Introduction
The blood supply to the vertebral canal is critical especially from the context of surgical and clinical considerations. The spinal cord located within the vertebral canal allows for a neuronal connection between the brain and the rest of the body and thus the blood supply to this structure is of vital importance. In this review, we go over the blood supply as well as additional information regarding the structure, function, variants, clinical, and surgical significance associated with the vertebral canal.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Structure general:
The spinal cord initiates at the base of the foramen magnum and extends to conus medullaris which ends, on average, between spinal vertebrae L1-L2 but can end as early as T12 or as far down as between L2-L3. The spinal cord is surrounded by the meninges consisting of the dura mater, arachnoid mater, and pia mater; the end of the subarachnoid space terminates around the S2 vertebrae. The vertebral canal is 33 vertebrae of which seven are cervical, 12 are thoracic, five are lumbar, and 5 are sacral along with four coccygeal.[1]
Structure vertebrae:
- The vertebral body is the main weight bearing aspect of the vertebral column, separated by the intervertebral discs (which allow cushioning). The size increases as the vertebrae move caudally, so the lumbar bodies are the largest ones which also bear the most weight.
- The vertebral arch forms the posterior and lateral aspects of the vertebrae with a central lumen in the middle which forms the vertebral canal where the spinal cord exists. The arch is made of pedicles which attach the arch to the body and the laminae which extend from each pedicle to meet at the midline and close off the arch; from where the spinous process also forms.
- The superior articular processes and inferior articular processes are located on each side of the pedicles connect with inferior and superior articular processes respectively of the adjacent vertebrae to form the intervertebral foramen through which blood vessels and nerves can exit and enter the spinal cord.[1]
- Transverse processes are present on each vertebra; however, they differ between the cervical, thoracic, and lumbar. They form at the junction between the pedicle and laminae and face posterolaterally. In the cervical vertebrae, the transverse processes contain a luminal space called the transverse foramen through which the vertebral arteries course through on both sides.
Function:
The function of the spinal canal and vertebral column is to protect the spinal cord and provide support to the body. It includes foramen such that blood supply and nerves to and from the spinal cord can occur at every level.
Embryology
Blood vessels form from the mesoderm. During development as the nerve roots that will connect into the spinal cord start to form, they carry a radicular artery along their route to the spinal cord. However, from this point, some of these arteries will grow larger to supply more than just their spinal cord level while other arteries will spontaneously regress and thus why we do not have 31 theoretical radicular arteries.[2]
The vertebral arteries initially start as seven longitudinally connected intersegmental cervical arteries. The first six of these arteries eventually resorb leaving a single long anterior spinal artery which connects to the seven intersegmental cervical arteries that will ultimately become the subclavian artery, producing the normal anatomical structure of the vertebral artery.[3]
Blood Supply and Lymphatics
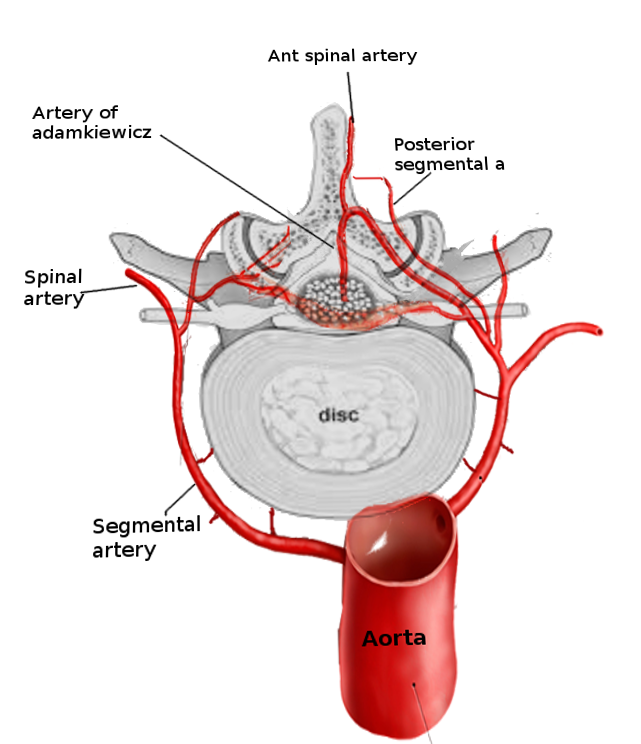
Arterial supply:
The vertebral blood supply for the spinal cord comes from many different sources in the body depending on the region. The main blood supply to the spinal cord is via the single anterior spinal artery (ASA) and the two posterior spinal arteries (PSA). The anterior spinal artery is formed by the vertebral arteries which originate from the first part of the subclavian artery. The vertebral arteries pass through the transverse foramen of C1 through C6 and through the foramen magnum to become the basilar artery. However, before joining together to become the basilar artery, the vertebral arteries each give off a branch which becomes the anterior spinal artery; the anterior spinal artery travels caudally down the spinal cord through the anterior sulcus.[4] The posterior spinal arteries can branch off the posterior inferior cerebellar artery (PICA) or branches from the pre-atlantal vertebral arteries which also travel caudally down the spinal cord but through the two posterior sulci.[5] The ASA provides blood to the anterior two-thirds of the spinal cord, and the PSA delivers blood to the posterior one-third of the spinal cord.
