Introduction
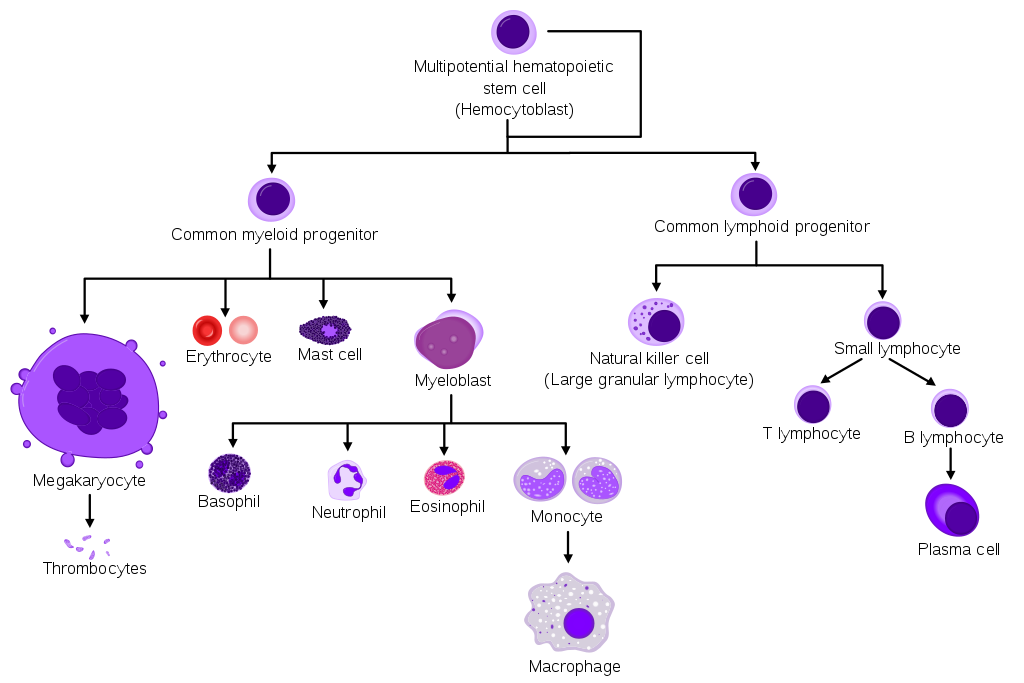
The production of abnormal leukocytes defines leukemia as either a primary or secondary process. They can be classified as acute or chronic based on the rapidity of proliferation and myeloid or lymphoid based on the cell of origin. Predominant subtypes are acute myeloid leukemia (AML) and chronic myeloid leukemia (CML), involving the myeloid lineage; acute lymphoblastic leukemia (ALL); and chronic lymphocytic leukemia (CLL), involving the lymphoid chain. Other less common variants, such as mature B-cell and T-cell leukemias, and NK cell-related leukemias, to name a few, arise from mature white blood cells. However, with the advent of next-generation sequencing (NGS) and the identification of various biomarkers, the World Health Organization (WHO) classification was updated in 2016, bringing multiple changes to the traditional classification for acute leukemias and myeloid neoplasms.[1] GLOBOCAN, a global observatory for cancer trends, showed a global incidence of 474,519 cases, with 67,784 in North America. The Age-Standardized Rates are around 11 per 100,000, with a mortality rate of approximately 3.2.[2]
Many genetic risk factors have been identified, such as Klinefelter and Down syndromes, ataxia telangiectasia, Bloom syndrome, and telomeropathies such as Fanconi anemia, dyskeratosis congenita, and Shwachman-Diamond syndrome; germline mutations in RUNX1, CEBPA, to name a few. Viral infections associated with Epstein Barr virus, human T-lymphotropic virus, ionizing radiation exposure, radiation therapy, environmental exposure with benzene, smoking history, history of chemotherapy with alkylating agents, and topoisomerase II agents have also been implicated in the development of acute leukemias. Symptoms are nonspecific and can include fever, fatigue, weight loss, bone pain, bruising, or bleeding. Definitive diagnoses often require bone marrow biopsy, the results of which help the hematologists and stem cell transplant physicians regarding the selection of treatment options ranging from chemotherapy to allogeneic stem cell transplantation. The prognosis is variable depending on the leukemia subtype in question.
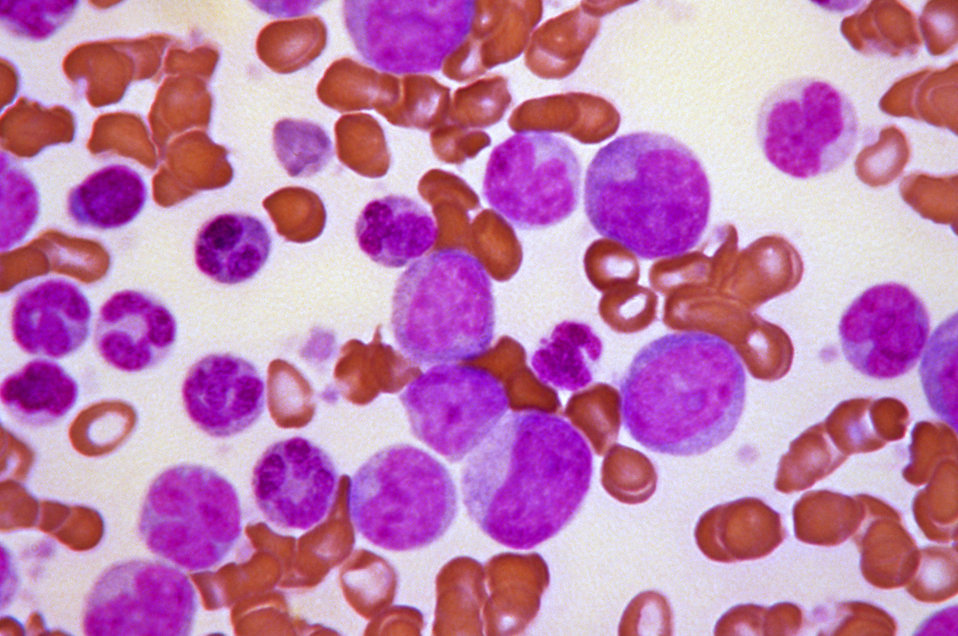
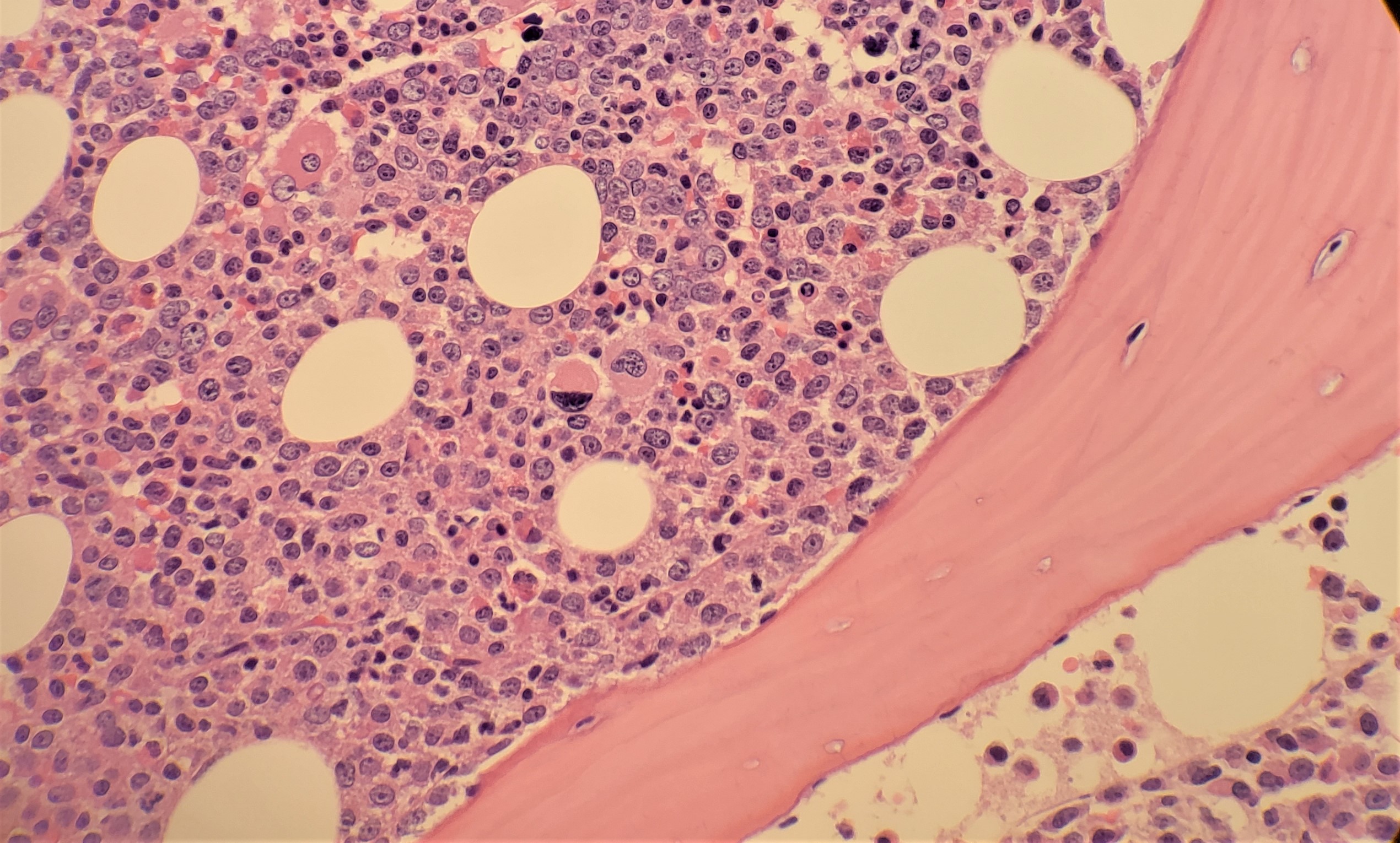
Acute vs. chronic myeloid leukemia: Blasts, which are immature and dysfunctional cells, normally make up 1% to 5% of marrow cells. Acute leukemias are characterized by greater than 20% blasts in the peripheral blood smear or on bone marrow leading to a more rapid onset of symptoms. In contrast, chronic leukemia has less than 20% blasts with a relatively chronic onset of symptoms. The accelerated/blast phase is a transformation of chronic myeloid leukemia into an acute phase with a significantly higher degree of blasts.[1][3][4]
As such, the four major subtypes of leukemia are:
- Acute lymphoblastic leukemia (ALL): ALL is seen in patients with the blastic transformation of B and T cells. It is the most common leukemia in the pediatric population, accounting for up to 80% of cases in this group vs. 20% of cases in adults. Treatment among adolescents and young adults is predominantly inspired by pediatric regimens with better survival rates.
- Acute myelogenous leukemia (AML): AML is characterized by greater than 20% myeloid blasts and is the most common acute leukemia in adults. It is the most aggressive cancer with a variable prognosis depending upon the molecular subtypes.
- Chronic lymphocytic leukemia (CLL): CLL occurs from the proliferation of monoclonal lymphoid cells. Most cases occur in people between the ages of 60 and 70. CLL is considered an indolent disease, for the most part, meaning not all patients with a diagnosis will need to start treatment until symptomatic from the disease.
