Introduction
In 1958, Ida Jean Orlando started the nursing process that still guides nursing care today. Defined as a systematic approach to care using the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EDP) recommendations, and nursing intuition. Holistic and scientific postulates are integrated to provide the basis for compassionate, quality-based care.[1][2][3]
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
The nursing process functions as a systematic guide to client-centered care with 5 sequential steps. These are assessment, diagnosis, planning, implementation, and evaluation.
Assessment
Assessment is the first step and involves critical thinking skills and data collection; subjective and objective. Subjective data involves verbal statements from the patient or caregiver. Objective data is measurable, tangible data such as vital signs, intake and output, and height and weight.
Data may come from the patient directly or from primary caregivers who may or may not be direct relation family members. Friends can play a role in data collection. Electronic health records may populate data and assist in assessment.
Critical thinking skills are essential to assessment, thus the need for concept-based curriculum changes.
Diagnosis
The formulation of a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The North American Nursing Diagnosis Association (NANDA) provides nurses with an up-to-date list of nursing diagnoses. A nursing diagnosis, according to NANDA, is defined as a clinical judgment about responses to actual or potential health problems on the part of the patient, family, or community.
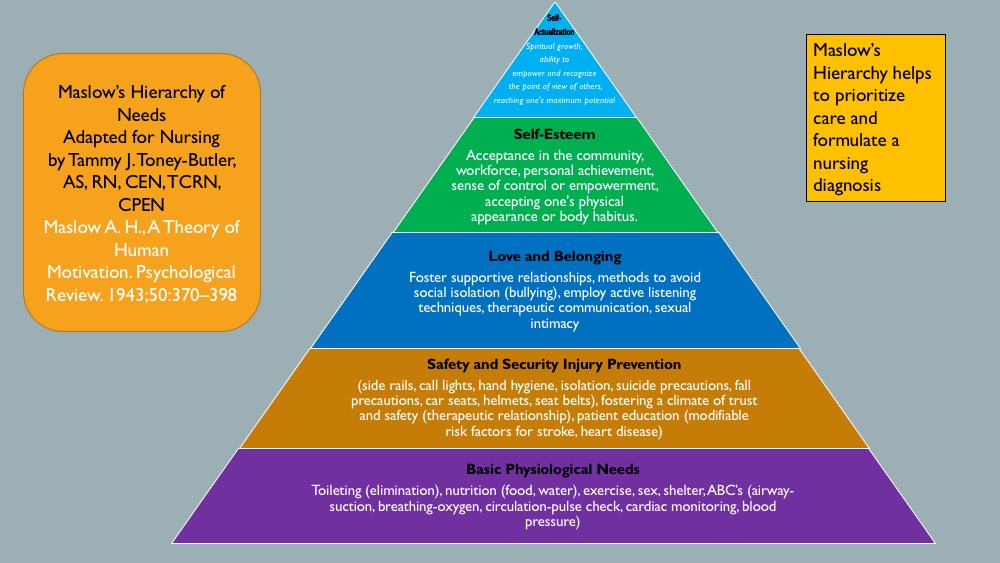
A nursing diagnosis encompasses Maslow's Hierarchy of Needs and helps to prioritize and plan care based on patient-centered outcomes. In 1943, Abraham Maslow developed a hierarchy based on basic fundamental needs innate to all individuals. Basic physiological needs/goals must be met before higher needs/goals can be achieved such as self-esteem and self-actualization. Physiological and safety needs provide the basis for the implementation of nursing care and nursing interventions. Thus, they are at the base of Maslow's pyramid, laying the foundation for physical and emotional health.[4][5]
Maslow's Hierarchy of Needs
- Basic Physiological Needs: Nutrition (water and food), elimination (Toileting), airway (suction)-breathing (oxygen)-circulation (pulse, cardiac monitor, blood pressure) (ABCs), sleep, sex, shelter, and exercise.
- Safety and Security: Injury prevention (side rails, call lights, hand hygiene, isolation, suicide precautions, fall precautions, car seats, helmets, seat belts), fostering a climate of trust and safety (therapeutic relationship), patient education (modifiable risk factors for stroke, heart disease).
- Love and Belonging: Foster supportive relationships, methods to avoid social isolation (bullying), employ active listening techniques, therapeutic communication, and sexual intimacy.
- Self-Esteem: Acceptance in the community, workforce, personal achievement, sense of control or empowerment, accepting one's physical appearance or body habitus.
- Self-Actualization: Empowering environment, spiritual growth, ability to recognize the point of view of others, reaching one's maximum potential.
Planning
The planning stage is where goals and outcomes are formulated that directly impact patient care based on EDP guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual's unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Goals should be:
- Specific
- Measurable or Meaningful
- Attainable or Action-Oriented
- Realistic or Results-Oriented
- Timely or Time-Oriented
Implementation
Implementation is the step that involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This phase requires nursing interventions such as applying a cardiac monitor or oxygen, direct or indirect care, medication administration, standard treatment protocols, and EDP standards.
Evaluation
This final step of the nursing process is vital to a positive patient outcome. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. Reassessment may frequently be needed depending upon overall patient condition. The plan of care may be adapted based on new assessment data.
