Introduction
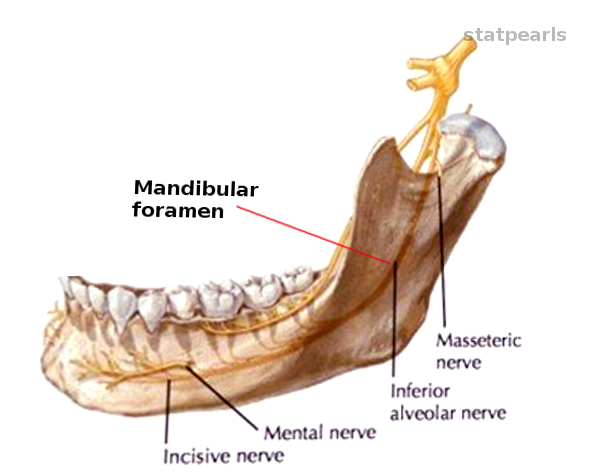
The maxilla and mandible bones create the opening of the mouth. The maxilla comprises the upper jaw while the lower jaw is from the mandible. These two bones work in sync for speaking, eating, and facial expression. The mandible is the only bone in the skull that is mobile. The mandible elevates and depresses during the actions of eating, speaking, and facial expression. The mandible bone has most of its vital structures enclosed in the mandibular foramen.
The words "mandibular foramen," equate to an opening/canal in the mandible bone. The foramen is designed to protect vessels and nerves as they travel toward their final destination. These vital structures are necessary for nerve innervation and blood supply to the skin, bone, teeth, gums, muscles, and tissues that attach to the mandible and the tissues bordering the mandible.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The mandibular foramen is a bony canal formed within the mandible. This bony canal opens on the inner side of the mandibular ramus. The opening is directly inferior to the mandibular notch and ends at the mental foramen. The foramen follows the shape of the mandible. The canal starts inferior to the mandibular notch and descends until it's slightly superior to the angle of the mandible. At the point superior to the angle of the mandible, the canal will make a turn towards the anterior chin region. After the canal makes the turn, it will travel and end at the mental foramen, which is slightly lateral to the anterior chin region. The mandibular foramen contains a branch of the trigeminal nerve (CN V), a branch of the maxillary artery and the inferior alveolar vein. The nerve and blood vessels within the mandibular foramen are the inferior alveolar nerve, artery, and vein. The inferior alveolar nerve is responsible for innervation of the gums, dental sockets, and mandible. The inferior alveolar artery is the dominant blood supply to the mandible, gums, teeth, and nerves in the lower jaw. The inferior alveolar vein is responsible for the venous drainage of the mandible and tissues that are nearby.
Once the mandibular foramen ends at the mental foramen, the inferior alveolar nerve and artery will become the mental nerve and artery. On the outer medial surface of the mandibular foramen, there is a groove called the mylohyoid fossa. This fossa is designed for the mylohyoid nerve (branch of the inferior alveolar nerve) as it travels toward the mylohyoid muscle.[1]
Embryology
The development of the mandible originates from the branchial apparatus. The branchial apparatus divides into three main components. The components are the branchial clefts, arches, and pouches. The branchial clefts are made up of ectoderm. The only significant branchial cleft is the first one. This first branchial cleft will develop into the external acoustic meatus. The composition of the branchial arches is of neural crest cells and mesoderm. The branchial arches are responsible for developing into the muscles, bones, and nerves of the face and neck. While the branchial pouches will develop into the organs in the face and neck such as the tonsils, parathyroid, and thymus. Simultaneously, the arterial system in the head, face, and neck will develop from the aortic arches; the aortic arches will differentiate around the same time as the structures from the branchial apparatus.
The first branchial arch will form the mandible. The grooves and impressions in the mandible will develop as the other tissues differentiate. As the inferior alveolar nerve and artery develop and travel toward the oral cavity, the mandibular foramen will develop. The mandibular foramen will form to protect the inferior alveolar nerve and vessels.
Blood Supply and Lymphatics
The dominant blood supply to the mandible derives from the inferior alveolar artery. The inferior alveolar artery travels within the mandibular foramen. As the inferior alveolar artery travels within the mandibular foramen, it will perfuse the mandible. The inferior alveolar vein is the venous drainage system for the mandible.
The lymphatic drainage of the mandible directs toward the submental or the submandibular lymph nodes. These lymph nodes will eventually drain their contents back into the central circulation via the right lymphatic duct or the thoracic duct. The thoracic duct will empty the lymph fluid from the left side of the mandible while the right lymphatic duct will drain the lymph fluid from the right side of the mandible.
Nerves
The mandibular foramen will house and protect the inferior alveolar nerve. This nerve provides innervation to the gums, dental sockets, and teeth. The inferior alveolar nerve innervates the anterior chin and lower lip via the mental nerve. The inferior alveolar nerve also innervates the mylohyoid muscle and the anterior muscle belly of the digastric muscle via the mylohyoid nerve. The mylohyoid nerve travels in the mylohyoid fossa on the medial surface of the mandibular foramen.
