Introduction
The buccinator muscle is a square, bilateral muscle situated in the mobile and adaptable cheek area.[1] Couper and Myot coined the term "buccinator" in 1694, relating to blowing a trumpet. Notably, this muscle puffs out the cheeks, thus it is also referred to as the "trumpeter's muscle."[2] The buccinator is one of the first muscles to be activated by sucking during infancy.
The buccinator contributes to mastication, articulation, and deglutition. Additionally, this structure is a target during cosmetic procedures, being a muscle of facial expression. Botulinum toxin treatment of the buccinator reduces facial synkinesis or undesired involuntary muscle contraction accompanying volitional movements.[16]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The buccinator, the main cheek muscle, originates from the mandible, the maxilla's alveolar process, the mandible's alveolar part, and the pterygomandibular raphe. The muscle then inserts on the mouth's angle (modiolus) and the orbicularis oris. The buccinator lies deep to the facial skin, anterior border of the masseter, and more superficial muscles.[3]
The buccinator muscle is sometimes referred to as an accessory mastication muscle as it coordinates with the orbicularis oris and superior constrictor muscle during swallowing, mastication, blowing, and sucking. The buccinator compresses the cheek inward against the molars. Some authors propose that the muscle thickens the cheek mucosa, acting as a muscular hydrostat. This thickening enables the cheek to push food boluses toward the tongue.[4][5]
The buccinator's contraction pulls the corner of the mouth laterally. The muscle contracts gradually while closing the mouth and relaxes when the mouth opens. These actions maintain cheek tension, preventing buccal mucosal injury.
The buccinator helps retain and stabilize complete dentures. Research also shows that the muscle contributes to parafunctional movements, which include bruxism, finger-sucking, and thumbsucking.[6]
Deglutition occurs in phases. The buccinator plays a role in the oral and pharyngeal phases of swallowing. The buccinator and orbicularis oris generate a peristaltic wave-like contraction during the oral phase. This wave is subsequently transmitted to the pharynx.[7]
The buccinator is activated during mandibular movements like protrusion and retrusion, aiding in completing these actions.[8] Studies also reveal that the buccinator helps regulate parotid secretion, having small fibers inserted in the distal portion of the parotid duct.[9]
Embryology
The buccinator derives from the 2nd pharyngeal arch (hyoid arch). Facial muscles start to form between the 3rd and 8th week of development, arising from the laminae the premyeloblasts and myeloblasts produce on each side of the face. Five laminae develop during this time: temporal, occipital, infraorbital, mandibular, and cervical. The buccinator arises from the mandibular lamina.[10]
Blood Supply and Lymphatics
The main blood supply to the buccinator comes from the buccal, facial, and posterosuperior alveolar arteries. These vessels form an extensive anastomosis on the muscle's lateral surface and within its fibers. The buccal artery, a maxillary artery branch, supplies the buccinator's posterior part. This artery runs anteroinferiorly, either superficial or deep, to the lateral pterygoid muscle to reach the buccinator's posterior aspect.
The facial artery supplies the buccinator's posterior, inferior, and anterior parts via its numerous branches. The posterior buccal branch, the largest facial artery segment, supplies the posterior aspect of the muscle. Inferior buccal branches of the facial artery supply the inferior portion of the buccinator. The facial artery then runs anterosuperiorly to give off anterior buccal branches, which supply the anterior aspect of the muscle. The posterosuperior alveolar artery is a branch of the maxillary artery that enters the buccinator muscle posterosuperiorly and supplies the area.
The veins draining the buccinator empty into the pterygoid plexus and internal maxillary vein.
Nerves
The buccinator's sensory innervation comes from the long buccal nerve, a branch of the maxillary division of the trigeminal nerve (CN V2). Motor innervation of the muscle is via the temporal and cervical divisions of the facial nerve (CN VII).[11]
Muscles
The buccinator muscle fibers originate from 3 areas, giving rise to 3 muscular bundles. Two of the muscular bundles have a bony origin. The maxillary bundle arises from the buccal portion of the maxilla's alveolar process. The mandibular bundle originates from the buccal portion of the mandible's alveolar process. The longitudinal bundle emerges from the pterygomandibular raphe. The raphe connects the buccinator's posterior fibers to the superior constrictor muscle, the most superior pharyngeal constrictor (see Image. Muscles of the Cheek and Pharynx).