- Chronic myelogenous leukemia (CML): CML typically arises from reciprocal translocation and fusion of BCR on chromosome 22 and ABL1 on chromosome 9, resulting in dysregulated tyrosine kinase on chromosome 22 called the Philadelphia (Ph) chromosome. This, in turn, causes a monoclonal population of dysfunctional granulocytes, predominantly neutrophils, basophils, and eosinophils.[1][3][5][6]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Multiple genetic and environmental risk factors are identified in the development of leukemia.
- Exposure to ionizing radiation is associated with an increased risk of multiple leukemia subtypes.[7][8]
- Exposure to benzene is a risk factor for leukemia in adults, particularly AML.[9]
- Previous exposure to chemotherapy, especially alkylating agents and topoisomerase II inhibitors, increases the risk for acute leukemia later in life.[7][8]
- A history of any hematologic malignancy is a risk factor for subsequently developing another subtype of leukemia.[10]
- Viral infections (e.g., human T-cell leukemia virus, Epstein Barr virus) are linked with subtypes of ALL.[11]
- Several genetic syndromes (e.g., Down syndrome, Fanconi anemia, Bloom syndrome, Li-Fraumeni syndrome) are associated with an increased risk of AML and ALL.[12]
Epidemiology
GLOBOCAN, which is a global observatory for cancer trends, showed a global incidence of 474,519 cases, with 67,784 in North America. The age-standardized rates are around 11 per 100,000, with a mortality rate of about 3.2. ALL and AML, which are important diseases in both childhood and adulthood, have bimodal age distributions, with CML and CLL mostly in the older age groups. According to the Surveillance, Epidemiology, and End Results (SEER) database, there are 61,090 estimated new cases of leukemia in 2021, accounting for 3.2% of all new cancer cases, making leukemia the 10th most common cancer in the United States. Estimated deaths are about 23,660, which comprises 3.9% of all cancer deaths. Since 2006, the incidence of the disease has increased by an average of 0.6% per year, while the mortality has decreased by an annual average of 1.5%.[6][7]
Pathophysiology
Leukemia occurs due to the malignant transformation of pluripotent (i.e., it can give rise to both myeloid and lymphoid precursors) hematopoietic stem cells. Rarely, it can also involve a more committed stem cell with limited self-renewal capacity. In acute leukemias, these malignant cells are generally immature, poorly differentiated, abnormal leukocytes (blasts) that can either be lymphoblasts or myeloblasts. These blasts can undergo clonal expansion and proliferation, leading to replacement and interference with the development and function of normal blood cells, leading to clinical symptoms.
Acute Leukemia
In ALL, chromosomal translocation or abnormal chromosome numbers can lead to mutations in precursor lymphoid cells leading to lymphoblasts. Common mutations include t(12;21) and t(9;22). In AML, chromosomal translocations, rearrangements, and gain or loss of chromosomes can lead to mutations and abnormal production of myeloblasts. One important translocation is t(15;17), which leads to the fusion of retinoic acid receptor alpha (RARA) and a promyelocytic leukemia transcription factor (PML). This leads to the development of acute promyelocytic leukemia, which can present with hallmarks of disseminated intravascular coagulation and need emergent treatment with all-trans retinoic acid.
