Introduction
The leptomeningeal cyst (LMC) is an encapsulated mass occurring commonly in infants associated with skull fractures. The first description of the entity was made by Howship in 1816, as he described it as parietal bone absorption.[1] The term ‘Growing skull fracture’ was coined by Pia and Tonnis, whereas ‘Leptomeningeal cyst’ was coined by Dyke.[2][3] Synonyms of the LMC described in the literature include:
- Traumatic ventricular cysts.
- Cranio-cerebral erosions.
- Cranial malacia.
- Diploic cyst.
- Growing skull fracture.
- Cerebrocranial erosion.[2]
However, the term leptomeningeal cyst itself appears as a misnomer as the pathology is an encephalocele consisting of brain parenchyma with CSF and leptomeningeal layers and not an actual cyst.[4] In leptomeningeal cysts, there is a diastatic fracture of the skull involving both the outer and inner table and a laceration of the underlying dura meter. Diastatic fractures occur when there is a separation of the cranial sutures. It is an uncommon complication occurring in young infants and children under three years of age with skull fractures. Post-traumatic intradiploic leptomeningeal cysts are a variant in which the fracture involves the inner table with the dural tear. This leads to CSF accumulation in a sac lined by the arachnoid membrane and located within the diploic space. It is not synonymous with an arachnoid cyst. Since most cases occur in infants, it is postulated that the formation of the mass requires the presence of a rapidly growing brain. The inciting insult seems to be a dural tear accompanying a linear skull fracture creating an orifice for the intracranial contents to herniate. As the intracranial contents begin to escape, they create pressure on the surrounding skull, causing erosion of the bone margins and subsequently expanding the skull fracture. This tissue interposition inhibits osteoblast migration, hence impeding fracture healing. In addition, continued CSF pulsation enlarges the cyst causing the lesions to escape to the subgaleal space. The severity of the trauma and degree of diastasis (>4 mm) also appear to play a role.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Fall-related incidents are the most common causes of LMC.[5] The parietal bone is the site of occurrence.[3] Case reports have described the leptomeningeal cyst occurrence from reconstructive craniofacial surgeries and craniosynostosis reconstruction, including simple suturectomy and extensive calvarial vault remodeling.[6][7] Endoscopic repair has also been reported as a cause of leptomeningeal cysts.[8] In rare instances, vacuum extraction, a form of assisted delivery, is reported to cause leptomeningeal cysts in newborns.[9][10]
Epidemiology
The incidence of LMC is approximately 0.05% to 1.6%. More than 90% of these cases occur below three years of age.[3][11] This may be related to the following:
- The rapid growth of the brain and skull.
- Dense adherence of the underlying dura to the bone.
- Skulls are thinner and more deformable.[2]
One of the studies described the mean age at the trauma as 8.8 months and the mean age at presentation as 21.9 months, with a slight predominance in male infants.[12] Presentation in adults is rare and almost invariably has a preceding history of head trauma.[13][14]
Pathophysiology
Concurrent underlying dural tear with herniation of the brain elements egressing through the fracture site is the primary variable governing the development of LMC.[15]
Four essential prerequisites for the development of LMC include:
- Skull fractures are sustained mostly below three years of age.
- There is an underlying dural tear.
- This leads to the interposition and continuum herniation of brain elements through the defect based on the ‘ball-valve’ mechanism, and
- There occurs progressive advancement of the fracture line.[2][3][5]
Phases described in the development of LMC include:
- The first phase- includes skull fracture with an underlying dural tear.
- The second phase- includes healing of the fracture margins hindered by invagination and entrapment of arachnoids and governed by brain pulsation.
- The last phase- is characterized by bone diastasis alongside the leptomeningeal herniation.[16]
The progression of growing LMC has been described into three stages:
Histopathology
Histopathological tissue at surgery appears to be variable depending on the swelling content. The outer skull table appears thinned, and the mass is usually soft and connected to the underlying brain through a dura defect. The tissue was congruent with the gliotic brain.[4]
History and Physical
The scalp swelling is usually first brought to the attention of caregivers. Depending on the contents, the mass is either soft or hard. Progressive but painless scalp swelling is the most common pattern of clinical presentation.[18] The symptomatology varies regarding severity, chronicity, and injury site.[17] These include:
- Pulsatile scalp mass aggravated by cough and crying impulses.
- Headache.
- Loss of consciousness.
- Seizures.
- Neurological deficits.
- Impaired vision, squint, and proptosis.