Muscles
The mandibular foramen does not contain any muscles. But the inferior alveolar nerve and vessels within the mandibular foramen are associated with muscles in the face and neck.
Physiologic Variants
The shape of the mandibular foramen may vary depending on its contents. The mandibular foramen's location, thickness, and length are dependent on the inferior alveolar nerve and artery.[2][3] The shape of the orifice of the mandibular foramen can be circular or even V-shaped in some individuals. The mandibular foramen vary depending on the age of the person also. The opening of the mandibular foramen is generally more superior in the ramus of the mandible in adults. In contrast, the mandibular foramen is located lower in the mandible in children.[4] In some cases, the mandibular foramen was found to have an extra canal. The extra foramen is called the accessory mandibular foramen. This extra foramen is present in individuals with bifid inferior alveolar nerves. The location of the accessory mandibular foramen is inferior to the primary mandibular foramen. In rarer variations, there are three mental foramina as the endpoint of the mandibular foramen.[5][6] These variations can be found and confirmed on radiographic imaging.[7][8][9][10]
Surgical Considerations
In dental and jaw surgery, the knowledge of the mandibular foramen is crucial. Knowing that the mandibular foramen houses the inferior alveolar nerve and vessels is important in avoiding unwanted complications. For example, the inferior alveolar nerve can become damaged during dental extractions or implantation of the third molar tooth.[11][12] In jaw reconstruction, if the mandibular foramen undergoes reconstruction and the contents get damaged, it could lead to ischemia and sensory loss to the areas innervated by the inferior alveolar nerve and perfused by the inferior alveolar artery.[13]
Clinical Significance
The clinical importance of the mandibular foramen comes into play for nerve blocks. The inferior alveolar nerve is commonly a target for blocking during dental procedures.[14][15] The location the inferior alveolar nerve block is usually before it enters the mandibular foramen. The landmarks for the inferior alveolar nerve block is the pterygomandibular raphe and the coronoid notch.[7] The local anesthetic is usually injected between these two structures to successful numb the sensory territory of the inferior alveolar nerve. In nerve blocking of the inferior alveolar nerve, the clinician should account for the age of the patient due to the location variation of the nerve in adults and children.[4] Also, it is important to account for the possible variations, such as when there are multiple inferior alveolar nerves. Using radiographic imaging, the clinician can confirm the presences of multiple mandibular foramina, since the number of mandibular foramina corresponds to the number of inferior alveolar nerves. This approach ensures a proper and successful nerve block that would anesthetize the entire region innervated by the inferior alveolar nerve.
Other Issues
Any conditions that affect the mandible has the potential to compromise the mandibular foramen and its contents. The mandible may become affected by osteonecrosis. Osteonecrosis of the jaw includes necrosis of the mandible. This condition typically affects individuals taking bisphosphonates prophylactically to prevent bone loss. Bisphosphonates have a side effect that results in osteonecrosis of the mandible.[16] Osteonecrosis can also occur from other medications such as disease-modifying antirheumatic drugs.[17] Osteonecrosis can also affect people who undergo dental implantation or extractions.
The inferior alveolar nerve and artery can be compressed within the mandibular foramen if the lumen of the foramen becomes narrowed. Compression of the inferior alveolar nerve leads to sensory deficits. While the compression of the inferior alveolar artery can lead to ischemia. The narrowing can be due to neoplasms, hematomas, and other pathologies infiltrating within the lumen of the mandibular foramen.[3][18][19]
Media
References
Toth J, Lappin SL. Anatomy, Head and Neck, Mylohyoid Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 31424877]
Al-Shayyab MH, Qabba'ah K, Alsoleihat F, Baqain ZH. Age and gender variations in the cone-beam computed tomographic location of mandibular canal: Implications for mandibular sagittal split osteotomy. Medicina oral, patologia oral y cirugia bucal. 2019 Jul 1:24(4):e545-e554. doi: 10.4317/medoral.22969. Epub 2019 Jul 1 [PubMed PMID: 31232390]
Friedrich RE, Matschke J, Wilczak W. Unilaterally Enlarged Mandibular Foramina and Canal Associated With Hyperplastic Lymphatic Tissue of Inferior Alveolar Nerve: Case Report and Short Literature Survey. Anticancer research. 2019 Aug:39(8):3991-4002. doi: 10.21873/anticanres.13554. Epub [PubMed PMID: 31366480]