Chronic Leukemia
Chromosomal abnormalities in hematopoietic stem cells that are precursors to leucocytes are the most common cause of chronic leukemia. Examples of abnormalities are deletions, translocations, or extra chromosomes. In CML, mutations mainly affect granulocytes (most commonly the t(9;22) translocation), and in CLL, they primarily affect lymphocytes (especially B lymphocytes). Unlike acute leukemias, in chronic leukemias, cells are partially mature. These partially mature cells do not function effectively and divide too quickly. They accumulate in the peripheral blood and lymphoid organs, which can lead to anemia and thrombocytopenia, and leukopenia.
Histopathology
Acute Leukemia
In acute leukemia, the peripheral blood or bone marrow is characterized by more than 20% blasts. However, regardless of the blast percentage, patients with t(8;21)(q22;q22), RUNX1-RUNX1T1, inv(16)(p13.1q22) or t(16;16)(p13.1;q22), CBFB-MYH11 or t(15;17)(q24.1;q21.1), PML-RARA, are considered and treated as acute leukemia. There is usually increased cellularity noted on bone marrow biopsy that is packed with blasts and a variable number of granulocytic or monocytic cells and erythroid precursors. Traditional markers included in the evaluation are CD7, CD11b, CD13, CD14, CD15, CD16, CD33, CD34, CD45, CD56, CD117, HLA-DR. Also, either peripheral smear or bone marrow aspirate is sent for a mutation panel of multiple genes with therapeutic and prognostic implications, such as ASXL1, CEBPA, DNMT3A, FLT3, IDH1, IDH2, NPM1, RUNX1, and TP53, to mention a few.
There is also increased bone marrow cellularity in ALL, composed of B and T lymphoblasts (with small nucleoli, dispersed chromatin, cleaved and irregular nuclei with undetectable cytoplasm). Common T-cell lymphoid immunostains include TdT, CD2, CD3, CD5, and CD7. Common B-cell lymphoid immunostains include HLA-DR, CD10, CD19, CD22, CD79a, PAX5, and CD20. There should not be any myeloid markers, such as myeloperoxidase (MPO), to confirm the diagnosis of the pure lymphoid lineage. Mixed phenotype acute leukemia (MPAL) has both myeloid and lymphoid markers but is a rare entity. Cytogenetics evaluation for Ph chromosome status and Ph-like translocation is a must as newer therapeutic agents are now incorporated into treatment algorithms.[13]
Chronic Leukemia
The white blood cell count in chronic leukemia is often elevated, with a smear suggestive of significant left shift/granulocyte predominance. Such a picture is commonly seen during the acute illness phase, but if such a picture persists upon repeat labs, CML should be evaluated. In CML, the translocation t(9;22) can be diagnosed by fluorescence in-situ hybridization (FISH) on peripheral blood. Bone marrow biopsy is not necessary for diagnosis, but if done, it will usually show 100% cellular marrow with increased granulocyte precursors, basophils, eosinophils, and occasional monocytes.
In CLL, the white cell count is elevated, with mostly CD5+ and CD23+ B-lymphocytes. The clonal lymphocyte population has to be greater than 5,000/mcL for diagnosis. If the clonal lymphocyte population is less than 5,000/mcL, the entity is termed monoclonal B cell lymphocytosis of undetermined significance. Flow cytometry is often diagnostic. Patients would need evaluation for del(17p) and TP53 mutation status, immunoglobulin heavy chain variable region (IGHV) gene mutation status, del(11q), del(13q), and trisomy 12 evaluation, which can help in selecting appropriate treatment regimens.[14]
History and Physical
Acute Leukemia
Acute leukemia tends to present non-specifically, although the most common presenting features include fever, lethargy, and bleeding. Hepatosplenomegaly, lymphadenopathy, and musculoskeletal symptoms (especially involving the spine and long bones) can also be clues to the diagnosis. Adults may also have more prominent anemia-related symptoms, such as shortness of breath, or symptoms related to thrombocytopenia, such as excessive bruising or increased bleeding tendency. Patients with acute promyelocytic leukemia (APL), which is associated with disseminated intravascular coagulation-type symptoms, can present with mucosal bleeding, including gum bleeds, nosebleeds, or menorrhagia.
Chronic Leukemia
Chronic leukemia subtypes occur almost exclusively in adults. Many patients are asymptomatic at the time of diagnosis, identified only incidentally after marked leukocytosis is discovered on a complete blood count (CBC) performed for another reason. Hepatosplenomegaly and lymphadenopathy can be appreciated in some cases, while bleeding and bruising are less common, presenting features relative to acute leukemia subtypes.[15]
Evaluation
The workup of leukemia is very involved, and multiple tests are needed to confirm a diagnosis and, subsequently, to stage the disease. Helpful initial studies include a CBC, comprehensive metabolic panel, liver function tests (LFT), and coagulation panel, which are often followed by a peripheral blood smear evaluation and a bone marrow biopsy and aspiration.
On rare occasions, leukemia can be diagnosed on histology alone. For example, AML is characterized by the presence of Auer rods (red-staining, needle-like bodies seen in the cytoplasm of myeloblasts) on a peripheral smear. In most other cases, more detailed analyses with flow cytometry, cytogenetics, and FISH testing are required to distinguish between subtypes.[16]
A bone marrow aspiration and biopsy are often required for the diagnosis of acute leukemias. For chronic leukemias, peripheral blood evaluation is often enough, and an invasive bone marrow biopsy may not be needed. For example, CML can be diagnosed by looking for BCR-ABL fusion protein on peripheral blood FISH analysis. CLL can be diagnosed by looking for a monoclonal B-cell population through peripheral blood flow cytometry.
Treatment / Management
Patients with leukemia should be referred to a hematologist-oncologist to initiate treatment. Therapy varies significantly based on the leukemia subtype and patient factors (e.g., age, comorbid conditions). Acute leukemias are treated predominantly as an in-patient needing significant support, frequent monitoring of vitals, and assessment for opportunistic infections and electrolyte imbalances. The predominant challenge at the time of diagnosis of acute myeloid leukemia is to identify the possibility of APL, which has a significantly different treatment compared to the rest of AML.
APL: APL patients typically present with bleeding diathesis with increased coagulation parameters (elevated PT, aPTT) and low fibrinogen. Peripheral smear shows a predominance of myeloid blasts with Auer rods. It is important to start the treatment with ATRA (all-trans-retinoic acid) when APL is suspected rather than awaiting confirmatory tests with FISH. ATRA advances arrested promyeloblasts into becoming mature granulocytes which can result in differentiation syndrome.[17] Differentiation syndrome is seen during 48 hours of ATRA initiation to even three weeks from starting therapy for APL. Patients have a fever, respiratory distress with acute pulmonary infiltration on imaging, and capillary leak resulting in edema. It can mimic sepsis, resulting in delaying the treatment with dexamethasone. The commonly accepted starting dosage is 10mg every 12 hours till improvement in symptoms and counts.[18] Other significant complication with ATRA includes raised intracranial pressure leading to headaches and significant vision changes from papilledema.
Specific treatment for APL depends on whether the patient is at low or intermediate risk (also known as standard risk) with a WBC count <10,000/ mcL or high risk with a WBC count >10,000/ mcL. Low or intermediate-risk APL is further differentiated by platelets above or below 40,000/mcL.
- Standard-risk APL: Patients respond well to ATRA and arsenic trioxide (ATO) with lesser complications during induction and recovery without needing an allogeneic stem cell transplant (SCT). During the utilization of ATO, patients need to be monitored for electrolyte changes closely and electrocardiogram for QTc prolongation changes(Framingham formula).[19]
- High-risk APL: Along with ATRA + ATO, high-risk patients achieve better responses with the addition of idarubicin.[20] Recent studies have included CD33-targeted drug conjugate, gemtuzumab ozogamicin (GO), during the induction therapy combined with ATRA + ATO.[21]
APL patients have better overall survival and prognosis than other types of AML without needing a transplant.
