Introduction
Retinal hemorrhages are an important ophthalmic diagnostic sign for an underlying systemic vascular disorder. They range from the smallest dot and blot hemorrhage to massive sub-hyaloid hemorrhage. The location, size, and distribution of the hemorrhages provide clues to the etiology and uncover underlying systemic disorders such as vascular disease, hematologic disorders, and dyscrasias, infections, trauma, or hypoxia. Rarely it can also be seen idiopathically. Most require a detailed systemic work up to detect the underlying cause for the hemorrhages. Management consists of observation, treating the primary cause, and intraocular management to reduce the ischemic and neovascularization sequelae following the hemorrhages.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Following are the conditions which show retinal hemorrhages depending on the stage and severity of the disease:
- Ocular diseases: Age-related macular degeneration (ARMD), polypoidal choroidal vasculopathy (PCV), juxta foveal telangiectasia, optic disc hemorrhages.
- Diabetic retinopathy: dot and blot and vitreous hemorrhages. Bilateral and diffusely distributed in the posterior pole.
- Hypertensive retinopathy: diffuse flame-shaped hemorrhages, preretinal hemorrhages seen rarely. Bilateral and diffusely distributed in the posterior pole.
- Retinal vein occlusions: diffuse intraretinal hemorrhages in all quadrants in central retinal vein occlusions and sectoral distribution in branch retinal vein occlusions.
- Trauma: multilayered hemorrhages can be unilateral or bilateral, depending on the type of trauma. Preretinal hemorrhages are typical of Terson syndrome and Valsalva retinopathy. The shaken baby syndrome shows bilateral diffuse multilayered hemorrhages in infants and children. Birth trauma is the leading cause of neonatal retinal hemorrhages.
- Anemia: Roth spots, multilayered hemorrhages, subhyaloid hemorrhages, and vitreous hemorrhages. They are seen bilaterally and diffusely distributed.
- Leukemia: Preretinal hemorrhages, vitreous hemorrhages, flame-shaped hemorrhages, intraretinal hemorrhages, Roth spots, and cotton wool spots, and. Sea-fan neovascularization is a typical finding. Bilaterally seen and diffusely distributed.
- Acute bacterial endocarditis: preretinal/vitreous, intraretinal, or flame-shaped hemorrhages in the parapapillary rim, cotton wool spots, Roth spots. They are bilaterally seen.
- Sickle cell anemia: SC and S-Thal variants lead to retinopathy, intraretinal salmon patch hemorrhages, black sunburst chorioretinal ischemic scars, and sea-fan neovascularization which might lead to vitreous hemorrhage. They are seen bilaterally.
- Ocular ischemic syndrome: Mid-peripheral intraretinal hemorrhages, retinal neovascularization.
- Preeclampsia: Intraretinal hemorrhages, Elschnig spots, with serous retinal detachment. They are seen bilaterally with varying intensity.
- Connective tissue disorders (lupus): intraretinal hemorrhage and vascular occlusions (severe stages) seen bilaterally.
- High altitude retinopathy: Roth spots, multilayered hemorrhages, and vitreous hemorrhages often seen bilaterally.
Epidemiology
Retinal hemorrhages in critically ill children with no history of trauma or abuse have a prevalence of 15%. Most cases are mild and are seen in children younger than two years and are associated with systemic infection, accidental brain trauma, and severe coagulopathy.[1] Birth-related retinal hemorrhages are seen in 25% of newborns with normal delivery and 40% to 50% of newborns with instrumental deliveries.[2] Retinal hemorrhages were seen in 30% of physically abused children, and most are less than six months of age.[3][4] The prevalence of retinal hemorrhages in adults is most commonly seen after 40 years of age, as most systemic disorders are common in that age.
