclerotherapy versus band ligation. The American journal of gastroenterology. 2001 Feb:96(2):437-41 [PubMed PMID: 11232687]
Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. The Annals of thoracic surgery. 2004 Apr:77(4):1475-83 [PubMed PMID: 15063302]
Axtell AL, Gaissert HA, Morse CR, Premkumar A, Schumacher L, Muniappan A, Ott H, Allan JS, Lanuti M, Mathisen DJ, Wright CD. Management and outcomes of esophageal perforation. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2022 Jan 7:35(1):. pii: doab039. doi: 10.1093/dote/doab039. Epub [PubMed PMID: 34212186]
Luttikhold J, Pattynama LMD, Seewald S, Groth S, Morell BK, Gutschow CA, Ida S, Nilsson M, Eshuis WJ, Pouw RE. Endoscopic vacuum therapy for esophageal perforation: a multicenter retrospective cohort study. Endoscopy. 2023 Sep:55(9):859-864. doi: 10.1055/a-2042-6707. Epub 2023 Feb 24 [PubMed PMID: 36828030]
Level 2 (mid-level) evidence