- Mental retardation.
- Gross skull deformity.[3][19]
Neurological deficit (40%) and loss of consciousness (86%) are frequent among children who present late.[19] Delayed seizures and new onset/progression of deficits harbinger the disease evolution.[18] In adults, the initial presentation could be swelling associated with headaches and scalp paraesthesia-dysesthesia.
In a study of 440 patients, the mean presentation age was 21.9 months. 57.8% of them were males.[12] Another study comprising 67 patients showed 86.67% of patients sustained the injury prior to three years of age. Seizures were observed in 41.80% of cases.[19] There is a variable time lapse between the index injury and the clinical presentation of LMC, varying from <6 months to more than 20 years.[18][19]
Evaluation
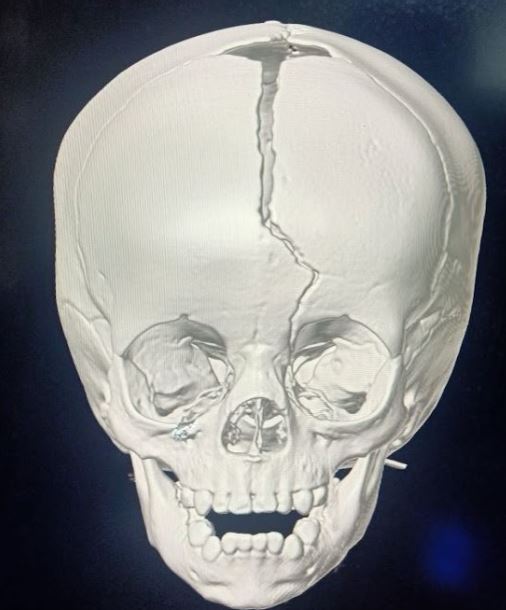
Diagnosis can be established with an antecedent history of trauma and neuroimaging modalities such as plain radiographs, computed tomography (CT), and magnetic resonance imaging (MRI). Imaging is imperative to define the extent of primary skull fracture and associated encephalomalacia, aid in surgical planning, and exclude other pathologies.
- Plain X-ray skull- early phase shows the diastatic fracture. Late lesions may show lytic lesions with scalloped margins.
- CT brain- In addition to the findings in the plain radiograph, the early phase shows concurrent lesions, with brain contusions being the most common finding.[19] In the late stage, CT imaging shows the presence of a leptomeningeal cyst, intradiploic cyst, encephalomalacia, porencephalic cyst, ventricular asymmetry, and hydrocephalus.[3][19] 3D CT is better at detecting fracture patterns.[20]
- MRI-The main advantage of MRI is early detection of the defect in the dura and concurrent herniated brain elements in high risks patients.[3]Patients with:
- Cephalhematoma
- Bone diastasis of 4 mm or more, and
- Underlying brain contusion should ideally have a contrast brain MRI to find out the dural tear and herniation of the brain matter.[15]
- Color Doppler imaging-useful for newborns who develop leptomeningeal cysts due to birth trauma.[21] Doppler imaging also reveals pulsatile arterial flow thought to be from the arterial flow in the dural space, thereby excluding avascular masses such as cephalhematoma or subgaleal bleeding. Doppler could also aid in evaluating for any concomitant venous injury.
- Seizures warrant evaluation with an electroencephalogram.
Three primary types of LMCs:
Treatment / Management
Early diagnosis and surgical intervention are crucial to avoid progressive and potentially permanent neurological sequelae. The surgical intervention of the leptomeningeal cyst involves a craniotomy, resection of the mass, repair of the dural defect with a pericranial patch, and repair with a bone graft. In one case report, fibrinogen-based collagen fleece was used as an alternative to dural repair. [23] The fibrinogen and thrombin imitate the last steps of the coagulation cascade. The coagulation factors dissolve upon contact with bleeding wounds or bodily fluids, and a link is formed between the collagen carrier and the wound surface.[23](B3)
Although primary closure of the dural defect is the definitive treatment, recurrence of the cyst (2%) remains possible.[12] Syndromic craniosynostosis, hydrocephalus, elevated intracranial pressure, repeated surgical interventions, endoscopic repair, and incomplete duraplasty/cranioplasty are all risk factors associated with the recurrence of leptomeningeal cysts. During initial craniosynostosis repair, mannitol can be administered to relax the brain and prevent injury to the dura.