Pathophysiology
Retinal hemorrhages are classified according to the location in the retina: Retinal nerve fiber layer (RNFL), intraretinal, subretinal, subretinal pigment epithelium (RPE), subhyaloid/preretinal, and vitreous hemorrhage.[5]
Retinal Nerve Fiber Layer (RNFL) Hemorrhages
RNFL hemorrhages are superficial and follow the direction, shape, and spread of the RNFL bundles. Three types of hemorrhages are seen at the level of RNFL: flame-shaped hemorrhages, splinter (disc) hemorrhages, and Roth spots.
- Flame shaped hemorrhages: These hemorrhages are diffuse, found in the posterior pole, and last approximately 6 to 12 weeks. They occur typically in diseases affecting superficial retinal capillary plexus secondary to arterial diseases like hypertension, blood dyscrasias, and anemias.
- Disc (Drance) hemorrhages: Theses are superficial splinter shaped hemorrhages located near the optic disc margin at the prelaminar level within one-disc diameter, usually with a tapered end towards the disc and feathery end away from the disc.[6][7] These are oriented perpendicular to the discs margin, found most commonly in inferotemporal in location, and are oriented along the retinal nerve fiber defect starting at the optic disc rim notch. Conditions causing disc hemorrhage are normal-tension glaucoma, primary open-angle glaucoma, posterior vitreous detachment, optic neuropathy, diabetes, anemia, hypertension, and retinal vascular disease.
- Roth spots: Roth spots are round in shape with a white center. It was Litten who described the association (Litten sign) and referred to it as Roth spots.[8][9][10] Capillary rupture with extravasation, and central fibrin–platelet plug gives the white center to the Roth spot. Roth spots are characteristic of subacute bacterial endocarditis and also seen in leukemia, anemia, anoxia, and other rare conditions.
Intraretinal Hemorrhages
These dot and blot hemorrhages are found within the inner nuclear and outer plexiform layers of the retina. These are dense, dark red, sharply outlined, and are seen in disorders that affect the pre-venular deep capillary layer. Common causes for such hemorrhages include diabetic retinopathy, retinal vein occlusions, ocular ischemic syndrome, sickle cell retinopathy, and juxta foveal telangiectasia.[5] Purtsher retinopathy is an occlusive microvasculopathy associated with cranial or thoracic compressive trauma.[11] Retinal findings are intraretinal whitening, cotton wool spots, and intraretinal hemorrhages. Purtscher-like retinopathy is seen in acute pancreatitis, renal failure, and autoimmune disease.
Subretinal Hemorrhages
These hemorrhages occur between the photoreceptor layer and retinal pigment epithelium (RPE). The hemorrhages are deep red in color and broader in shape with diffuse margins. Such hemorrhages are commonly seen in ARMD, presumed ocular histoplasmosis, high myopia, PCV, retinal macroaneurysm, and trauma. Sub-macular hemorrhages are commonly seen in choroidal neovascular membranes secondary to ARMD.[12]
Sub-RPE Hemorrhages
These hemorrhages are located between RPE and Bruch membrane and appear dark red with well-defined sharp borders. They are commonly seen in choroidal neovascular membranes (CNVM), choroidal tumors, and choroidal rupture secondary to acute trauma.
Sub-hyaloid or Preretinal Hemorrhages
Preretinal hemorrhages are “boat” or ‘D’ shaped hemorrhages which collect between the posterior limiting membrane of the vitreous and internal limiting membrane (ILM) of the retina.[13] Causes include Terson syndrome, Valsalva retinopathy, proliferative diabetic retinopathy, and proliferative retinopathy after retinal vein occlusions. Terson syndrome is intraocular hemorrhage associated with subarachnoid hemorrhage, intracerebral hemorrhage, or traumatic brain injury.[14] Hemorrhage may be present in the vitreous, subhyaloid, or intraretinal /sub-internal limiting membrane. Valsalva retinopathy is a pre-retinal hemorrhage caused by a sudden increase in intra-thoracic or intra-abdominal pressure.[15][4]
Vitreous Hemorrhage (VH)
Bleeding into the vitreous cavity is seen as fresh blood clots with sudden onset of floaters.[16] Chronic hemorrhages appear as diffuse vitreous clouding with settled blood inferiorly. They are commonly seen due to the rupture of a vessel, as seen commonly in proliferative diabetic retinopathy, retinal arteriolar microaneurysm, or during posterior vitreous detachment. A subretinal hemorrhage can cause a breakthrough bleeding into the vitreous. Breakthrough hemorrhage into vitreous also happens in malignant choroidal melanoma, retinal vascular occlusions, and idiopathic polypoidal choroidal vasculopathy (IPCV).