AML: Standard therapy for AML is well known as the '7+3' regimen, which includes a 7-day course of cytarabine continuous infusion with a 3-day course of an anthracycline (either daunorubicin or idarubicin). With the advent of cytogenetics and NGS testing, patients are now being risk-stratified based on the molecular markers resulting in prognostic and therapeutic implications.[22] The outline of therapy based on the risk status per ELN (European LeukemiaNet) is as follows
(A1)| Risk status | Cytogenetics | Treatment |
| Favorable risk | t(8;21)(q22;q22.1); inv(16) or t(16;16)Mutated NPM1 without FLT3-ITD or with FLT3-ITDlowBiallelic mutated CEBPA |
Standard 7+3 regimen with/without GO.[23] This chemo regimen can be attempted in patients > 60 years old if they have good tolerability as determined by performance status. Patients who achieve complete response can complete consolidation without the obvious need for SCT unless patients relapse. |
| Intermediate risk | Mutated NPM1 and FLT3-ITD highWild type NPM1 without FLT3-ITD or with FLT3-ITD low (without adverse-risk genetic abnormalities)t(9;11)(p21.3;q23.3); MLLT3-KMT2ACytogenetic abnormalities not classified as favorable or adverse |
Standard 7 + 3 with FLT3 tyrosine kinase inhibitor (midostaurin) during induction and consolidation.[24] Strongly consider SCT among this risk group.
For patients above 60 years or with intermediate performance status Hypomethylating agents (HMA) with/without B-cell lymphoma-2 (BCL-2) inhibitor - venetoclax.[25]
Therapy-related AML or AML arising from antecedent myelodysplastic syndrome or Chronic myelomonocytic leukemia Patients respond better with liposomal cytarabine and daunorubicin, which is a category 1 indication in NCCN guidelines.[26] |
| Adverse risk | t(6;9)(p23;q34.1); DEK-NUP214t(v;11q23.3); KMT2A rearrangedt(9;22)(q34.1;q11.2); BCR-ABL1inv(3)(q21.3q26.2) or t(3;3)(q21.3;q26.2); GATA2,MECOM(EVI1) –5 or del(5q); –7; –17/abn(17p)Complex karyotype,◊ monosomal karyotype§Wild type NPM1 and FLT3-ITDhighMutated RUNX1Mutated ASXL1Mutated TP53 | Clinical trials preferred |
ALL
ALL is divided into B or T lymphocyte variants based on the lymphoblast origin and the presence of >20% lymphoblasts in peripheral smear or BM. The presence or absence of the Ph chromosome is the most important molecular marker leading to therapeutic implications in treating ALL.
(A1)| Ph status | Treatment regimen |
| Ph-positive ALL |
Combination of chemotherapy with oral tyrosine kinase inhibitor (TKI) favorably 2nd generation and beyond such as dasatinib, ponatinib, bosutinib, nilotinib, and imatinib. Not all the TKI combinations have data with chemotherapy agents, and the availability of the drug and provider practices generally dictate the regimen. For patients in adolescent and young adult (AYA) age groups (around 15 to 40 years), pediatric-inspired chemotherapy regimens with peg-asparaginase (Berlin-Frankfurt-Münster regimen) are favored when patients can tolerate treatment. Other chemotherapy options for patients <65 years old include hyper-fractionated CVAD( cyclophosphamide, vincristine sulfate, doxorubicin, and dexamethasone), alternating with high-dose methotrexate and cytarabine, and newer therapy with bispecific CD19-directed CD3 T-cell engager blinatumomab.[27][28][29] For patients >65 years old, TKI backbone combined with corticosteroids with/without vincristine or lower dose hyperCVAD in robust patients can be tried.[30][28][30] Recently a chemotherapy-free induction and consolidation regimen using dasatinib with blinatumomab yielded good responses and improved survival outcomes.[29] |
| Ph negative ALL |
Chemotherapy forms the predominant backbone in Ph-negative patients without any role for TKIs. Multiple chemotherapy regimens are adapted based on the age of the patient. In AYA age groups, predominant use of peg-asparaginase-based regimens such as CALGB 10403, COG AALL0434, DCFI ALL regimen, etc.[31][32][33] For patients less than 65 years old, rituximab-based regimens in CD20-positive patients, such as GRAALL-2005 [34], CALGB 8811, and hyperCVAD, as mentioned prior, are utilized. For older patients, based on their performance status, corticosteroids with/without vincristine, POMP regimen (prednisolone, vincristine, methotrexate, and 6-mercaptopurine), and lower dose hyperCVAD therapy are options.[35] |
The overall outcome depends upon the patient's response to induction therapy and the presence or absence of MRD (minimal residual disease) needing further therapies and BMT.
CML: CML is one of the first cancers revolutionized by utilizing targeted therapy with Ph chromosome targeting TKIs. Patients have a significant response to TKIs, negating the need for acute chemotherapy unless they are in an accelerated phase/blast crisis. A patient's risk can be assessed based on multiple available calculators such as the Sokal score, EUTOS Score, and EUTOS long-term survival score (ELTS).[36][37][38] For patients having high-risk disease, second-generation (nilotinib, dasatinib, and bosutinib) TKIs are utilized as first-line therapy to achieve the therapy milestones faster with deeper responses.[39] For low and intermediate-risk patients, imatinib can be initiated as first-line therapy. However, there is no significant difference in overall survival based on the generation of the TKI used. (B2)
Major milestones after initiation of TKI include:
- At 3 months: BCR-ABL1 [International Scale (IS)] at ≤10 percent and/or ≤35% Ph-positive metaphase cells
- At 6 months: BCR-ABL1 (IS) at ≤1 percent or/and 0 % Ph-positive metaphase cells
- At 1 year : BCR-ABL1 (IS) ≤0.1 percent
Patients need to be monitored for resistance mutations, predominantly T315I mutation, for which ponatinib, asciminib, and omacetaxine are approved.[40][41] Patients might continue to develop resistance to multiple TKIs for whom SCT can be attempted. (A1)
CLL: CLL runs its course in a more indolent fashion than all the other leukemic subtypes, with the patient's lifespan minimally impacted by the disease. Patients do not benefit from early treatment unless they meet the criteria for therapy. Patients with a rapid doubling time of lymphocytes, worsening cytopenias, increasing spleen size causing abdominal discomfort, and significant B symptoms (fatigue, night sweats, and weight loss) benefit from treatment. The most important determinant in treating CLL is knowing the IGVH mutation status and the presence of del17p and TP53 mutation. t(11:14) is often obtained to rule out mantle cell lymphoma.
For patients with IGVH mutation who have a relatively good prognosis, chemotherapy with FCR (fludarabine, cyclophosphamide, rituximab)[42] or BR (bendamustine, rituximab)[43] can be attempted as patients would be able to achieve prolonged disease-free survival for over ten years. For high-risk patients with del17p / TP53 mutation, patients benefit significantly from targeted therapy with venetoclax (BCL-2 inhibitor) or Bruton's tyrosine kinase (BTK) inhibitors (ibrutinib, acalabrutinib), either as a single agent or in combination with rituximab or obinutuzumab.[44][45][46][47] Older patients with comorbidities tolerate BTK inhibitors better.(A1)
Rarely do patients with CLL/SLL who have a dormant course present with acute aggressive lymphadenopathy. They need an urgent lymph node or bone marrow biopsy to rule out Richter transformation into aggressive diffuse large B cell lymphoma and rarely Hodgkin lymphoma or T cell lymphomas.
