Introduction
Trichofolliculoma is a cutaneous adnexal tumor derived from the hair follicle. Trichofolliculomas, sometimes called folliculomas, are a category of benign hair follicle tumors comprising a diverse group of uncommon neoplasms. The specific type and extent of hair follicle differentiation distinguish each neoplasm. Several examples of more widely documented benign hair follicle tumors include trichilemmoma, trichoadenoma, dilated pore of Winer, and trichoblastoma [1].
Trichofolliculomas are considered hamartomatous neoplasms rather than cancerous. Trichofolliculomas generally are characterized by well-differentiated cells without atypical features that display abnormal tissue arrangement.[2] More specifically, trichofolliculomas manifest a cystic dilation of one or multiple infundibula with a centralized opening to the skin surface, through which one or more hair shafts pass.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Numerous genetic abnormalities have been documented in cutaneous adnexal tumors. However, outside of experimental models, no clearly identified mutations or genetic predispositions have been implicated in the formation of trichofolliculoma. One animal-based study suggested a mutation in genes encoding for bone morphogenetic proteins (BMPs) and pygopus homolog 2 (PYGO2) may be associated with trichofolliculoma; this has not yet been substantiated in human subjects or reproduced in subsequent studies. Trichofolliculoma is a rare condition with an as-yet undefined etiology.[3]
Epidemiology
Trichofolliculoma typically manifests as a solitary nodule on the face or scalp in adulthood. Numerous case series and retrospective analyses have suggested that the incidence of trichofolliculoma is highest among middle-aged adults. However, trichofolliculoma can occur across a broad age spectrum, with infrequent instances reported in children and older people.
In a case series involving 11 individuals with trichofolliculoma, the mean age at diagnosis was 46 years, ranging from 20 to 75 years.[4] While no apparent gender predilection has been established, some studies suggest there may be a slight male preponderance.[3] Furthermore, no specific racial or ethnic predisposition has been identified using available evidence.
While there have been several documented cases of congenital trichofolliculoma, these lesions typically arise spontaneously and lack any recognized connections with systemic or dermatologic syndromes.[5]
Histopathology
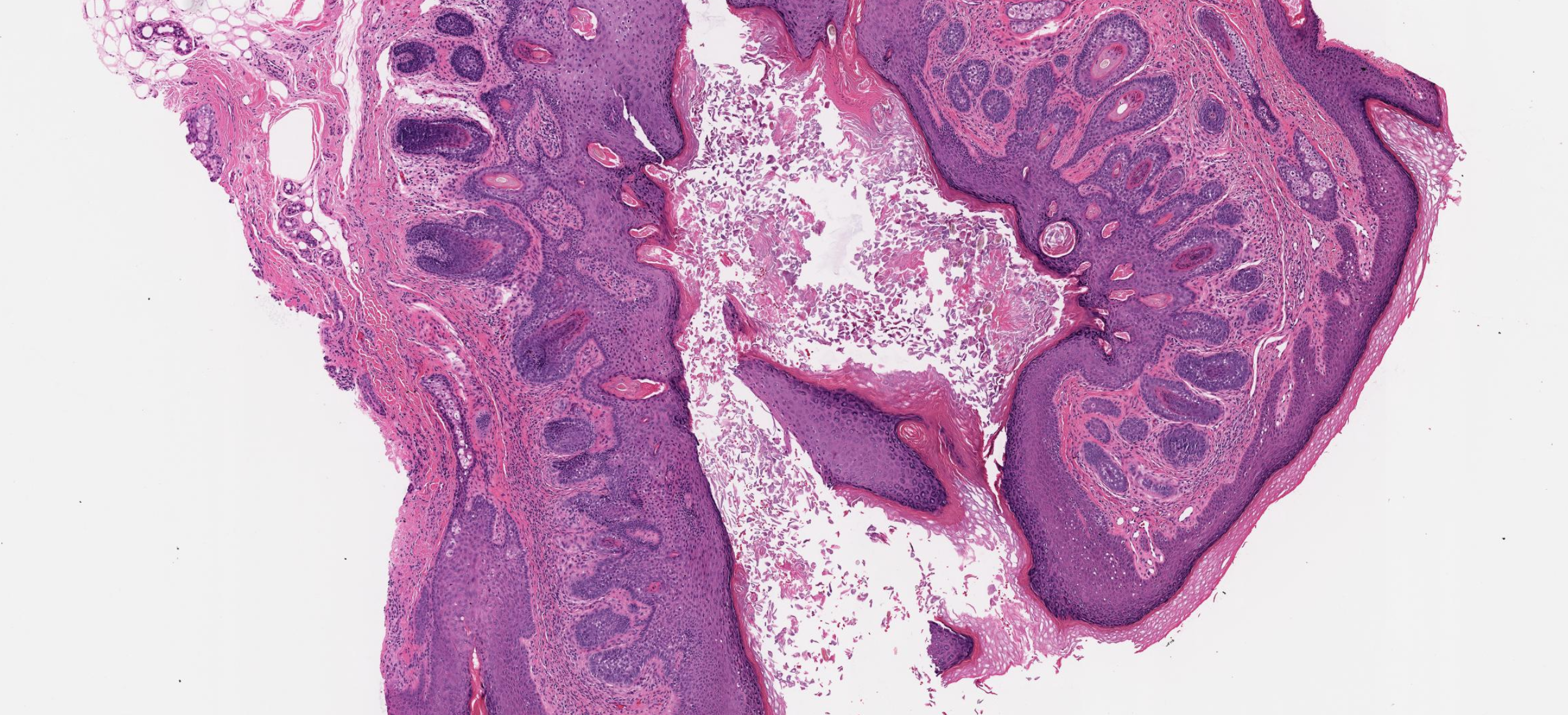
Classically, trichofolliculoma is distinguished by a prominently dilated primary follicle lined by stratified squamous epithelium originating from the infundibulum. The primary follicle typically exhibits differentiation of the outer root sheath and features keratinized epithelium with a granular layer and keratohyalin granules. (see Image. Trichofolliculoma Pathologic Specimen)
However, the histological appearance of trichofolliculoma can vary based on the stage of evolution of the lesion. Trichofolliculoma initially presents as slight infundibular widening with curved vellus follicles and often lacks marked cystic dilation. However, a thin-walled cystic structure originating from the primary infundibulum will be seen in advanced stages.[6] Extending radially from this central configuration is a multitude of well-differentiated vellus follicles, each with an associated bulb, papilla, and an inner and outer sheath layer. These follicles can display varying degrees of maturation and contain hairs in anagen, catagen, or telogen phases. A distinctive stroma parallel to the perifollicular sheath with vascular and fibrous composition encompasses the complete structure.[2]