Level 3 (low-level) evidenceHwang TJ, Hsu SC, Huang QF, Guo MK. [Age changes in location of mandibular foramen]. Zhonghua ya yi xue hui za zhi. 1990 Sep:9(3):98-103 [PubMed PMID: 2135997]
Predoiu M, Rusu MC, Chiriţă AL. A rare anatomic variation: Triple mental foramina. Morphologie : bulletin de l'Association des anatomistes. 2019 Jun:103(341 Pt 2):110-115. doi: 10.1016/j.morpho.2019.04.004. Epub 2019 May 15 [PubMed PMID: 31103465]
Lam M, Koong C, Kruger E, Tennant M. Prevalence of Accessory Mental Foramina: A Study of 4,000 CBCT Scans. Clinical anatomy (New York, N.Y.). 2019 Nov:32(8):1048-1052. doi: 10.1002/ca.23434. Epub 2019 Jul 25 [PubMed PMID: 31301240]
Thangavelu K, Kannan R, Kumar NS, Rethish E, Sabitha S, Sayeeganesh N. Significance of localization of mandibular foramen in an inferior alveolar nerve block. Journal of natural science, biology, and medicine. 2012 Jul:3(2):156-60. doi: 10.4103/0976-9668.101896. Epub [PubMed PMID: 23225978]
Subramanian B, Anthony SN, Mubbunu L, Hachombwa C, Mlawa MS, Majambo MM, Sasi RM. Anthropometrics Analysis of Mental Foramen and Accessory Mental Foramen in Zambian Adult Human Mandibles. TheScientificWorldJournal. 2019:2019():9093474. doi: 10.1155/2019/9093474. Epub 2019 Jul 16 [PubMed PMID: 31379470]
Kalabalik F, Aytuğar E. Localization of the Mandibular Canal in a Turkish Population: a Retrospective Cone-Beam Computed Tomography Study. Journal of oral & maxillofacial research. 2019 Apr-Jun:10(2):e2. doi: 10.5037/jomr.2019.10202. Epub 2019 Jun 30 [PubMed PMID: 31404191]
Level 2 (mid-level) evidenceCosta ED, Peyneau PD, Visconti MA, Devito KL, Ambrosano GMB, Verner FS. Double mandibular canal and triple mental foramina: detection of multiple anatomical variations in a single patient. General dentistry. 2019 Sep-Oct:67(5):46-49 [PubMed PMID: 31454322]
Qi W, Lei J, Liu YN, Li JN, Pan J, Yu GY. Evaluating the risk of post-extraction inferior alveolar nerve injury through the relative position of the lower third molar root and inferior alveolar canal. International journal of oral and maxillofacial surgery. 2019 Dec:48(12):1577-1583. doi: 10.1016/j.ijom.2019.07.008. Epub 2019 Jul 28 [PubMed PMID: 31362896]
Level 2 (mid-level) evidenceKang F, Sah MK, Fei G. Determining the risk relationship associated with inferior alveolar nerve injury following removal of mandibular third molar teeth: A systematic review. Journal of stomatology, oral and maxillofacial surgery. 2020 Feb:121(1):63-69. doi: 10.1016/j.jormas.2019.06.010. Epub 2019 Aug 30 [PubMed PMID: 31476533]
Level 1 (high-level) evidenceShen H, Wang S, Zhi Y, Si J, Shi J. Effects of inferior alveolar nerve rupture on bone remodeling of the mandible: A preliminary study. Medicine. 2019 Aug:98(35):e16897. doi: 10.1097/MD.0000000000016897. Epub [PubMed PMID: 31464921]
Kommineni M, Kuchimanchi PK, Koneru G, Sanikommu S. A Simplified Single-Penetration Technique of IANB (MK Technique) for Mandibular Anesthesia. Journal of maxillofacial and oral surgery. 2019 Sep:18(3):459-465. doi: 10.1007/s12663-018-1169-1. Epub 2018 Oct 29 [PubMed PMID: 31371891]
Kojima Y, Murouchi T, Akiba M, Oka T. Ultrasound-guided inferior alveolar nerve block for postoperative analgesia after mandibular sequestrectomy: A single-center retrospective study. Journal of clinical anesthesia. 2020 Mar:60():39-40. doi: 10.1016/j.jclinane.2019.08.026. Epub 2019 Aug 20 [PubMed PMID: 31442855]
Level 2 (mid-level) evidenceSoares AL, Simon S, Gebrim LH, Nazário ACP, Lazaretti-Castro M. Prevalence and risk factors of medication-related osteonecrosis of the jaw in osteoporotic and breast cancer patients: a cross-sectional study. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2020 May:28(5):2265-2271. doi: 10.1007/s00520-019-05044-0. Epub 2019 Aug 29 [PubMed PMID: 31468192]
Level 2 (mid-level) evidenceBrijs K, Miclotte I, Vermeire S, Darche V, Politis C. Osteonecrosis of the jaw in patients with inflammatory bowel disease treated with tumour necrosis factor alpha inhibitors. International journal of oral and maxillofacial surgery. 2020 Mar:49(3):317-324. doi: 10.1016/j.ijom.2019.08.007. Epub 2019 Aug 27 [PubMed PMID: 31466830]
Fujita M, Hirokawa Y, Naito K, Tagashira N, Yajin K, Wada T. Recurrent lower gingival squamous cell carcinoma spreading along the pathway of the inferior alveolar nerve. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 1995 Sep:80(3):369-75 [PubMed PMID: 7489283]
Level 3 (low-level) evidenceRazak A, Goh BS, Rajaran JR, Nazimi AJ. Numb chin syndrome: an ominous sign of mandibular metastasis. BMJ case reports. 2018 May 14:2018():. pii: bcr-2017-223586. doi: 10.1136/bcr-2017-223586. Epub 2018 May 14 [PubMed PMID: 29764822]
Level 3 (low-level) evidence