Differential Diagnosis
The differential diagnosis is broad because leukemia is a broad diagnosis with non-specific symptoms. One must rule out infection, drug effects, vitamin/micronutrient deficiencies, and other myelodysplastic disorders that can cause abnormalities in blood cell lines.
Consider the following when seeing abnormalities in the blood count:
- B12 and folate deficiencies
- Copper deficiencies
- Viral infections (e.g., HIV, cytomegalovirus, Epstein-Barr virus)
- Drugs (chemotherapeutic agents, valproic acid, ganciclovir, mycophenolate mofetil)
- Autoimmune conditions (e.g., systemic lupus erythematosus)
Prognosis
Long-term survival with leukemia varies tremendously based on leukemia subtype, cytogenetic and molecular findings, patient age, and comorbid conditions. Broadly, leukemia's 5-year cancer survival rate increased from 33% in 1975 to 59% in 2005.[6]
Complications
Tumor Lysis Syndrome (TLS)
TLS is a complication of chemotherapy that can result when tumor cells die quickly. The widespread cellular destruction releases intracellular contents into the bloodstream overwhelming the kidneys and resulting in dangerously high serum levels of potassium, phosphorus, and uric acid.[48] Patients need aggressive hydration, frequent lab monitoring, and management of hyperuricemia with allopurinol and rasburicase. Hyperkalemia and hypocalcemia can lead to significant cardiac toxicity requiring urgent correction.
Disseminated Intravascular Coagulation (DIC)
DIC is a complication of leukemia itself in which the proteins that control the blood clotting process become dysfunctional, leading to both thrombosis and hemorrhage. DIC is often associated with acute promyelocytic leukemia but can be seen in other subtypes of leukemia as well.[16]. Frequent lab monitoring with active replacement of fibrinogen with cryoprecipitate is vital to the patient's survival.
Infection
Immunosuppression from chemotherapy, stem cell transplantation, or leukemia itself increases the risk of dangerous infections. Fever with neutropenia in an immunosuppressed patient should prompt an immediate evaluation for infection source and the initiation of broad-spectrum antibiotic therapy.[49]
Cancer
Survivors of leukemia are at an increased risk of subsequent cancers. For example, the Childhood Cancer Survivor Study demonstrated that the 30-year cumulative incidence of any cancer after leukemia was 5.6%; the median time to occurrence of the subsequent cancer was nine years. The most common second neoplasms in childhood leukemia survivors are different subtypes of leukemia or lymphoma.[10]
Deterrence and Patient Education
Leukemia is the production of abnormal white blood cells from bone marrow and lymphatic tissues. Excess production of such white blood cells affects the production of normal blood cells, which are essential to fight infections, carry oxygen, and help clot blood. Such abnormal cell production can be fast, making it acute leukemia or a relatively slower process leading to chronic leukemia. Common symptoms include recurrent infections, weight loss, fatigue, fevers, abdominal pain, and bleeding. Multiple types of leukemias are present, and they require evaluation by a hematologist for further guidance on treatment.
Enhancing Healthcare Team Outcomes
Acute and chronic leukemias are heterogeneous hematologic diseases with complex diagnostic and therapeutic implications requiring an interprofessional healthcare team. The involvement of healthcare professionals from across specialties and disciplines - clinicians, nurses, specialists (especially hematologists and oncologists), nurses, pharmacists, nutritionists, etc. - is needed to achieve effective management, mitigate adverse events, and ensure their quality of life.
The patient's initial encounter will often be with their family clinician, who runs initial bloodwork and other tests, but specialist input is an absolute necessity if there are any indications that leukemia is the diagnosis. Specialists will primarily guide the therapy regimen, but nursing will play a pivotal role in assisting in the evaluation, coordinating activities between specialists, and providing patient counseling. A specialized oncology pharmacist is a valuable asset to the team. Their consultation can help guide chemotherapy, appropriate dosing medication reconciliation, and medication counseling for patients, especially regarding adverse events. All interprofessional team members must maintain meticulous records on all interactions and interventions with the patient; this is part of communicating all patient data to the rest of the team. Everyone involved in care must keep other team members informed of any changes in the patient's condition as appropriate and include the patient in all care decisions, answering questions and offering counsel. Patient-centered communication and shared decision-making are integral to successful patient outcomes in the interprofessional team model. [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Video to Play)
(Click Image to Enlarge)
References
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016 May 19:127(20):2391-405. doi: 10.1182/blood-2016-03-643544. Epub 2016 Apr 11 [PubMed PMID: 27069254]
. Erratum: Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2020 Jul:70(4):313. doi: 10.3322/caac.21609. Epub 2020 Apr 6 [PubMed PMID: 32767693]
Vardiman JW. The World Health Organization (WHO) classification of tumors of the hematopoietic and lymphoid tissues: an overview with emphasis on the myeloid neoplasms. Chemico-biological interactions. 2010 Mar 19:184(1-2):16-20. doi: 10.1016/j.cbi.2009.10.009. Epub 2009 Oct 24 [PubMed PMID: 19857474]
Level 3 (low-level) evidenceBrunning RD. Classification of acute leukemias. Seminars in diagnostic pathology. 2003 Aug:20(3):142-53 [PubMed PMID: 14552428]
Yamamoto JF, Goodman MT. Patterns of leukemia incidence in the United States by subtype and demographic characteristics, 1997-2002. Cancer causes & control : CCC. 2008 May:19(4):379-90 [PubMed PMID: 18064533]
Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA: a cancer journal for clinicians. 2017 Jan:67(1):7-30. doi: 10.3322/caac.21387. Epub 2017 Jan 5 [PubMed PMID: 28055103]
Bispo JAB, Pinheiro PS, Kobetz EK. Epidemiology and Etiology of Leukemia and Lymphoma. Cold Spring Harbor perspectives in medicine. 2020 Jun 1:10(6):. doi: 10.1101/cshperspect.a034819. Epub 2020 Jun 1 [PubMed PMID: 31727680]
Level 3 (low-level) evidenceMiranda-Filho A, Piñeros M, Ferlay J, Soerjomataram I, Monnereau A, Bray F. Epidemiological patterns of leukaemia in 184 countries: a population-based study. The Lancet. Haematology. 2018 Jan:5(1):e14-e24. doi: 10.1016/S2352-3026(17)30232-6. Epub [PubMed PMID: 29304322]
Level 2 (mid-level) evidenceSnyder R. Leukemia and benzene. International journal of environmental research and public health. 2012 Aug:9(8):2875-93. doi: 10.3390/ijerph9082875. Epub 2012 Aug 14 [PubMed PMID: 23066403]
Level 3 (low-level) evidenceFriedman DL,Whitton J,Leisenring W,Mertens AC,Hammond S,Stovall M,Donaldson SS,Meadows AT,Robison LL,Neglia JP, Subsequent neoplasms in 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. Journal of the National Cancer Institute. 2010 Jul 21; [PubMed PMID: 20634481]
Level 2 (mid-level) evidenceDavis AS, Viera AJ, Mead MD. Leukemia: an overview for primary care. American family physician. 2014 May 1:89(9):731-8 [PubMed PMID: 24784336]
Level 3 (low-level) evidenceStieglitz E, Loh ML. Genetic predispositions to childhood leukemia. Therapeutic advances in hematology. 2013 Aug:4(4):270-90. doi: 10.1177/2040620713498161. Epub [PubMed PMID: 23926459]
Level 3 (low-level) evidenceLeszczenko P, Borek-Dorosz A, Nowakowska AM, Adamczyk A, Kashyrskaya S, Jakubowska J, Ząbczyńska M, Pastorczak A, Ostrowska K, Baranska M, Marzec KM, Majzner K. Towards Raman-Based Screening of Acute Lymphoblastic Leukemia-Type B (B-ALL) Subtypes. Cancers. 2021 Oct 31:13(21):. doi: 10.3390/cancers13215483. Epub 2021 Oct 31 [PubMed PMID: 34771646]
Looi W,Zargari A,Dun K,Grigoriadis G,Fedele P,Gregory GP,Low MSY, Concomitant diagnosis of chronic myeloid leukaemia and myeloma. Pathology. 2021 Nov 11; [PubMed PMID: 34776244]
Nebgen DR, Rhodes HE, Hartman C, Munsell MF, Lu KH. Abnormal Uterine Bleeding as the Presenting Symptom of Hematologic Cancer. Obstetrics and gynecology. 2016 Aug:128(2):357-363. doi: 10.1097/AOG.0000000000001529. Epub [PubMed PMID: 27400009]
Sanz MA, Grimwade D, Tallman MS, Lowenberg B, Fenaux P, Estey EH, Naoe T, Lengfelder E, Büchner T, Döhner H, Burnett AK, Lo-Coco F. Management of acute promyelocytic leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood. 2009 Feb 26:113(9):1875-91. doi: 10.1182/blood-2008-04-150250. Epub 2008 Sep 23 [PubMed PMID: 18812465]
Mantha S, Goldman DA, Devlin SM, Lee JW, Zannino D, Collins M, Douer D, Iland HJ, Litzow MR, Stein EM, Appelbaum FR, Larson RA, Stone R, Powell BL, Geyer S, Laumann K, Rowe JM, Erba H, Coutre S, Othus M, Park JH, Wiernik PH, Tallman MS. Determinants of fatal bleeding during induction therapy for acute promyelocytic leukemia in the ATRA era. Blood. 2017 Mar 30:129(13):1763-1767. doi: 10.1182/blood-2016-10-747170. Epub 2017 Jan 12 [PubMed PMID: 28082441]
Montesinos P, Bergua JM, Vellenga E, Rayón C, Parody R, de la Serna J, León A, Esteve J, Milone G, Debén G, Rivas C, González M, Tormo M, Díaz-Mediavilla J, González JD, Negri S, Amutio E, Brunet S, Lowenberg B, Sanz MA. Differentiation syndrome in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline chemotherapy: characteristics, outcome, and prognostic factors. Blood. 2009 Jan 22:113(4):775-83. doi: 10.1182/blood-2008-07-168617. Epub 2008 Oct 22 [PubMed PMID: 18945964]
Lallemand-Breitenbach V, de Thé H. Retinoic acid plus arsenic trioxide, the ultimate panacea for acute promyelocytic leukemia? Blood. 2013 Sep 19:122(12):2008-10. doi: 10.1182/blood-2013-06-505115. Epub 2013 Jul 26 [PubMed PMID: 23894153]
Iland HJ, Bradstock K, Supple SG, Catalano A, Collins M, Hertzberg M, Browett P, Grigg A, Firkin F, Hugman A, Reynolds J, Di Iulio J, Tiley C, Taylor K, Filshie R, Seldon M, Taper J, Szer J, Moore J, Bashford J, Seymour JF, Australasian Leukaemia and Lymphoma Group. All-trans-retinoic acid, idarubicin, and IV arsenic trioxide as initial therapy in acute promyelocytic leukemia (APML4). Blood. 2012 Aug 23:120(8):1570-80; quiz 1752 [PubMed PMID: 22715121]
Abaza Y,Kantarjian H,Garcia-Manero G,Estey E,Borthakur G,Jabbour E,Faderl S,O'Brien S,Wierda W,Pierce S,Brandt M,McCue D,Luthra R,Patel K,Kornblau S,Kadia T,Daver N,DiNardo C,Jain N,Verstovsek S,Ferrajoli A,Andreeff M,Konopleva M,Estrov Z,Foudray M,McCue D,Cortes J,Ravandi F, Long-term outcome of acute promyelocytic leukemia treated with all-{i}trans{/i}-retinoic acid, arsenic trioxide, and gemtuzumab. Blood. 2017 Mar 9 [PubMed PMID: 28003274]
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, Levine RL, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz M, Sierra J, Tallman MS, Tien HF, Wei AH, Löwenberg B, Bloomfield CD. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017 Jan 26:129(4):424-447. doi: 10.1182/blood-2016-08-733196. Epub 2016 Nov 28 [PubMed PMID: 27895058]
Hills RK, Castaigne S, Appelbaum FR, Delaunay J, Petersdorf S, Othus M, Estey EH, Dombret H, Chevret S, Ifrah N, Cahn JY, Récher C, Chilton L, Moorman AV, Burnett AK. Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: a meta-analysis of individual patient data from randomised controlled trials. The Lancet. Oncology. 2014 Aug:15(9):986-96. doi: 10.1016/S1470-2045(14)70281-5. Epub 2014 Jul 6 [PubMed PMID: 25008258]
Level 1 (high-level) evidenceSchlenk RF, Weber D, Fiedler W, Salih HR, Wulf G, Salwender H, Schroeder T, Kindler T, Lübbert M, Wolf D, Westermann J, Kraemer D, Götze KS, Horst HA, Krauter J, Girschikofsky M, Ringhoffer M, Südhoff T, Held G, Derigs HG, Schroers R, Greil R, Grießhammer M, Lange E, Burchardt A, Martens U, Hertenstein B, Marretta L, Heuser M, Thol F, Gaidzik VI, Herr W, Krzykalla J, Benner A, Döhner K, Ganser A, Paschka P, Döhner H, German-Austrian AML Study Group. Midostaurin added to chemotherapy and continued single-agent maintenance therapy in acute myeloid leukemia with FLT3-ITD. Blood. 2019 Feb 21:133(8):840-851. doi: 10.1182/blood-2018-08-869453. Epub 2018 Dec 18 [PubMed PMID: 30563875]