Sebaceous trichofolliculoma is a subtype of trichofolliculoma initially characterized by Plewig in 1980.[7] Aside from a yellowish hue, the clinical presentation does not notably differ from nonsebaceous lesions. However, this variant exhibits prominent sebaceous follicles joined with a central channel or sinus.[8] The hair follicles that extend radially are commonly sectioned tangentially, leading to substantial microscopic variability. Consequently, obtaining deeper tissue sections from the specimen may be necessary for an accurate diagnosis. In instances where the follicles are observed to coexist with sebaceous glands, the corresponding hamartoma can be designated as a sebaceous trichofolliculoma [9]. However, this additional diagnostic terminology does not hold any significant clinical relevance. Whether a lesion is designated as a classic trichofolliculoma or specified as a sebaceous trichofolliculoma, there are no documented changes in behavior, and management recommendations remain unchanged [10].
On histological evaluation, trichofolliculoma presents as a basaloid follicular neoplasm. Alternative pathological conditions that should be considered in the histological differential diagnosis include trichoepithelioma, fibrofolliculoma, hair follicle nevus, pilar sheath acanthoma, trichoadenoma, and basal cell carcinoma.[11] Immunohistochemical staining may be employed to clarify the diagnosis.[3]
While there is no standard guideline for immunohistological staining, the primary follicles of trichofolliculoma demonstrate expression of CD34; pleckstrin homology-like domain, family A, member 1 protein (PHLDA1); and cytokeratin (CK) 10, 15, and 17. Staining for CK 17 is particularly prominent. Additionally, the secondary follicles have demonstrated expression of CK 14. PHLDA1 is a marker for epithelial follicular stem cells. CD34 is a widely recognized marker for hematopoietic stem cells, commonly expressed in spindle-shaped cells located within the central region of intact hair follicles.[11]
In scenarios where the pathologist or dermatologist is attempting to differentiate between benign follicular tumors and basal cell carcinoma histologically, a stain for CD34 or PHLDA1 may be useful. When the histological differential diagnosis includes basal cell carcinoma, a tissue sample staining positive for PHLDA1 would suggest the diagnosis of a follicular hair tumor such as trichoblastoma, trichofolliculoma, and trichoepithelioma to be more likely.[3] One study demonstrated that CD34 expression by benign follicular tumors is significantly higher than in basal cell carcinoma, as basal cell carcinomas are more commonly CD34-negative.[11]
History and Physical
The vast majority of trichofolliculomas have been described as painless, solitary, dome-shaped papules, with only isolated reports documenting the presence of multiple lesions.[12] Trichofolliculomas most commonly occur on the central face, scalp, and neck. The typical presentation is a skin-colored papule with a smooth surface containing an enlarged central pore, from which multiple fine, vellus hairs emerge.[1]
Nevertheless, several investigations have proposed that clinically apparent central hair is only observed in a minority of trichofolliculoma cases and generally correlates with the presence of numerous secondary vellus hair follicles on histology. A comprehensive study examining 90 cases of trichofolliculoma highlighted that the prevailing clinical manifestation was a solid papule or nodule, averaging 7 mm in diameter. A central pit was identified in only 15.5% of cases, and visible hair tufts were observed in only 12.2%. Nearly 40% of trichofolliculomas were in the nasal region, 15% on the cheek, and approximately 12% on the ear. Only four cases were documented in locations other than the facial region.[4]
There are scattered reports of trichofolliculomas on the lips, intranasal cavity, external auditory canal, and upper extremities.[12]
Evaluation
Evaluation of trichofolliculoma begins with obtaining a comprehensive medical history and performing a thorough physical examination. A trichofolliculoma classically presents as a painless, slow-growing papule on the face of an adult with a tuft of light-colored hair protruding from a central punctum. Aside from histopathologic examination via skin biopsy, no specific laboratory, radiographic, or other diagnostic evaluations are routinely ordered for patients with suspected trichofolliculoma. Many genetic aberrations have been identified in many of the adnexal neoplasms; however, no specific mutations have been linked to the development of trichofolliculoma at this time. Furthermore, there are no known associated genetic syndromes or systemic symptoms.[3]