Shaken Baby Syndrome
This comes under abusive head trauma (AHT), is seen in young children caused by repeated acceleration-deceleration injury.[17] Characteristic clinical features include extensive bilateral multilayered retinal hemorrhages, intracranial injury (hemorrhage/hypoxic-ischemic injury), and occult fractures (ribs and long bone metaphysis).
History and Physical
A detailed history about social conditions, medication use, abuse or trauma, recent Valsalva maneuvers or chest compression injury, flashes or floaters with a sudden transient dimming of vision, are all important to come to a diagnosis. All patients need a slit lamp examination of the anterior segment, dilated fundus examination, and intraocular pressure measurement. Optical coherence tomography (OCT), fundus fluorescein angiography (FFA), and fundus photography are all helpful to determine the location and depth of the hemorrhage. One should suspect abusive head trauma if a child less than three years shows retinal hemorrhages with an intracranial injury.[18]
Evaluation
Blood pressure, body mass index, and blood sugar are mandatory before evaluating further. Also, the following workup would help in diagnosing the underlying systemic disorder leading to the retinal hemorrhages:
- Diabetes and metabolic syndromes: complete blood count and platelet count, erythrocyte sedimentation rate and C-reactive protein, fasting glucose and hemoglobin A1c and lipid profile.
- Hypercoagulable states: prothrombin time/ partial thromboplastin time, protein-C and -S, factor V Leiden, prothrombin gene mutation, homocysteine, antithrombin III, antiphospholipid antibodies.
- Systemic lupus erythematosus (SLE) and autoimmune workup: antinuclear antibody, anti-ds deoxyribonucleic acid (DNA), anti-nRNP antibody testing, anti-histone antibodies, anti-Ro/SS-A, anti-La/SS-B antibodies.
- Infective work up: ELISA, FTA-ABS/RPR.
- Masquerade syndrome: When the diagnosis is unclear, doing Lyme titers, herpes simplex titers, and FTA-ABS/RPR for syphilis will help in the diagnosis.
- Spondyloarthropathy: HLA-B5/B12: For conditions that present with anterior and posterior segment findings, one should rule out Behcet disease.
Treatment / Management
A solitary retinal hemorrhage can be observed and followed up for progression in size and number. Hemorrhages that do not obscure or threaten vision do not warrant immediate treatment, and the primary systemic disorder causing the hemorrhages needs to be diagnosed and addressed. Direct intervention for retinal hemorrhages is indicated in submacular, subhyaloid, and vitreous hemorrhages because of their potential to damage vision irreversibly.
Most dot and blot, splinter, and flame-shaped hemorrhages are not vision-threatening and are usually found in the posterior pole sparing the fovea and can be observed. Hemorrhages seen in retinal vein occlusions are not treated per se, but the retinal edema or the neovascularization, which follows as a sequela, needs to be treated. Roth spots are generally asymptomatic and typically resolve with treatment of the underlying disease, especially subacute bacterial endocarditis.