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, Konopleva M, Döhner H, Letai A, Fenaux P, Koller E, Havelange V, Leber B, Esteve J, Wang J, Pejsa V, Hájek R, Porkka K, Illés Á, Lavie D, Lemoli RM, Yamamoto K, Yoon SS, Jang JH, Yeh SP, Turgut M, Hong WJ, Zhou Y, Potluri J, Pratz KW. Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. The New England journal of medicine. 2020 Aug 13:383(7):617-629. doi: 10.1056/NEJMoa2012971. Epub [PubMed PMID: 32786187]
Kolitz JE, Strickland SA, Cortes JE, Hogge D, Lancet JE, Goldberg SL, Villa KF, Ryan RJ, Chiarella M, Louie AC, Ritchie EK, Stuart RK. Consolidation outcomes in CPX-351 versus cytarabine/daunorubicin-treated older patients with high-risk/secondary acute myeloid leukemia. Leukemia & lymphoma. 2020 Mar:61(3):631-640. doi: 10.1080/10428194.2019.1688320. Epub 2019 Nov 25 [PubMed PMID: 31760835]
Slayton WB, Schultz KR, Kairalla JA, Devidas M, Mi X, Pulsipher MA, Chang BH, Mullighan C, Iacobucci I, Silverman LB, Borowitz MJ, Carroll AJ, Heerema NA, Gastier-Foster JM, Wood BL, Mizrahy SL, Merchant T, Brown VI, Sieger L, Siegel MJ, Raetz EA, Winick NJ, Loh ML, Carroll WL, Hunger SP. Dasatinib Plus Intensive Chemotherapy in Children, Adolescents, and Young Adults With Philadelphia Chromosome-Positive Acute Lymphoblastic Leukemia: Results of Children's Oncology Group Trial AALL0622. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2018 Aug 1:36(22):2306-2314. doi: 10.1200/JCO.2017.76.7228. Epub 2018 May 29 [PubMed PMID: 29812996]
Jabbour E, Short NJ, Ravandi F, Huang X, Daver N, DiNardo CD, Konopleva M, Pemmaraju N, Wierda W, Garcia-Manero G, Sasaki K, Cortes J, Garris R, Khoury JD, Jorgensen J, Jain N, Alvarez J, O'Brien S, Kantarjian H. Combination of hyper-CVAD with ponatinib as first-line therapy for patients with Philadelphia chromosome-positive acute lymphoblastic leukaemia: long-term follow-up of a single-centre, phase 2 study. The Lancet. Haematology. 2018 Dec:5(12):e618-e627. doi: 10.1016/S2352-3026(18)30176-5. Epub [PubMed PMID: 30501869]
Foà R, Bassan R, Vitale A, Elia L, Piciocchi A, Puzzolo MC, Canichella M, Viero P, Ferrara F, Lunghi M, Fabbiano F, Bonifacio M, Fracchiolla N, Di Bartolomeo P, Mancino A, De Propris MS, Vignetti M, Guarini A, Rambaldi A, Chiaretti S, GIMEMA Investigators. Dasatinib-Blinatumomab for Ph-Positive Acute Lymphoblastic Leukemia in Adults. The New England journal of medicine. 2020 Oct 22:383(17):1613-1623. doi: 10.1056/NEJMoa2016272. Epub [PubMed PMID: 33085860]
Rousselot P, Coudé MM, Gokbuget N, Gambacorti Passerini C, Hayette S, Cayuela JM, Huguet F, Leguay T, Chevallier P, Salanoubat C, Bonmati C, Alexis M, Hunault M, Glaisner S, Agape P, Berthou C, Jourdan E, Fernandes J, Sutton L, Banos A, Reman O, Lioure B, Thomas X, Ifrah N, Lafage-Pochitaloff M, Bornand A, Morisset L, Robin V, Pfeifer H, Delannoy A, Ribera J, Bassan R, Delord M, Hoelzer D, Dombret H, Ottmann OG, European Working Group on Adult ALL (EWALL) group. Dasatinib and low-intensity chemotherapy in elderly patients with Philadelphia chromosome-positive ALL. Blood. 2016 Aug 11:128(6):774-82. doi: 10.1182/blood-2016-02-700153. Epub 2016 Apr 27 [PubMed PMID: 27121472]
Stock W, Luger SM, Advani AS, Yin J, Harvey RC, Mullighan CG, Willman CL, Fulton N, Laumann KM, Malnassy G, Paietta E, Parker E, Geyer S, Mrózek K, Bloomfield CD, Sanford B, Marcucci G, Liedtke M, Claxton DF, Foster MC, Bogart JA, Grecula JC, Appelbaum FR, Erba H, Litzow MR, Tallman MS, Stone RM, Larson RA. A pediatric regimen for older adolescents and young adults with acute lymphoblastic leukemia: results of CALGB 10403. Blood. 2019 Apr 4:133(14):1548-1559. doi: 10.1182/blood-2018-10-881961. Epub 2019 Jan 18 [PubMed PMID: 30658992]
Dunsmore KP, Winter SS, Devidas M, Wood BL, Esiashvili N, Chen Z, Eisenberg N, Briegel N, Hayashi RJ, Gastier-Foster JM, Carroll AJ, Heerema NA, Asselin BL, Rabin KR, Zweidler-Mckay PA, Raetz EA, Loh ML, Schultz KR, Winick NJ, Carroll WL, Hunger SP. Children's Oncology Group AALL0434: A Phase III Randomized Clinical Trial Testing Nelarabine in Newly Diagnosed T-Cell Acute Lymphoblastic Leukemia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2020 Oct 1:38(28):3282-3293. doi: 10.1200/JCO.20.00256. Epub 2020 Aug 19 [PubMed PMID: 32813610]
Level 1 (high-level) evidenceDeAngelo DJ, Stevenson KE, Dahlberg SE, Silverman LB, Couban S, Supko JG, Amrein PC, Ballen KK, Seftel MD, Turner AR, Leber B, Howson-Jan K, Kelly K, Cohen S, Matthews JH, Savoie L, Wadleigh M, Sirulnik LA, Galinsky I, Neuberg DS, Sallan SE, Stone RM. Long-term outcome of a pediatric-inspired regimen used for adults aged 18-50 years with newly diagnosed acute lymphoblastic leukemia. Leukemia. 2015 Mar:29(3):526-34. doi: 10.1038/leu.2014.229. Epub 2014 Jul 31 [PubMed PMID: 25079173]
Levato L, Molica S. Rituximab in the management of acute lymphoblastic leukemia. Expert opinion on biological therapy. 2018 Feb:18(2):221-226. doi: 10.1080/14712598.2018.1425389. Epub 2018 Jan 17 [PubMed PMID: 29310477]
Level 3 (low-level) evidenceBerry DH, Pullen J, George S, Vietti TJ, Sullivan MP, Fernbach D. Comparison of prednisolone, vincristine, methotrexate, and 6-mercaptopurine vs. vincristine and prednisone induction therapy in childhood acute leukemia. Cancer. 1975 Jul:36(1):98-102 [PubMed PMID: 1203854]
Level 1 (high-level) evidenceSokal JE, Cox EB, Baccarani M, Tura S, Gomez GA, Robertson JE, Tso CY, Braun TJ, Clarkson BD, Cervantes F. Prognostic discrimination in "good-risk" chronic granulocytic leukemia. Blood. 1984 Apr:63(4):789-99 [PubMed PMID: 6584184]
Hasford J, Baccarani M, Hoffmann V, Guilhot J, Saussele S, Rosti G, Guilhot F, Porkka K, Ossenkoppele G, Lindoerfer D, Simonsson B, Pfirrmann M, Hehlmann R. Predicting complete cytogenetic response and subsequent progression-free survival in 2060 patients with CML on imatinib treatment: the EUTOS score. Blood. 2011 Jul 21:118(3):686-92. doi: 10.1182/blood-2010-12-319038. Epub 2011 May 2 [PubMed PMID: 21536864]