Dermoscopic evaluation of a suspected trichofolliculoma can be useful; data regarding the dermoscopic appearance of trichofolliculoma is limited due to the sparse number of cases reported since dermoscopy has become a more widely used diagnostic tool.[13] When reviewing the limited dermoscopic descriptions in the literature, the most frequently recurring dermoscopic findings of trichofolliculoma were a “firework pattern” with a central punctum and the “troll doll sign.”[14] The firework pattern refers to a central tan-colored zone with multiple, radially oriented peripheral projections of dark brown with no pigment networks or prominent vascularization.[15] A lesion demonstrating the dermoscopic troll doll sign is a shapeless pink neoplasm with multiple clusters of smooth white vellus hairs and resembles the distinctive hair of a troll doll.[16]
Ultimately, the diagnosis of trichofolliculoma is confirmed by histological evaluation, which is typically necessary due to the clinical similarities to basal cell carcinoma and other follicular tumors. Histopathological features may overlap, and immunohistochemical staining may be employed to clarify the diagnosis.[3]
Treatment / Management
A biopsy is often necessary for diagnostic confirmation of trichofolliculoma and to definitively rule out neoplasms of malignant behavior. However, after the diagnosis of trichofolliculoma has been established, conservative management is generally advised, and no further treatment is required.[17][3]
Simple excision may be considered for cosmesis or if the lesion is in sensitive areas. Other treatment options can include curettage or electrodesiccation. Due to limited data, there are currently no standard practice guidelines for managing trichofolliculoma.[3]
Differential Diagnosis
There can be a large crossover in clinical and histological appearance among various cutaneous neoplasms. The diagnosis of trichofolliculoma can often be established based on clinical findings alone in cases with characteristic features. However, there are instances where there is no appreciable central indentation or hair plug on physical examination; this can pose a significant clinical diagnostic challenge.[4]
Several benign conditions in the clinical differential diagnosis of trichofolliculoma are melanocytic nevus, epidermoid cyst, trichoepithelioma, fibrofolliculoma, and neurofollicular hamartoma.[5] Establishing a diagnosis of trichofolliculoma can be particularly challenging in cases where the patient has forcefully removed the central hair before the evaluation; this may distort the morphology and further broaden the clinical differential to include keratoacanthoma, sebaceous hyperplasia, molluscum contagiosum, milium, syringoma, or basal cell carcinoma.[18] As the differential diagnosis for trichofolliculoma can be expansive and includes several lesions with malignant potential, such as squamous and basal cell carcinoma, definitive diagnosis typically requires biopsy and subsequent histological evaluation.[6]
Prognosis
Trichofolliculomas are hamartomatous growths of the hair follicle, and as with all hamartomas, trichofolliculomas are generally considered benign, slow-growing, and self-limited neoplasms.[19] The prognosis for trichofolliculoma is excellent even when left untreated, and no treatment is required.[20] There has only been one reported case of trichofolliculoma with perineural invasion; no documented cases of malignant transformation or distant metastasis have been reported.[21]
Complications
There have been numerous documented cases of local trichofolliculoma recurrence when intervention is limited to biopsy; recurrence was not associated with any increase in morbidity or mortality.[22] If excised with confirmed negative margins, the likelihood of trichofolliculoma recurring is reportedly low.[3] As with any skin biopsy or excision, there is always the risk of scarring, bleeding, pain, infection, or nerve damage.