Subhyaloid hemorrhage is seen typically in Terson syndrome and Valsalva retinopathy.[15][14][4] Besides, bilateral hemorrhages in the vitreous, sub-hyaloid, or intra-retinal hemorrhages are also seen. The first approach for a subhyaloid hemorrhage is always conservative observation. If no signs of resolution are seen within 1 to 3 months or for patients with high professional visual demand, Nd: YAG laser membranotomy is done to rupture the posterior hyaloid or the internal limiting membrane to drain the blood into vitreous. The blood settles into the inferior vitreous and out of the visual axis, prompting a rapid return of central visual acuity. Unresolved vitreous hemorrhage obstructing vision needs pars plana vitrectomy (PPV).(B3)
Submacular hemorrhage (SMH) is a sight-threatening complication that can occur in a CNVM secondary to exudative ARMD, PCV, high myopia, angioid streaks, and others. CNVM appears as a dirty grey-green color lesion, deep to the retina.[19] The grey-green appearance is believed to be due to the hyperplastic response of RPE. It may be accompanied by subretinal hemorrhage and/or lipid, serous or hemorrhagic PED, neurosensory exudate detachment, macular edema, and cystoid macular changes. Signs of choroidal neovascularization include RPE elevation, exudate, or subretinal fluid.
Patients prone to develop CNVM are advised to self-check their retinal status weekly through Amsler grid charts. Any sudden onset of distortion of lines is suspicious of the development of CNVM. When left untreated, SMH causes irreversible vision loss by damaging the photoreceptors. The treatment strategies for SMH include:
- Pneumatic displacement of SMH with or without tissue plasminogen activator (t-PA) displacement of blood from the fovea, usually by intravitreal injection of 0.3 to 0.4 ml of either shorter-acting sulfur hexafluoride (SF6) or longer-acting perfluoropropane (C3F8) followed by face-down head positioning for one to three days.
- Pharmacologic clot lysis such as with recombinant tissue plasminogen activator (r-tPA)
- Intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) agents
- Pars plana vitrectomy with subretinal tPA/pneumatic gas displacement with and without post-operative anti-VEGF injections
Vitreous hemorrhage is commonly seen in vascular conditions such as diabetic retinopathy and retinal vein occlusions. The treatment strategies depending on the severity of hemorrhage and vision loss are as follows:[16][20]
- Bed rest with head elevation helps reduce further bleeding. Bilateral eye patching helps in reducing eye movement, thereby settling the bleeding inferiorly, helping in a faster visual recovery.
- Avoid drugs like aspirin under physician supervision.
- Retinal breaks are closed by laser photocoagulation or cryotherapy (unlike cryotherapy, laser photocoagulation can close the compromised vessel in addition to the retinal tear), detached retinas are reattached with surgery, and proliferative retinal vascular diseases are treated with laser photocoagulation or cryotherapy.
- Surgical removal by Pars-Plana vitrectomy is indicated in patients with retinal detachment, unresolved VH for more than 2 to 3 months, VH with rubeosis, or Ghost cell glaucoma. Ghost cell glaucoma is a complication of long-standing vitreous hemorrhage wherein the hemoglobin-laden macrophages block the trabecular meshwork to cause raised intraocular pressure. Khaki-colored or red-tinged cells are seen floating in the anterior chamber, and reddish-brown discoloration of the trabecular meshwork is often present. The cells develop within 1 to 3 months of vitreous hemorrhage.
Differential Diagnosis
Since retinal hemorrhages can be found in both children and adults, therefore the differentials also vary according to the age group.
Neonatal: hemorrhages from birth trauma, including spontaneous vaginal delivery, vacuum extraction, and double instrument deliveries (vacuum and forceps).[2]
Infants and Children:
- Ocular: Child abuse, Coat disease, persistent hyperplastic persistent vitreous, retinopathy of prematurity, retinal dysplasia, hypertension, myopia,
- Systemic: Hematological or cardiovascular disorder, infection, protein C deficiency.[21]
Adults:
Diabetes, hypertension, leukemia, blood dyscrasias, hypoxia/ anoxia/high altitudinal syndromes, high myopia, posterior vitreous detachment, retinal tear, and detachment.