The anterior spinal artery and PSA are fed additional arteries throughout their course down the spinal cord at each spinal level through the intervertebral foramen. These additional arteries are called segmental spinal arteries. The segmental arteries then bifurcate into an anterior and posterior radicular artery which feed into both anterior and posterior spinal arteries respectively. Not only can they supply the ASA/PSA but also provide blood supply to the nerve roots along which they track. Theoretically there should be 31 radicular arteries for each foramen that receives an artery, but in reality, there is always less.[2] Sometimes, however, the spinal segmental arteries also give off segmental medullary arteries which directly feed into the anterior spinal artery and posterior spinal arteries, however, the numbers differ between person to person. There are thought to be anywhere from 8 to 10 in every person. The two anterior spinal arteries primarily supply the upper cervical spinal cord as they come off the vertebral arteries before they anastomose together into the single ASA.[4] The mid cervical spinal cord receives vascular supply by segmental medullary arteries coming from directly off the vertebral artery. The lower cervical to the upper thoracic spinal cord is supplied by radiculomedullary arteries arising from the cervicothoracic trunk C7 to T1 (either left or right).[2] Segmental spinal arteries supply the mid-thoracic region (T3 to T9) as they come off usually the posterior intercostal artery. The largest segmental medullary artery is the artery of Adamkiewicz also known as the greater anterior radiculomedullary artery. The artery of the Adamkiewicz (AKA) branches off the left side of the descending aorta around T8 to L2 (via lumbar or intercostal arteries) and connects on the ventral side of the spinal cord to supply the anterior spinal artery.[5][6] Of note, the artery of Adamkiewicz delivers vascular supply a large area of the thoracolumbar region and thus is considered a watershed area. Branches from the internal iliac arteries supply the lumbosacral spinal cord.[7]
Venous supply:
The spinal cord drains via the single anterior spinal vein and single posterior spinal vein which in turn drain into the internal vertebral venous plexus located in the epidural space within the extradural fat.[2] These veins eventually empty into the external vertebral venous plexus via the basivertebral veins. From the external venous plexus, blood drains systemically depending on the location; for example, the thoracic region of the spinal cord empties into the azygos system. Of note, the Batson venous plexus (which drains many organs in the pelvis region including bladder, prostate, and rectum) feeds into the internal vertebral plexus, and the Batson plexus does not contain valves.[7]
Physiologic Variants
Vertebral artery variants[3]:
- The most common variant is for the left vertebral artery to originate off the aortic arch between the left common and left subclavian artery with a prevalence of 2 to 5 %.
Artery of Adamkiewicz variants[8]:
- 75% of the time the artery inserts into the dura and ASA at the level T9-T12.
- 15% of the time the artery inserts into the dura and ASA at the level T5-T8.
- 10% of the time the artery inserted into the dura and ASA at the level L1-L2.
- There are two variants of ASA and AKA junction. The first variant seen describes a small caliber ASA which when joining with a larger caliber AKA forms a large ASA descending from that level. This variant is considered an AKA dominant circulation and disruption of the AKA in patients with this circulation could lead to severe neurological damage. Type 2 variant is where the ASA and AKA are the same calibers and upon joining together, the caliber of the ASA does not increase. In patients with type 2 circulation, the AKA is non-dominant, and thus disruption of the AKA in these patients might not lead to neurological damage right away.
Surgical Considerations
Posterior cervical spinal procedures can put a patient at risk for vertebral artery injury especially is the procedure requires the use of screws close to the proximity of the transverse foramen.[9] Thoracoabdominal aortic aneurysm surgery can often lead to lower spinal ischemia because of the disruption of blood flow to the artery of Adamkiewicz. Unilateral disruption of blood does not generally cause ischemia; however bilateral disruption can, which is often seen in the surgery for a thoracoabdominal aortic aneurysm and aortic dissection. However preoperative planning and identification of the artery of Adamkiewicz were led to fewer complications. However, preoperative imaging can be limited due to bony abnormalities in which case the continuity technique of tracing the artery of the aorta and into the ASA is imperative. Often a right-sided transthoracic approach is taken for anterior spinal surgeries to avoid the artery of Adamkiewicz because the majority of the time it originates from the left, reducing the chance of insulting the artery. Understanding where the artery of Adamkiewicz inserts into the ASA can also help with the identification of the AKA.[6] Disruption of the artery of Adamkiewicz can lead to paraplegia is the lower thoracic/lumbar spine becomes ischemic.