Deterrence and Patient Education
Trichofolliculoma is often discovered in individuals with no history of similar lesions. No clearly identified risk factors, associated genetic syndromes, or systemic findings exist. The underlying etiology and pathophysiology of trichofolliculoma have not yet been elucidated.[3] Consequently, there are no specific screening recommendations or known prevention methods.
Any individual who develops a new skin growth of unknown behavior should be advised to seek a dermatological evaluation. Once the diagnosis has been histologically confirmed as trichofolliculoma, patients can be reassured regarding the benign nature of the condition; if there are cosmetic or functional considerations, various removal methods are available.[17]
Enhancing Healthcare Team Outcomes
The healthcare practitioner and patient should know that trichofolliculomas are benign lesions that do not require treatment. Nonetheless, obtaining accurate diagnoses based on clinicopathologic correlation is crucial for determining appropriate management and avoiding unnecessary interventions. Histopathologic evaluation plays a vital role in diagnosing cutaneous adnexal tumors like trichofolliculoma due to their resemblance to malignancies such as basal cell carcinoma. Particular attention should be given to trichofolliculomas located in sensitive areas like the eyelid, as referral to oculoplastic surgery may be necessary to address cosmetic and functional concerns.[17]
Open communication amongst all healthcare team members, including advanced practice providers and clinical staff, and interprofessional collaboration across pertinent specialties such as primary care, dermatology, pathology, and plastic surgery is essential for ensuring safe and effective treatment and optimizing patient outcomes.
Media
(Click Image to Enlarge)
References
Tellechea O, Cardoso JC, Reis JP, Ramos L, Gameiro AR, Coutinho I, Baptista AP. Benign follicular tumors. Anais brasileiros de dermatologia. 2015 Nov-Dec:90(6):780-96; quiz 797-8. doi: 10.1590/abd1806-4841.20154114. Epub [PubMed PMID: 26734858]
Patel P, Nawrocki S, Hinther K, Khachemoune A. Trichoblastomas Mimicking Basal Cell Carcinoma: The Importance of Identification and Differentiation. Cureus. 2020 May 25:12(5):e8272. doi: 10.7759/cureus.8272. Epub 2020 May 25 [PubMed PMID: 32596088]
Płachta I, Kleibert M, Czarnecka AM, Spałek M, Szumera-Ciećkiewicz A, Rutkowski P. Current Diagnosis and Treatment Options for Cutaneous Adnexal Neoplasms with Follicular Differentiation. International journal of molecular sciences. 2021 Apr 30:22(9):. doi: 10.3390/ijms22094759. Epub 2021 Apr 30 [PubMed PMID: 33946233]
Massara B, Sellami K, Graja S, Boudaouara O, Miladi S, Hammami F, Bahloul E, Boudaouara T, Turki H. Trichofolliculoma: A Case Series. The Journal of clinical and aesthetic dermatology. 2023 Mar:16(3):41-43 [PubMed PMID: 36950043]
Level 2 (mid-level) evidenceRomero-Pérez D, García-Bustinduy M, Cribier B. Clinicopathologic study of 90 cases of trichofolliculoma. Journal of the European Academy of Dermatology and Venereology : JEADV. 2017 Mar:31(3):e141-e142. doi: 10.1111/jdv.13960. Epub 2016 Sep 18 [PubMed PMID: 27608202]
Level 3 (low-level) evidenceAbdelbary A, Shakshouk H. Trichofolliculoma Mimicking Squamous Cell Carcinoma. Dermatology practical & conceptual. 2022 Feb:12(1):e2022026. doi: 10.5826/dpc.1201a26. Epub 2022 Jan 1 [PubMed PMID: 35223170]
Lei JH, Shen H. Sebaceous Trichofolliculoma of the Scrotum: A Rare Occurrence. Indian journal of dermatology. 2022 Sep-Oct:67(5):625. doi: 10.4103/ijd.ijd_1056_20. Epub [PubMed PMID: 36865871]