The management of elevated intracranial pressure is crucial to prevent cyst recurrence. Surgically, increased intracranial pressure can be treated by resecting herniated brain matter and treating hydrocephalus. Repair should be delayed until herniated brain tissue is apparent on brain imaging. It is suggested that the repair be postponed until the edema subsides and the brain tissue retracts from the defect. However, if the herniated tissue continues despite sufficient surveillance, which is usually up to two months, excision of the nonfunctional tissue is required. After this period, it is unlikely that the cyst will regress spontaneously and generally continue to grow without surgical intervention.[12]
Ventriculoperitoneal (VP) shunting is another method that can be utilized to treat hydrocephalus or increased intracranial pressure.[6] In individuals with hydrocephalus, VP shunting and the resulting cerebrospinal fluid diversion may occasionally be used alone to treat recurrent leptomeningeal cysts.[24] Cranioplasty should preferably be performed with a bone graft secured with rigid absorbable screws and plates or absorbable sutures, although a split-thickness graft is also appropriate.[7](B3)
Pivotal Aspects in the Management
The salient surgical steps in the management include:
- Defining the edges of the bony defect.
- Wide craniotomy to expose the dural defect.
- Excision of the meningo-cerebral cicatrix.
- Watertight duroplasty.
- Repair of the bony defect.[19]
Watertight closure of the dural defect and cranioplasty is the mainstay of management. The dural defects are, on average, 1.42 times larger than the bony defects.[19] Wide exposure of the dural margins by liberal craniectomy is, therefore, of paramount importance.[16] The removal of the leptomeningeal cyst, followed by safe resection of the encephalomalacia, is undertaken.[3] Watertight closure of the dural defect through the use of autologous grafts such as pericranium and fascia lata have improved outcomes owing to better tissue compatibility and minimized risk of infections, adhesions, and rejections.[11] A split calvarial bone graft is advocated for children below three years old.[25] This, however, has increased the risk of resorption owing to brain pulsation.[11] Titanium mesh which has excellent biocompatibility, a low infection rate, and high mechanical strength, is preferred for cranioplasty.[5] Endoscopic-assisted duraplasty with the use of collagen matrix has also been described.[11](B3)
Orbital roof repair is required for orbitofrontal variants of LMC.[26] Lesions involving or in the vicinity of the major dural venous sinuses should ideally not be surgically intervened.[5](B3)
Differential Diagnosis
- Intradiploic encephalocele.
- Intradiploic arachnoid cyst.
- Post traumatic lipomas.
- Meningeal melanocytoma.
- Congenital parietal bone agenesis.
- Menkes disease.
- Eosinophilic granulomas.
- Langerhans cell histiocytosis.
- Multiple myelomas.
- Epidermoid cyst.
- Osteomyelitis.
- Calvarial metastasis.[19][27][28]
An intracranial epidermoid cyst is a rare congenital cyst that appears as lobulated lesions that fill and enlarge cerebrospinal fluid spaces and have the same density as cerebrospinal fluid on CT. On skull CT, Langerhans cell histiocytosis presents as solitary or multiple punched-out lytic lesions devoid of a sclerotic rim; "beveled edges" or "button sequestrum" may be observed due to the involvement of inner and outer tables.[29] Multiple myeloma of the calvarium manifests as well-defined lytic lesions without sclerotic rims (punched-out lesions) of varying sizes distributed throughout the skull.[29]
Osteomyelitis is characterized by focal bone lysis, cortical loss, periosteal thickening, and endosteal scalloping on plain radiographs. Depending on the underlying malignancy, calvarial metastasis manifests as either a lytic or sclerotic lesion; occasionally, mixed lytic and sclerotic lesions are observed. Metastatic lesions of the skull are frequently multiple; however, a single metastatic lesion may also be present.[29] The radiological appearance of congenital calvarial defects could vary depending on the condition, such as the partial or complete absence of cranial vault bones, abnormal cerebral hemisphere development, incomplete medical parietal bone suture, delayed or incomplete ossification of the membranous parietal bone. Other possible diagnoses include an intradiploic arachnoid cyst. These are likely congenital and result from a restriction in the flow of cerebrospinal fluid from the arachnoid granulations into the veins. These cysts typically manifest as localized pain, swelling, seizures, or neurological deficits late in life.[14]
Cephaloceles are congenital herniations of intracranial structures resulting from a skull defect.[30][31] Cephaloceles are classified based on the location and content of the herniated tissue. Meningocele is a protrusion of the meninges and cerebrospinal fluid only, whereas encephalocele involves a protrusion of the meninges, cerebrospinal fluid, and brain tissue. The encephalocystocele comprises meninges, cerebrospinal fluid, brain tissue, and ventricle. The term atretic cephalocele refers to a lesion in the midline that contains meninges, fibrous tissue, and dysplastic brain tissue.[32]
Prognosis
The leptomeningeal cyst is benign and carries a good prognosis. However, timely diagnosis and prompt surgical repair are crucial to avoiding long-term complications. The cyst can remain asymptomatic in some individuals; however, it still requires repair, given the risk of progressive enlargement and irreversible neurological complications. In addition, epilepsy, brain herniation with neurological deficit, and mental retardation can be associated with poor quality of life and significant morbidity.