Roth spots:
- Subacute bacterial endocarditis
- Leukemia
- Anemia
- Anoxia
- Carbon monoxide poisoning
- Prolonged intubation during anesthesia
- Preeclampsia
- Hypertension
- Diabetic retinopathy
- HIV retinopathy
- Complicated labor and traumatic delivery in mothers and neonates
- Shaken baby syndrome
- Intracranial hemorrhage from arteriovenous malformation or aneurysm
- Acute reduction of intraocular pressure following trabeculectomy
Prognosis
Most neonatal and infant retinal hemorrhages secondary to trauma have a good prognosis and resolve in 2 to 4 weeks. Retinal hemorrhages secondary to metabolic syndromes and venous occlusions resolve with control of the underlying conditions. Submacular and subretinal hemorrhages have a very poor prognosis and can irreversibly affect the vision due to damage to the photoreceptor layer. Subhyaloid hemorrhages, if ruptured by ND-YAG laser at an appropriate time, have a good prognosis. Most vitreous hemorrhages resolve within three months, and fine traces of blood clot can still be seen settled inferiorly. Unresolved hemorrhages or hemorrhages which cause secondary glaucoma carry a poor prognosis.
Complications
Following are the complications that can arise secondary to retinal hemorrhages and underlying disorders:
- Photoreceptor damage leading to permanent vision loss
- Neovascular and Ghost cell glaucoma
- Organized vitreous hemorrhage
- Submacular fibrosis
- Retinal neovascularization
- Vitreoretinal fibrovascular proliferation
Deterrence and Patient Education
- Educate the patients about their retinal hemorrhages and the importance of keeping their underlying comorbid systemic conditions under control.
- Provide them with education leaflets and handover materials.