Al-Ghadeer H, Edward DP. Congenital Sebaceous Trichofolliculoma of the Upper Eyelid. Ophthalmic plastic and reconstructive surgery. 2017 May/Jun:33(3S Suppl 1):S60-S61. doi: 10.1097/IOP.0000000000000698. Epub [PubMed PMID: 27097063]
Monteiro MB, Mesquita-Guimarães J, Ramos S. [Sebaceous trichofolliculoma]. Medicina cutanea ibero-latino-americana. 1987:15(3):205-7 [PubMed PMID: 3312863]
Level 3 (low-level) evidencePlewig G. Sebaceous trichofolliculoma. Journal of cutaneous pathology. 1980 Dec:7(6):394-403 [PubMed PMID: 7451702]
Level 3 (low-level) evidenceSengul D, Sengul I, Astarci MH, Ustun H, Mocan G. Differential diagnosis of basal cell carcinoma and benign tumors of cutaneous appendages originating from hair follicles by using CD34. Asian Pacific journal of cancer prevention : APJCP. 2010:11(6):1615-9 [PubMed PMID: 21338206]
Choi CM, Lew BL, Sim WY. Multiple trichofolliculomas on unusual sites: a case report and review of the literature. International journal of dermatology. 2013 Jan:52(1):87-9. doi: 10.1111/j.1365-4632.2011.05120.x. Epub 2012 May 29 [PubMed PMID: 22640019]
Level 3 (low-level) evidenceYélamos O, Braun RP, Liopyris K, Wolner ZJ, Kerl K, Gerami P, Marghoob AA. Usefulness of dermoscopy to improve the clinical and histopathologic diagnosis of skin cancers. Journal of the American Academy of Dermatology. 2019 Feb:80(2):365-377. doi: 10.1016/j.jaad.2018.07.072. Epub 2018 Oct 13 [PubMed PMID: 30321580]
Karaarslan I, Oraloglu G, Yaman B. In vivo reflectance confocal microscopic findings in a case of trichofolliculoma. Anais brasileiros de dermatologia. 2022 Mar-Apr:97(2):236-239. doi: 10.1016/j.abd.2021.05.013. Epub 2022 Jan 14 [PubMed PMID: 35039208]
Level 3 (low-level) evidenceLai M, Muscianese M, Piana S, Chester J, Borsari S, Paolino G, Pellacani G, Longo C, Pampena R. Dermoscopy of cutaneous adnexal tumours: a systematic review of the literature. Journal of the European Academy of Dermatology and Venereology : JEADV. 2022 Sep:36(9):1524-1540. doi: 10.1111/jdv.18210. Epub 2022 May 25 [PubMed PMID: 35536546]
Level 1 (high-level) evidenceShah KM, Der Sarkissian SA, Cheung K, Sebaratnam DF. Trichofolliculoma - 'troll hair' dermoscopy. The Australasian journal of dermatology. 2021 Feb:62(1):90-92. doi: 10.1111/ajd.13459. Epub 2020 Sep 11 [PubMed PMID: 32914875]
Varde MA, Heindl LM, Kakkassery V. [Diagnosis and treatment of benign eyelid tumors]. Die Ophthalmologie. 2023 Mar:120(3):240-251. doi: 10.1007/s00347-022-01798-x. Epub 2023 Feb 10 [PubMed PMID: 36763162]
Garcia-Garcia SC, Villarreal-Martinez A, Guerrero-Gonzalez GA, Miranda-Maldonado I, Ocampo-Candiani J. Dermoscopy of trichofolliculoma: a rare hair follicle hamartoma. Journal of the European Academy of Dermatology and Venereology : JEADV. 2017 Feb:31(2):e123-e124. doi: 10.1111/jdv.13870. Epub 2016 Aug 9 [PubMed PMID: 27504964]
Pe'er J. Pathology of eyelid tumors. Indian journal of ophthalmology. 2016 Mar:64(3):177-90. doi: 10.4103/0301-4738.181752. Epub [PubMed PMID: 27146927]
Gokalp H, Gurer MA, Alan S. Trichofolliculoma: a rare variant of hair follicle hamartoma. Dermatology online journal. 2013 Aug 15:19(8):19264 [PubMed PMID: 24021443]
Level 3 (low-level) evidenceStern JB, Stout DA. Trichofolliculoma showing perineural invasion. Trichofolliculocarcinoma? Archives of dermatology. 1979 Aug:115(8):1003-4 [PubMed PMID: 464613]
Level 3 (low-level) evidenceNayak SU, Shenoi SD, Geetha V, Prabhu S, Nagel B. Multiple trichofolliculomas mimicking multiple trichoepitheliomas. Indian journal of dermatology. 2015 Mar-Apr:60(2):214. doi: 10.4103/0019-5154.152591. Epub [PubMed PMID: 25814743]