Good-to-excellent outcomes, even in the delayed presentation, are observed in most cases.[18] In a study of 440 patients, dura-cranioplasty was performed in 61.6%.[12] Improvement in seizures and neurological deficits was noted in 12.7% and 7.05% of cases.[12]
Poor prognostic factors in one study included:
- Significant bony defect (>7 cm).
- Initial severe head injury.
- Calvarial defects crossing the midline, and
- Delayed repair (>8 months).[18]
Comminuted fracture (OR, 7.572) and the degree of diastasis (OR, 2.081 per mm diastasis) have a significant role in developing growing skull fractures.[33] Children at risk for developing GSF should be monitored clinically for up to 3 months following the initial insult.[12] A high index of suspicion is required among children with cephalohematoma persisting even after two weeks of trauma.[34]
Complications
Complications
- Rupture and subgaleal CSF collection.
- Ipsilateral ventricular dilatation.
- Hydrocephalus.
- Seizures.
- Progressive neurological deficits.
- Mental retardation.[2][35]
Complications of Surgery
- Wound infection.
- Subdural hygroma.
- CSF leaks and meningitis.
- Lesions communicating to the ventricles can lead to potentially life-threatening hemorrhagic complications due to sagging of the brain and rupture of draining veins.
- Recurrence.
- Mortality due to anesthesia and meningitis (reported in up to 8% of cases).[19][36]
Deterrence and Patient Education
Patients should be informed about the cause, disease course, and surgical management of the leptomeningeal cyst. Patients and families should be reassured regarding the benign nature of the cyst. In cases where children are affected, patients' families should be given detailed information about the complications and reminded to contact a physician or urgently present at the emergency room if there are any changes in the patient's clinical condition. Patients should be made aware of the likelihood of the cyst reoccurrence, although the reoccurrence is quite rare. It is essential that the necessity of multispecialty involvement in the patient's treatment and regular multispecialty follow-up with the neurosurgeon, neurologist, and pediatrician, be emphasized. Patients or parents should be warned of several long-term neurological issues that may have a prolonged or unpredictable course of recovery, such as mental retardation, motor weakness, speech disorders, and vision problems, and appropriate assistance should be provided.
Careful observation and education of the parents are pivotal.[25] Early recognition, prompt diagnosis, and timely surgery are the most pivotal aspects of management.[3] The use of a baby helmet after the operation can prevent recurrences.[34]
Enhancing Healthcare Team Outcomes
Children with scalp swelling, especially those under the age of three, warrant urgent evaluation. If the swelling remains persistent and there are associated neurological signs, the child should immediately be assessed by a pediatric neurologist or a neurosurgeon. The optimum management of a leptomeningeal cyst requires an interprofessional approach involving several specialists, such as an emergency physician, pediatrician, pediatric neurologist, pediatric neurosurgeon, pediatric epilepsy specialist, physical therapist, occupational therapist, and speech therapist. In addition, as a result of the fact that neurological deficits can result in mental retardation, speech problems, weakness, and emotional distress in the parents, it is necessary to consult with a psychologist or psychiatrist. Interprofessional care coordination with open communication channels will yield the best results for these patients. [Level 5]
Media
(Click Image to Enlarge)
References