- Explain to them about multidisciplinary liaison and how all the comorbidities are interlinked and how they influence one another.
- Inform the patients about the risk their retinal hemorrhages have over their vision and define the risks of progression and its consequences.
Enhancing Healthcare Team Outcomes
- Discuss a follow-up or referral appointment to the clinic.
- Schedule the patient to return to the clinic if any new ocular symptoms or changes in vision occur between the appointments.
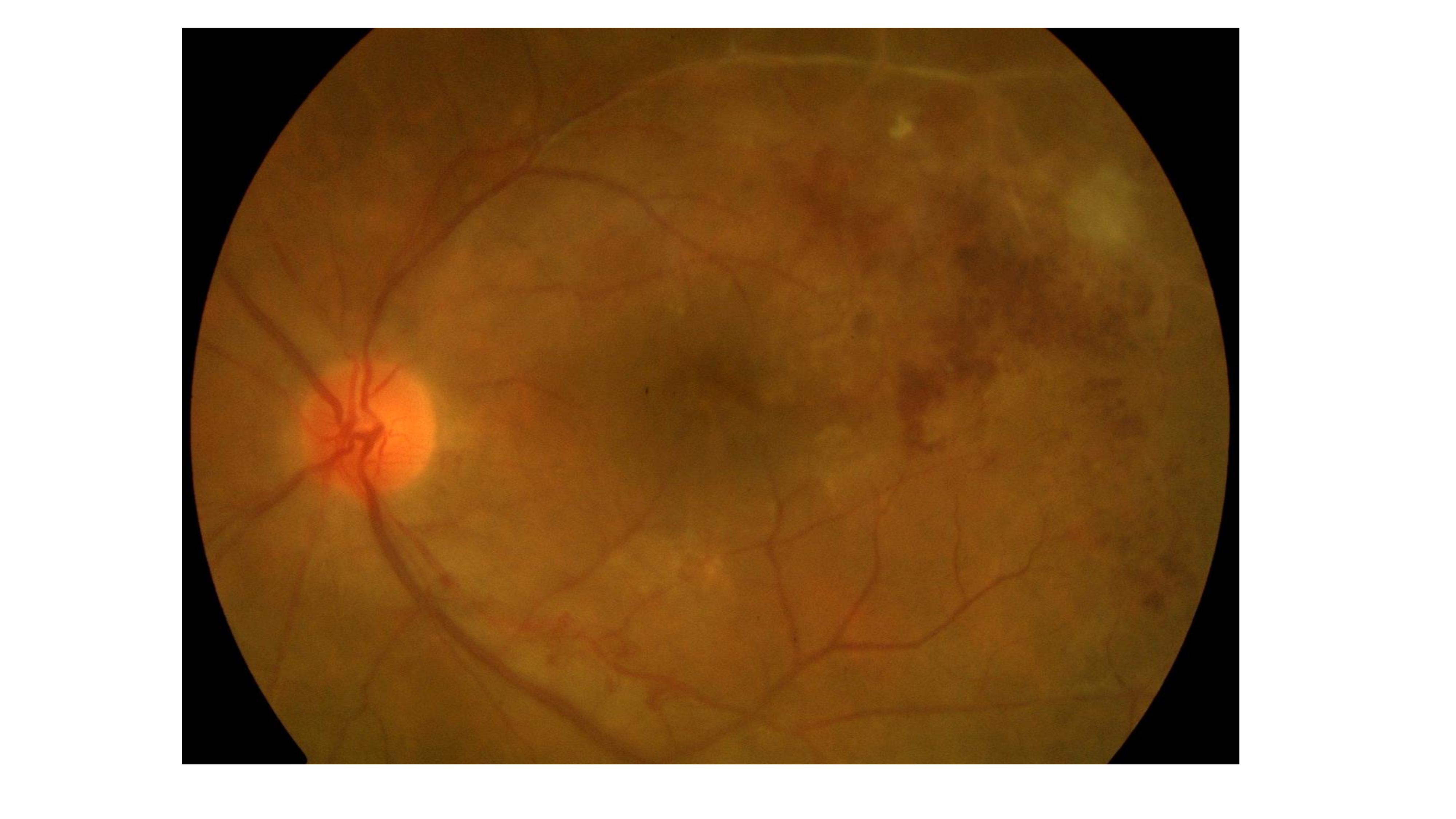
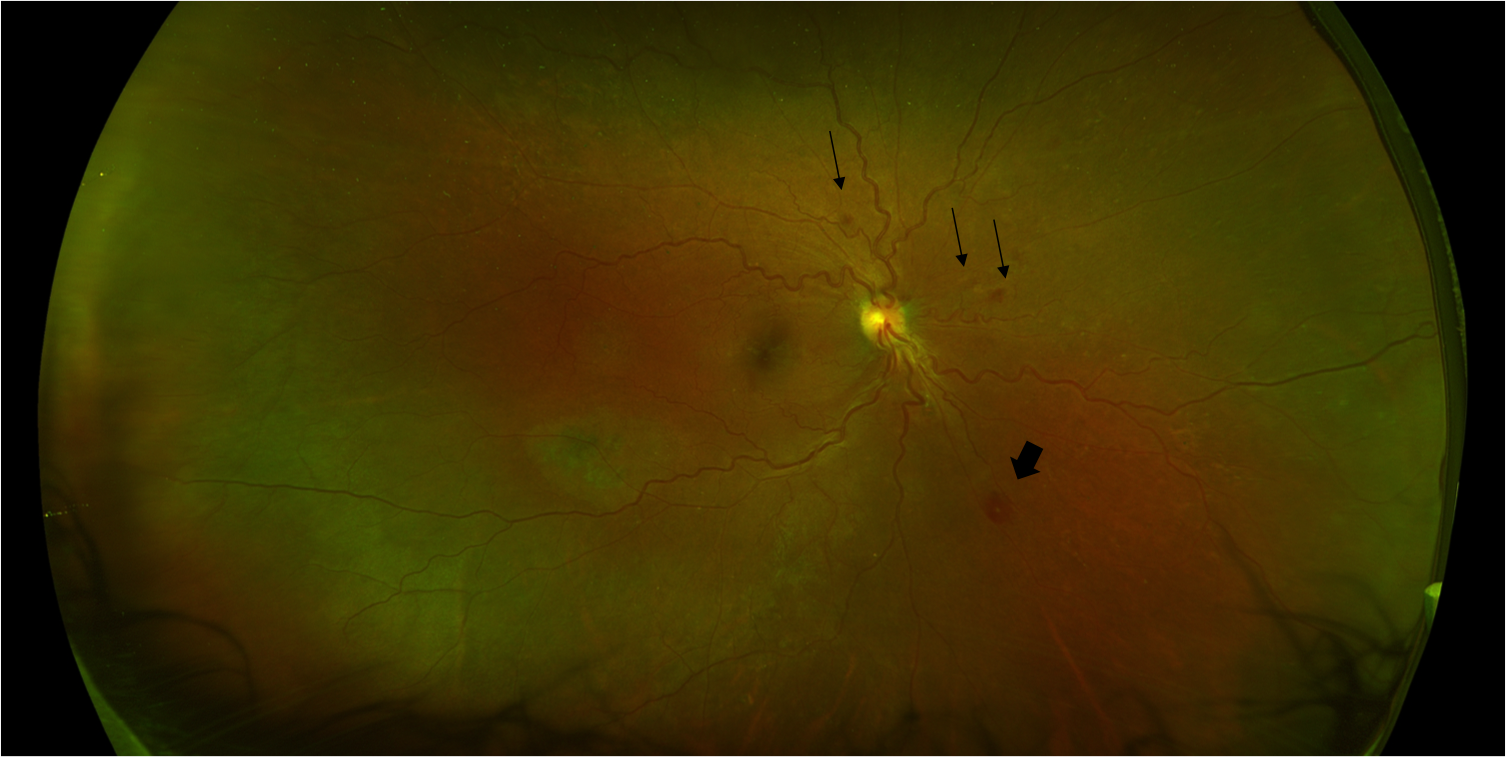
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Video to Play)
References
Agrawal S, Peters MJ, Adams GG, Pierce CM. Prevalence of retinal hemorrhages in critically ill children. Pediatrics. 2012 Jun:129(6):e1388-96. doi: 10.1542/peds.2011-2772. Epub 2012 May 21 [PubMed PMID: 22614777]
Level 2 (mid-level) evidenceWatts P, Maguire S, Kwok T, Talabani B, Mann M, Wiener J, Lawson Z, Kemp A. Newborn retinal hemorrhages: a systematic review. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2013 Feb:17(1):70-8. doi: 10.1016/j.jaapos.2012.07.012. Epub 2013 Jan 28 [PubMed PMID: 23363882]
Level 1 (high-level) evidenceBinenbaum G, Mirza-George N, Christian CW, Forbes BJ. Odds of abuse associated with retinal hemorrhages in children suspected of child abuse. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2009 Jun:13(3):268-72. doi: 10.1016/j.jaapos.2009.03.005. Epub [PubMed PMID: 19541267]
Level 2 (mid-level) evidenceLiu Z,Pan X,Bi H, Treatment of Valsalva retinopathy. Optometry and vision science : official publication of the American Academy of Optometry. 2014 Nov; [PubMed PMID: 25279780]
Level 3 (low-level) evidenceKaur B, Taylor D. Retinal haemorrhages. Archives of disease in childhood. 1990 Dec:65(12):1369-72 [PubMed PMID: 2103739]