Issues of Concern
According to a 2011 study conducted in Mekelle Zone hospitals, nurses lack the knowledge to implement the nursing process into practice and factors such as nurse-patient ratios inhibit them from doing so. Ninety percent of study participants lacked sufficient experience to apply the nursing process to standard practice. The study also concluded that a shortage of available resources, coupled with increased workloads due to high patient-nurse ratios, contributed to the lack of the nursing process implementation in the delivery of patient care.[6][7][8]
Clinical Significance
The utilization of the nursing process to guide care is clinically significant going forward in this dynamic, complex world of patient care. Aging populations carry with them a multitude of health problems and inherent risks of missed opportunities to spot a life-altering condition.
As explored by Salmond and Echevarria, healthcare is changing, and the traditional roles of nurses are transforming to meet the demands of this new healthcare environment. Nurses are in a position to promote change and impact patient delivery care models in the future.[9][10]
Other Issues
Critical thinking skills will play a vital role as we develop plans of care for these patient populations with multiple comorbidities and embrace this challenging healthcare arena. Thus, the trend towards concept-based curriculum changes will assist us in the navigation of these uncharted waters.
Concept-Based Curriculum
Baron further explores this need for a concept-based curriculum as opposed to the traditional educational model and the challenges faced with its implementation. A direct impact on quality patient care and positive outcomes. Nursing practice and educational environments form a bond with clinical knowledge and expertise, and that bond facilitates the transition into the current workforce as an indispensable team player and leader in this new wave of healthcare.
Learning should be the focus and the integration into current practice. Learning is a dynamic process, propelled by a force that must coexist within the same learning milieu between educator and student, preceptor and novice, mentor, and trainee.
IN the future, nurses must be able to problem-solve in a multitude of situations and conditions to meet these new adversities: challenging nurse-patient ratios, multifaceted approaches to prioritization of care, fewer resources, navigation of the electronic health record as well as functionality within the team dynamic and leadership style.
Media
(Click Image to Enlarge)
References
Karttunen M, Sneck S, Jokelainen J, Elo S. Nurses' self-assessments of adherence to guidelines on safe medication preparation and administration in long-term elderly care. Scandinavian journal of caring sciences. 2020 Mar:34(1):108-117. doi: 10.1111/scs.12712. Epub 2019 May 6 [PubMed PMID: 31058362]
Younan L, Clinton M, Fares S, Samaha H. The translation and cultural adaptation validity of the Actual Scope of Practice Questionnaire. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. 2019 Apr 25:25(3):181-188. doi: 10.26719/emhj.18.028. Epub 2019 Apr 25 [PubMed PMID: 31054228]
Epstein AS, Desai AV, Bernal C, Romano D, Wan PJ, Okpako M, Anderson K, Chow K, Kramer D, Calderon C, Klimek VV, Rawlins-Duell R, Reidy DL, Goldberg JI, Cruz E, Nelson JE. Giving Voice to Patient Values Throughout Cancer: A Novel Nurse-Led Intervention. Journal of pain and symptom management. 2019 Jul:58(1):72-79.e2. doi: 10.1016/j.jpainsymman.2019.04.028. Epub 2019 Apr 26 [PubMed PMID: 31034869]
Shih CY, Huang CY, Huang ML, Chen CM, Lin CC, Tang FI. The association of sociodemographic factors and needs of haemodialysis patients according to Maslow's hierarchy of needs. Journal of clinical nursing. 2019 Jan:28(1-2):270-278. doi: 10.1111/jocn.14532. Epub 2018 Jul 30 [PubMed PMID: 29777561]
Maslow K, Mezey M. Recognition of dementia in hospitalized older adults. The American journal of nursing. 2008 Jan:108(1):40-9; quiz, 50 [PubMed PMID: 18156858]
Raso A, Ligozzi L, Garrino L, Dimonte V. Nursing profession and nurses' contribution to nursing education as seen through students' eyes: A qualitative study. Nursing forum. 2019 Jul:54(3):414-424. doi: 10.1111/nuf.12349. Epub 2019 May 6 [PubMed PMID: 31056754]
Level 2 (mid-level) evidenceHu J, Yang Y, Fallacaro MD, Wands B, Wright S, Zhou Y, Ruan H. Building an International Partnership to Develop Advanced Practice Nurses in Anesthesia Settings: Using a Theory-Driven Approach. Journal of transcultural nursing : official journal of the Transcultural Nursing Society. 2019 Sep:30(5):521-529. doi: 10.1177/1043659619846248. Epub 2019 May 6 [PubMed PMID: 31060444]
Bird M, Tolan J, Carter N. Baccalaureate Nursing Students' Perceptions of Learning in Mentored and Simulated Research Practica. The Journal of nursing education. 2019 May 1:58(5):290-293. doi: 10.3928/01484834-20190422-07. Epub [PubMed PMID: 31039263]
Salmond SW, Echevarria M, Allread V. Care Bundles: Increasing Consistency of Care. Orthopedic nursing. 2017 Jan/Feb:36(1):45-48. doi: 10.1097/NOR.0000000000000311. Epub [PubMed PMID: 28107300]
Rigolosi R, Salmond S. The journey to independent nurse practitioner practice. Journal of the American Association of Nurse Practitioners. 2014 Dec:26(12):649-57. doi: 10.1002/2327-6924.12130. Epub 2014 May 14 [PubMed PMID: 24824941]
Level 2 (mid-level) evidence