Bir SC,Kalakoti P,Notarianni C,Nanda A, John Howship (1781-1841) and growing skull fracture: historical perspective. Journal of neurosurgery. Pediatrics. 2015 Oct [PubMed PMID: 26186359]
Level 3 (low-level) evidenceKumar A,Jaiswal G,Kankane VK,Kumar PK,Gupta TK, Arrested Hydrocephalus Complicated by Growing Skull Fracture - A Case Report with Review of Literature. Journal of pediatric neurosciences. 2020 Jul-Sep [PubMed PMID: 33531942]
Level 3 (low-level) evidenceChoi JI,Kim SD, Pediatric Minor Traumatic Brain Injury : Growing Skull Fracture, Traumatic Cerebrospinal Fluid Leakage, Concussion. Journal of Korean Neurosurgical Society. 2022 May [PubMed PMID: 35468709]
Britz GW,Kim DK,Mayberg MR, Traumatic leptomeningeal cyst in an adult: a case report and review of the literature. Surgical neurology. 1998 Nov; [PubMed PMID: 9842874]
Level 3 (low-level) evidenceMendpara V,Sahu S,Madhu K,Tarannum Shaik S,Maram MR,Natarajan B,Movva S,Sayed Mushir Ali A,Chauhan DR, Cranioplasty for a Growing Fracture of the Skull: A Case Report. Cureus. 2022 Oct [PubMed PMID: 36381935]
Level 3 (low-level) evidenceZemann W,Metzler P,Jacobsen C,Kruse AL,Lübbers HT,Könü D,Obwegeser JA, Growing skull fractures after craniosynostosis repair: risk factors and treatment algorithm. The Journal of craniofacial surgery. 2012 Sep; [PubMed PMID: 22948644]
Abuzayed B,Tuzgen S,Canbaz B,Yuksel O,Tutunculer B,Sanus GZ, Reconstruction of growing skull fracture with in situ galeal graft duraplasty and porous polyethylene sheet. The Journal of craniofacial surgery. 2009 Jul; [PubMed PMID: 19553832]
Aryan HE,Meltzer HS,Gerras GG,Jandial R,Levy ML, Leptomeningeal cyst development after endoscopic craniosynostosis repair: case report. Neurosurgery. 2004 Jul; [PubMed PMID: 15214995]
Level 3 (low-level) evidenceDjientcheu VD,Rilliet B,Delavelle J,Argyropoulo M,Gudinchet F,de Tribolet N, Leptomeningeal cyst in newborns due to vacuum extraction: report of two cases. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 1996 Jul; [PubMed PMID: 8869777]
Level 3 (low-level) evidenceCurtis J,King SJ,Weindling AM, Case report: Leptomeningeal cyst: an unusual complication of delivery by vacuum extraction. Clinical radiology. 1998 Nov; [PubMed PMID: 9833794]
Level 3 (low-level) evidenceKozaki Y,Nonaka M,Miki K,Tanaka H,Abe H,Inoue T, Endoscopic-assisted Duraplasty with Collagen Matrix for Growing Skull Fracture: A Case Report. NMC case report journal. 2021 [PubMed PMID: 35079464]
Level 3 (low-level) evidenceVezina N,Al-Halabi B,Shash H,Dudley RR,Gilardino MS, A Review of Techniques Used in the Management of Growing Skull Fractures. The Journal of craniofacial surgery. 2017 May; [PubMed PMID: 28060103]
S Bhatoe BH, Posterior Fossa Arachnoid Cyst Following Trauma in an Adult. Neurology India. 2022 May-Jun; [PubMed PMID: 35864686]
Bava J,Bansal A,Patil SB,Kale KA,Joshi AR, Posttraumatic Intradiploic Leptomeningeal Cyst: A Rare Complication of Head Trauma. Case reports in radiology. 2015; [PubMed PMID: 26558129]
Level 3 (low-level) evidenceSingh I,Rohilla S,Siddiqui SA,Kumar P, Growing skull fractures: guidelines for early diagnosis and surgical management. Child [PubMed PMID: 27023392]
Jain S,Gandhi A,Sharma A,Mittal RS, Growing skull fracture with cerebrospinal fluid fistula: A rare case report and its management strategies. Asian journal of neurosurgery. 2015 Jul-Sep; [PubMed PMID: 26396614]
Level 3 (low-level) evidenceKim I, Growing Skull Fracture in the Primary Motor Cortex in a 50-day-old Child: A Case Report. Korean journal of neurotrauma. 2020 Oct [PubMed PMID: 33163438]
Level 3 (low-level) evidencePrasad GL,Gupta DK,Mahapatra AK,Borkar SA,Sharma BS, Surgical results of growing skull fractures in children: a single centre study of 43 cases. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2015 Feb [PubMed PMID: 25227164]