Clinical Significance
The artery of Adamkiewicz is considered a watershed area in the spinal cord and susceptible to infarction following episodes of severe hypotension. This area supplied by this artery is prone to ischemia and infarction because it is the last major artery feeding the lumbar spinal cord and makes a classic “hairpin loop” upon entry to the anterior spinal artery. There are generally no communication or anastomoses between the anterior and posterior spinal arteries thus making the artery of Adamkiewicz similar to an end artery. This vascular anatomy can often lead to anterior spinal cord syndrome within the region of the lumbar spinal cord leading to loss of motor function and sensory function carried by the anterior columns including pain and temperature (sparing proprioception within the dorsal column which is supplied by the posterior spinal artery). Diagnosis is made by MRI which can show classic “owl’s eye” hyperintensity on T2 axial images.[10]
Vertebral artery dissection is a rare origin of stroke but occurs more often in the younger population age less than 45 years old. They can occur from blunt trauma to the neck, chiropractic manipulation or connective tissue diseases. Tearing of the intimal layer leads to blood dissecting through other layers and forming hematomas within the arterial connective tissue and creating stenosis thus restricting blood flow to the brain. The prognosis is generally good with 80% of patients making a full recovery.[9][11]
The Batson venous plexus of the pelvis is a well-documented route of metastasis where carcinomas of the pelvis, namely the prostate, can hematogenously spread to the spinal cord, vertebral column and brain because of the valveless structure of the Batson plexus.[12]
Other Issues
During pregnancy, the extradural venous plexus can become engorged when the gravid uterus lay supine and restricts blood supply to the inferior vena cava. The blood would then shunt to the external venous plexus. Because of the increasing supply of blood to the area, some studies claim that fewer spinal anesthetics would be necessary during pregnancy.[13]
Media
References
DeSai C, Reddy V, Agarwal A. Anatomy, Back, Vertebral Column. StatPearls. 2024 Jan:(): [PubMed PMID: 30247844]
Demondion X, Lefebvre G, Fisch O, Vandenbussche L, Cepparo J, Balbi V. Radiographic anatomy of the intervertebral cervical and lumbar foramina (vessels and variants). Diagnostic and interventional imaging. 2012 Sep:93(9):690-697. doi: 10.1016/j.diii.2012.07.008. Epub 2012 Aug 9 [PubMed PMID: 22883939]
Yuan SM. Aberrant Origin of Vertebral Artery and its Clinical Implications. Brazilian journal of cardiovascular surgery. 2016 Feb:31(1):52-9. doi: 10.5935/1678-9741.20150071. Epub [PubMed PMID: 27074275]
Ali F, Reddy V, Dublin AB. Anatomy, Back, Anterior Spinal Artery. StatPearls. 2023 Jan:(): [PubMed PMID: 30422558]
Boll DT, Bulow H, Blackham KA, Aschoff AJ, Schmitz BL. MDCT angiography of the spinal vasculature and the artery of Adamkiewicz. AJR. American journal of roentgenology. 2006 Oct:187(4):1054-60 [PubMed PMID: 16985157]
Lindeire S, Hauser JM. Anatomy, Back, Artery Of Adamkiewicz. StatPearls. 2024 Jan:(): [PubMed PMID: 30422566]
Singh U, Silver JR, Welply NC. Hypotensive infarction of the spinal cord. Paraplegia. 1994 May:32(5):314-22 [PubMed PMID: 8058348]
Level 3 (low-level) evidenceN'da HA, Chenin L, Capel C, Havet E, Le Gars D, Peltier J. Microsurgical anatomy of the Adamkiewicz artery-anterior spinal artery junction. Surgical and radiologic anatomy : SRA. 2016 Jul:38(5):563-7. doi: 10.1007/s00276-015-1596-3. Epub 2015 Dec 1 [PubMed PMID: 26627692]
Simon LV, Nassar AK, Mohseni M. Vertebral Artery Injury. StatPearls. 2024 Jan:(): [PubMed PMID: 29262106]
Kaiser JT, Reddy V, Lugo-Pico JG. Anatomy, Back, Spinal Cord Arteries. StatPearls. 2024 Jan:(): [PubMed PMID: 30725904]
Britt TB, Agarwal S. Vertebral Artery Dissection. StatPearls. 2024 Jan:(): [PubMed PMID: 28722857]
Maccauro G, Spinelli MS, Mauro S, Perisano C, Graci C, Rosa MA. Physiopathology of spine metastasis. International journal of surgical oncology. 2011:2011():107969. doi: 10.1155/2011/107969. Epub 2011 Aug 10 [PubMed PMID: 22312491]
Hirabayashi Y, Shimizu R, Fukuda H, Saitoh K, Igarashi T. Soft tissue anatomy within the vertebral canal in pregnant women. British journal of anaesthesia. 1996 Aug:77(2):153-6 [PubMed PMID: 8881616]