The fibers of all 3 bundles run anteriorly and descend through the modiolus, thus forming the musculature of the cheek. The buccinator fibers blend with orbicularis oris muscle fibers. The maxillary bundle fibers blend with the orbicularis oris muscle fibers at the mandibular lip. The mandibular bundle fibers run superiorly to the maxillary lip. The longitudinal bundle fibers travel toward the oral commissures to insert into the upper and lower lips.[12]
Laterally, the buccinator is related to the mandibular ramus, masseter and medial pterygoid muscles, buccal fat pad, and buccopharyngeal fascia. Medially, the buccinator is covered by the cheek's submucosa and mucosa. The parotid duct (Stenson's duct) pierces the buccinator muscle after crossing the masseter muscle. The duct then turns medially at the buccinator's anterior border, opening into the oral cavity into a small papilla opposite the maxillary 2nd molar.
Physiologic Variants
Attachment of the buccinator muscle into an alveolar ridge crest has been reported. The alveolar ridge holds the tooth sockets. Anomalous buccinator attachment to this area can impede toothbrush insertion into the mouth and adequate visualization during dental procedures.[17]
Surgical Considerations
The ease of lifting the buccinator makes it useful as a flap in reconstruction surgery. One application of this technique is the correction of small-to-medium oral cavity defects. Covering mucosal defects with a buccinator flap has very low morbidity at the donor site. The muscle is also remarkably elastic and, thus, can be stretched easily to conform to defects with a complex shape. The parotid duct, which pierces the buccinator muscle, should be identified and preserved during surgery.
Clinical Significance
Clinical conditions involving the buccinator include the following:[13][14]
- Buccinator hyperactivity can excessively compress the underlying hard tissues, resulting in narrow arches and malocclusion.
- Facial nerve damage can lead to buccinator paralysis and difficult mastication. Loss of buccinator function can cause repeated cheek mucosal lacerations.
- As previously mentioned, abnormal attachment of this muscle may interfere with proper prosthodontic management and oral hygiene maintenance. Abnormal buccinator attachments may also restrict cheek and lip movement, producing mastication and phonation difficulties.
- The tongue's outward force in the oral cavity balances the inward forces due to orbicularis oris and buccinator contraction. Therefore, denture molding for a completely edentulous patient must be guided by muscle function.
- The buccinator, orbicularis oris, and pharyngeal constrictors form a functional unit—the buccinator mechanism—essential to orofacial functions like swallowing, sucking, whistling, chewing, and vowel pronunciation. Food accumulates in the vestibule during chewing if the buccinator is weakened or paralyzed.
- The buccinator muscle stabilizes dentures in several ways. First, it grips the denture's polished surface. Second, the longitudinal fibers hold food boluses between the teeth during mastication. Third, the buccinator's maxillary bundle raises the upper denture. Fourth, the muscle's mandibular bundle depresses the lower denture.
- Synkinesis is a condition arising from nerve misfiring following an episode of facial weakness. Involuntary facial movements are triggered alongside voluntary actions, producing symptoms like pain, eating difficulty, and poor cosmesis. Botulinum toxin treatment of the buccinator can help improve facial synkinesis.
The buccinator plays a significant role in various oral functions and facial expressions. Therefore, understanding the clinical relevance of this muscle is vital in various medical fields.
Other Issues
The buccal space is a fascial space limited superomedially and inferomedially by the buccinator's maxillary and mandibular bundle fibers. The parotid gland and roots of the posterior teeth are related to this space. The fascial spaces confine early infection. However, inflammation can still spread due to the communication between fascial spaces. Fascial space interconnections may thus permit the spread of parotid and posterior tooth infections to nearby sites through the buccal space.[15]
Media
(Click Image to Enlarge)
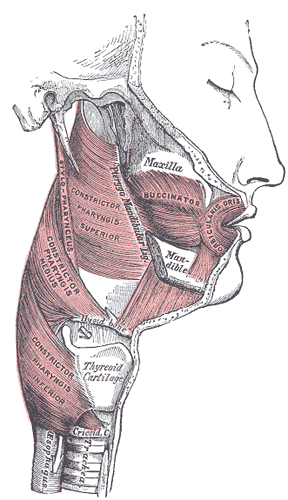
Muscles of the Cheek and Pharynx. This lateral-view image shows the buccinator, orbicularis oris, and constrictor pharyngis superior, medius, and inferior. The thyroid cartilage, trachea, upper esophagus, stylopharyngeus, maxilla, and mandible are also shown.