Level 2 (mid-level) evidenceSinghal GD,Atri S,Suggala S,Jaluka D,Singhal S,Shrivastava AK, Growing Skull Fractures; Pathogenesis and Surgical Outcome. Asian journal of neurosurgery. 2021 Jul-Sep [PubMed PMID: 34660366]
Sim SY,Kim HG,Yoon SH,Choi JW,Cho SM,Choi MS, Reappraisal of Pediatric Diastatic Skull Fractures in the 3-Dimensional CT Era: Clinical Characteristics and Comparison of Diagnostic Accuracy of Simple Skull X-Ray, 2-Dimensional CT, and 3-Dimensional CT. World neurosurgery. 2017 Dec; [PubMed PMID: 28844920]
Voet D,Govaert P,Caemaert J,de Lille L,D'herde K,Afschrift M, Leptomeningeal cyst: early diagnosis by color Doppler imaging. Pediatric radiology. 1992; [PubMed PMID: 1437364]
Level 3 (low-level) evidenceNaim-Ur-Rahman,Jamjoom Z,Jamjoom A,Murshid WR, Growing skull fractures: classification and management. British journal of neurosurgery. 1994 [PubMed PMID: 7718163]
Level 3 (low-level) evidenceKim H,Jo KW, Treatment of a traumatic leptomeningeal cyst in an adult with fibrinogen-based collagen. Journal of Korean Neurosurgical Society. 2013 May; [PubMed PMID: 23908705]
Level 3 (low-level) evidenceKashiwagi S,Abiko S,Aoki H, Growing skull fracture in childhood. A recurrent case treated by shunt operation. Surgical neurology. 1986 Jul; [PubMed PMID: 3715702]
Level 3 (low-level) evidenceTamada I,Ihara S,Hasegawa Y,Aoki M, Surgical Treatment of Growing Skull Fracture: Technical Aspects of Cranial Bone Reconstruction. The Journal of craniofacial surgery. 2019 Jan [PubMed PMID: 30444774]
Singh V,Sasidharan GM,Bhat DI,Devi BI, Growing Skull Fracture and the Orbitocranial Variant: Nuances of Surgical Management. Pediatric neurosurgery. 2017 [PubMed PMID: 28427053]
Chen X,Dai H, Intradiploic encephalocele following linear skull fracture: a rare evolution of growing skull fracture. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2021 Dec [PubMed PMID: 33715079]
Tewfik K,Covelli C,Rossini M,Burlini D, Lump on the scalp of a child arising over a previous parietal fracture: growing skull fracture or post-traumatic lipoma? BMJ case reports. 2022 Apr 4 [PubMed PMID: 35379677]
Level 3 (low-level) evidenceGomez CK,Schiffman SR,Bhatt AA, Radiological review of skull lesions. Insights into imaging. 2018 Oct; [PubMed PMID: 30232767]
Diebler C,Dulac O, Cephaloceles: clinical and neuroradiological appearance. Associated cerebral malformations. Neuroradiology. 1983; [PubMed PMID: 6633855]
Naidich TP,Altman NR,Braffman BH,McLone DG,Zimmerman RA, Cephaloceles and related malformations. AJNR. American journal of neuroradiology. 1992 Mar-Apr; [PubMed PMID: 1566723]
Yokota A,Kajiwara H,Kohchi M,Fuwa I,Wada H, Parietal cephalocele: clinical importance of its atretic form and associated malformations. Journal of neurosurgery. 1988 Oct; [PubMed PMID: 3418387]
Lopez J,Chen J,Purvis T,Reategui A,Khavanin N,Iyer R,Manson PN,Dorafshar AH,Cohen AR,Redett RJ, Pediatric Skull Fracture Characteristics Associated with the Development of Leptomeningeal Cysts in Young Children after Trauma: A Single Institution [PubMed PMID: 32332544]
San Martín-García I,Aguilera-Albesa S,Zazpe-Cenoz I,Yoldi-Petri ME, [Recurring post-traumatic growing skull fracture]. Revista de neurologia. 2015 Apr 16 [PubMed PMID: 25857859]
Kulkarni AV,Dikshit P,Devi BI,Sadashiva N,Shukla D,Bhat DI, Unusual Complication of a Neglected Growing Skull Fracture. Pediatric neurosurgery. 2021 [PubMed PMID: 33626526]
Baldawa S, Remote intracranial hemorrhage following surgery for giant orbitofrontal growing skull fracture: A lesson learnt. Journal of pediatric neurosciences. 2016 Apr-Jun [PubMed PMID: 27606019]