Pfirrmann M, Baccarani M, Saussele S, Guilhot J, Cervantes F, Ossenkoppele G, Hoffmann VS, Castagnetti F, Hasford J, Hehlmann R, Simonsson B. Prognosis of long-term survival considering disease-specific death in patients with chronic myeloid leukemia. Leukemia. 2016 Jan:30(1):48-56. doi: 10.1038/leu.2015.261. Epub 2015 Sep 29 [PubMed PMID: 26416462]
Yun S, Vincelette ND, Segar JM, Dong Y, Shen Y, Kim DW, Abraham I. Comparative Effectiveness of Newer Tyrosine Kinase Inhibitors Versus Imatinib in the First-Line Treatment of Chronic-Phase Chronic Myeloid Leukemia Across Risk Groups: A Systematic Review and Meta-Analysis of Eight Randomized Trials. Clinical lymphoma, myeloma & leukemia. 2016 Jun:16(6):e85-94. doi: 10.1016/j.clml.2016.03.003. Epub 2016 Mar 30 [PubMed PMID: 27101984]
Level 2 (mid-level) evidenceCortes JE, Kim DW, Pinilla-Ibarz J, le Coutre PD, Paquette R, Chuah C, Nicolini FE, Apperley JF, Khoury HJ, Talpaz M, DeAngelo DJ, Abruzzese E, Rea D, Baccarani M, Müller MC, Gambacorti-Passerini C, Lustgarten S, Rivera VM, Haluska FG, Guilhot F, Deininger MW, Hochhaus A, Hughes TP, Shah NP, Kantarjian HM. Ponatinib efficacy and safety in Philadelphia chromosome-positive leukemia: final 5-year results of the phase 2 PACE trial. Blood. 2018 Jul 26:132(4):393-404. doi: 10.1182/blood-2016-09-739086. Epub 2018 Mar 22 [PubMed PMID: 29567798]
Réa D, Mauro MJ, Boquimpani C, Minami Y, Lomaia E, Voloshin S, Turkina A, Kim DW, Apperley JF, Abdo A, Fogliatto LM, Kim DDH, le Coutre P, Saussele S, Annunziata M, Hughes TP, Chaudhri N, Sasaki K, Chee L, García-Gutiérrez V, Cortes JE, Aimone P, Allepuz A, Quenet S, Bédoucha V, Hochhaus A. A phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Blood. 2021 Nov 25:138(21):2031-2041. doi: 10.1182/blood.2020009984. Epub [PubMed PMID: 34407542]
Level 1 (high-level) evidenceCostello J, Kang M, Banerji V. Frontline Treatment of the Young, Fit Patient with CLL: A Canadian Perspective. Current oncology (Toronto, Ont.). 2021 Sep 30:28(5):3825-3835. doi: 10.3390/curroncol28050326. Epub 2021 Sep 30 [PubMed PMID: 34677244]
Level 3 (low-level) evidenceEichhorst B, Fink AM, Bahlo J, Busch R, Kovacs G, Maurer C, Lange E, Köppler H, Kiehl M, Sökler M, Schlag R, Vehling-Kaiser U, Köchling G, Plöger C, Gregor M, Plesner T, Trneny M, Fischer K, Döhner H, Kneba M, Wendtner CM, Klapper W, Kreuzer KA, Stilgenbauer S, Böttcher S, Hallek M, international group of investigators, German CLL Study Group (GCLLSG). First-line chemoimmunotherapy with bendamustine and rituximab versus fludarabine, cyclophosphamide, and rituximab in patients with advanced chronic lymphocytic leukaemia (CLL10): an international, open-label, randomised, phase 3, non-inferiority trial. The Lancet. Oncology. 2016 Jul:17(7):928-942. doi: 10.1016/S1470-2045(16)30051-1. Epub 2016 May 20 [PubMed PMID: 27216274]
Level 1 (high-level) evidenceSharman JP, Egyed M, Jurczak W, Skarbnik A, Pagel JM, Flinn IW, Kamdar M, Munir T, Walewska R, Corbett G, Fogliatto LM, Herishanu Y, Banerji V, Coutre S, Follows G, Walker P, Karlsson K, Ghia P, Janssens A, Cymbalista F, Woyach JA, Salles G, Wierda WG, Izumi R, Munugalavadla V, Patel P, Wang MH, Wong S, Byrd JC. Acalabrutinib with or without obinutuzumab versus chlorambucil and obinutuzmab for treatment-naive chronic lymphocytic leukaemia (ELEVATE TN): a randomised, controlled, phase 3 trial. Lancet (London, England). 2020 Apr 18:395(10232):1278-1291. doi: 10.1016/S0140-6736(20)30262-2. Epub [PubMed PMID: 32305093]
Level 1 (high-level) evidenceAl-Sawaf O, Zhang C, Tandon M, Sinha A, Fink AM, Robrecht S, Samoylova O, Liberati AM, Pinilla-Ibarz J, Opat S, Sivcheva L, Le Dû K, Fogliatto LM, Niemann CU, Weinkove R, Robinson S, Kipps TJ, Tausch E, Schary W, Ritgen M, Wendtner CM, Kreuzer KA, Eichhorst B, Stilgenbauer S, Hallek M, Fischer K. Venetoclax plus obinutuzumab versus chlorambucil plus obinutuzumab for previously untreated chronic lymphocytic leukaemia (CLL14): follow-up results from a multicentre, open-label, randomised, phase 3 trial. The Lancet. Oncology. 2020 Sep:21(9):1188-1200. doi: 10.1016/S1470-2045(20)30443-5. Epub [PubMed PMID: 32888452]
Level 1 (high-level) evidenceMoreno C, Greil R, Demirkan F, Tedeschi A, Anz B, Larratt L, Simkovic M, Samoilova O, Novak J, Ben-Yehuda D, Strugov V, Gill D, Gribben JG, Hsu E, Lih CJ, Zhou C, Clow F, James DF, Styles L, Flinn IW. Ibrutinib plus obinutuzumab versus chlorambucil plus obinutuzumab in first-line treatment of chronic lymphocytic leukaemia (iLLUMINATE): a multicentre, randomised, open-label, phase 3 trial. The Lancet. Oncology. 2019 Jan:20(1):43-56. doi: 10.1016/S1470-2045(18)30788-5. Epub 2018 Dec 3 [PubMed PMID: 30522969]
Level 1 (high-level) evidenceCheung MC, Mittmann N, Owen C, Abdel-Samad N, Fraser GAM, Lam S, Crump M, Sperlich C, van der Jagt R, Prica A, Couban S, Woyach JA, Ruppert AS, Booth AM, Mandrekar SJ, McDonald G, Shepherd LE, Yen H, Chen BE, Hay AE. A Prospective Economic Analysis of Early Outcome Data From the Alliance A041202/ CCTG CLC.2 Randomized Phase III Trial Of Bendamustine-Rituximab Compared With Ibrutinib-Based Regimens in Untreated Older Patients With Chronic Lymphocytic Leukemia. Clinical lymphoma, myeloma & leukemia. 2021 Nov:21(11):766-774. doi: 10.1016/j.clml.2021.06.011. Epub 2021 Jul 3 [PubMed PMID: 34334330]
Level 1 (high-level) evidenceHoward SC, Trifilio S, Gregory TK, Baxter N, McBride A. Tumor lysis syndrome in the era of novel and targeted agents in patients with hematologic malignancies: a systematic review. Annals of hematology. 2016 Mar:95(4):563-73. doi: 10.1007/s00277-015-2585-7. Epub 2016 Jan 12 [PubMed PMID: 26758269]
Level 1 (high-level) evidenceFreifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR, Infectious Diseases Society of Americaa. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 Update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2011 Feb 15:52(4):427-31. doi: 10.1093/cid/ciq147. Epub 2011 Jan 4 [PubMed PMID: 21205990]
Level 1 (high-level) evidence