Ozturker ZK, Munro K, Gupta N. Optic disc hemorrhages in glaucoma and common clinical features. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2017 Dec:52(6):583-591. doi: 10.1016/j.jcjo.2017.04.011. Epub 2017 Jun 26 [PubMed PMID: 29217027]
Uhler TA, Piltz-Seymour J. Optic disc hemorrhages in glaucoma and ocular hypertension: implications and recommendations. Current opinion in ophthalmology. 2008 Mar:19(2):89-94. doi: 10.1097/ICU.0b013e3282f3e6bc. Epub [PubMed PMID: 18301280]
Level 3 (low-level) evidenceLoughrey PB,Armstrong D,Lockhart CJ, Classical eye signs in bacterial endocarditis. QJM : monthly journal of the Association of Physicians. 2015 Nov; [PubMed PMID: 25762500]
Level 3 (low-level) evidenceLing R, James B. White-centred retinal haemorrhages (Roth spots). Postgraduate medical journal. 1998 Oct:74(876):581-2 [PubMed PMID: 10211348]
Level 3 (low-level) evidenceKhawly JA, Pollock SC. Litten's sign (Roth's spots) in bacterial endocarditis. Archives of ophthalmology (Chicago, Ill. : 1960). 1994 May:112(5):683-4 [PubMed PMID: 8185527]
Level 3 (low-level) evidenceMiguel AI, Henriques F, Azevedo LF, Loureiro AJ, Maberley DA. Systematic review of Purtscher's and Purtscher-like retinopathies. Eye (London, England). 2013 Jan:27(1):1-13. doi: 10.1038/eye.2012.222. Epub 2012 Nov 23 [PubMed PMID: 23174749]
Level 1 (high-level) evidenceHochman MA, Seery CM, Zarbin MA. Pathophysiology and management of subretinal hemorrhage. Survey of ophthalmology. 1997 Nov-Dec:42(3):195-213 [PubMed PMID: 9406367]
Level 3 (low-level) evidenceMennel S. Subhyaloidal and macular haemorrhage: localisation and treatment strategies. The British journal of ophthalmology. 2007 Jul:91(7):850-2 [PubMed PMID: 17576704]