Henry Vandyke Carter, Public domain, via Wikimedia Commons
References
Baghele ON. Buccinator muscle repositioning. Journal of Indian Society of Periodontology. 2012 Jul:16(3):456-60. doi: 10.4103/0972-124X.100930. Epub [PubMed PMID: 23162347]
Level 3 (low-level) evidencePlas E, Deliac P, Garuet Lempirou A, Caix P, Bioulac B. The buccinator muscle: an original morphogenetical study. Morphologie : bulletin de l'Association des anatomistes. 2004 Apr:88(280):27-30 [PubMed PMID: 15214310]
Dutra EH, Caria PH, Rafferty KL, Herring SW. The buccinator during mastication: A functional and anatomical evaluation in minipigs. Archives of oral biology. 2010 Sep:55(9):627-38. doi: 10.1016/j.archoralbio.2010.06.004. Epub [PubMed PMID: 20621287]
Level 3 (low-level) evidenceMioche L, Hiiemae KM, Palmer JB. A postero-anterior videofluorographic study of the intra-oral management of food in man. Archives of oral biology. 2002 Apr:47(4):267-80 [PubMed PMID: 11922870]
D'Andrea E, Barbaix E. Anatomic research on the perioral muscles, functional matrix of the maxillary and mandibular bones. Surgical and radiologic anatomy : SRA. 2006 Jun:28(3):261-6 [PubMed PMID: 16547604]
Pancherz H. Activity of the temporal and masseter muscles in class II, division 1 malocclusions. An electromyographic investigation. American journal of orthodontics. 1980 Jun:77(6):679-88 [PubMed PMID: 6930165]
Perkins RE, Blanton PL, Biggs NL. Electromyographic analysis of the "baccinator mechanism" in human beings. Journal of dental research. 1977 Jul:56(7):783-94 [PubMed PMID: 269159]
Blanton PL, Biggs NL, Perkins RC. Electromyographic analysis of the buccinator muscle. Journal of dental research. 1970 Mar-Apr:49(2):389-94 [PubMed PMID: 5264602]
Kang HC, Kwak HH, Hu KS, Youn KH, Jin GC, Fontaine C, Kim HJ. An anatomical study of the buccinator muscle fibres that extend to the terminal portion of the parotid duct, and their functional roles in salivary secretion. Journal of anatomy. 2006 May:208(5):601-7 [PubMed PMID: 16637883]
Som PM, Naidich TP. Illustrated review of the embryology and development of the facial region, part 2: Late development of the fetal face and changes in the face from the newborn to adulthood. AJNR. American journal of neuroradiology. 2014 Jan:35(1):10-8. doi: 10.3174/ajnr.A3414. Epub 2013 Mar 14 [PubMed PMID: 23493895]
Vitti M, Basmajian JV, Ouellette PL, Mitchell DL, Eastmen WP, Seaborn RD. Electromyographic investigations of the tongue and circumoral muscular sling with fine-wire electrodes. Journal of dental research. 1975 Jul-Aug:54(4):844-9 [PubMed PMID: 1057568]
da Silva RH, Porciúncula HF, Jardini RS, Pita AP, Ribeiro AP. External location of the buccinator muscle to facilitate electromyographic analysis. Brazilian dental journal. 2008:19(2):130-3 [PubMed PMID: 18568227]
Howland JP, Brodie AG. Pressures exerted by the buccinator muscle. The Angle orthodontist. 1966 Jan:36(1):1-12 [PubMed PMID: 5218760]
Fränkel R. Decrowding during eruption under the screening influence of vestibular shields. American journal of orthodontics. 1974 Apr:65(4):372-406 [PubMed PMID: 4522227]
Paonessa DF, Goldstein JC. Anatomy and physiology of head and neck infections (with emphasis on the fascia of the face and neck). Otolaryngologic clinics of North America. 1976 Oct:9(3):561-80 [PubMed PMID: 980495]