Czorlich P, Skevas C, Knospe V, Vettorazzi E, Richard G, Wagenfeld L, Westphal M, Regelsberger J. Terson syndrome in subarachnoid hemorrhage, intracerebral hemorrhage, and traumatic brain injury. Neurosurgical review. 2015 Jan:38(1):129-36; discussion 136. doi: 10.1007/s10143-014-0564-4. Epub 2014 Aug 31 [PubMed PMID: 25173620]
Duane TD. Valsalva hemorrhagic retinopathy. Transactions of the American Ophthalmological Society. 1972:70():298-313 [PubMed PMID: 4663671]
Saxena S, Jalali S, Verma L, Pathengay A. Management of vitreous haemorrhage. Indian journal of ophthalmology. 2003 Jun:51(2):189-96 [PubMed PMID: 12831156]
Mills M. Funduscopic lesions associated with mortality in shaken baby syndrome. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 1998 Apr:2(2):67-71 [PubMed PMID: 10530965]
Maguire S, Pickerd N, Farewell D, Mann M, Tempest V, Kemp AM. Which clinical features distinguish inflicted from non-inflicted brain injury? A systematic review. Archives of disease in childhood. 2009 Nov:94(11):860-7. doi: 10.1136/adc.2008.150110. Epub 2009 Jun 15 [PubMed PMID: 19531526]
Level 1 (high-level) evidenceKitagawa Y, Shimada H, Mori R, Tanaka K, Yuzawa M. Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injection for Submacular Hemorrhage in Polypoidal Choroidal Vasculopathy. Ophthalmology. 2016 Jun:123(6):1278-86. doi: 10.1016/j.ophtha.2016.01.035. Epub 2016 Mar 2 [PubMed PMID: 26949121]
Sato T, Morita S, Bando H, Sato S, Ikeda T, Emi K. Early vitreous hemorrhage after vitrectomy with preoperative intravitreal bevacizumab for proliferative diabetic retinopathy. Middle East African journal of ophthalmology. 2013 Jan-Mar:20(1):51-5. doi: 10.4103/0974-9233.106387. Epub [PubMed PMID: 23580852]
Kaur B, Taylor D. Fundus hemorrhages in infancy. Survey of ophthalmology. 1992 Jul-Aug:37(1):1-17 [PubMed PMID: 1509354]
Level 3 (low-level) evidence