Introduction
The supraclavicular block is a regional anesthetic technique used as an alternative or adjunct to general anesthesia or used for postoperative pain control for upper extremity surgeries (mid-humerus through the hand). First introduced in 1911 by Kulenkampff as a landmark-based approach, the associated risk of pneumothorax was likely responsible for the technique falling out of favor. [1] With the advent of ultrasonography, La Grange described the utilization of the Doppler probe to identify arteries in 1978. [2] Contemporarily, Kapral and colleagues advocated for the dynamic use of ultrasound to guide needle advancement in the supraclavicular position. [3] Colloquially known as the “spinal of the arm,” the supraclavicular block is advantageous as the brachial plexus nerves are tightly packed in this approach and speed of onset is often rapidly achieved. However, because of this consolidated relationship, consider restricting volumes of local anesthesia to as low as possible to achieve goals, as compression ischemia may occur.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The anterior rami of C5 to T1 form the brachial plexus, which exits the cervical spine to form the superior, middle, and inferior trunks that travel between the anterior and middle scalene muscles. Each trunk divides into an anterior and posterior branch, which subsequently rejoins to form the lateral, posterior, and medial cords as it travels distally to the clavicle. The supraclavicular approach blocks the brachial plexus from the distal trunks to the proximal cords but often is targeted at the divisions level. [4]
Indications
The supraclavicular block is indicated for primary regional anesthesia during surgeries and/or postoperative pain control to the distal two-thirds of the upper extremity, or from the mid-humerus to the fingertips. Sparing of very distal branches, especially the ulnar nerve, can occur. [5]
Contraindications
General contraindications to peripheral nerve blockade apply to supraclavicular block (e.g., patient refusal, allergy to local anesthetics, infection at injection site, malignancy at the needle entry site, and coagulopathy). Recent guidelines from the American Society for Regional Anesthesia and Pain Medicine (ASRA) should be followed as a supraclavicular block is considered a noncompressible or “deep block” site. A more superficial brachial plexus block should be considered for patients maintained on anticoagulation therapy. Additional caution is advised in patients with severe pulmonary disease as local anesthesia spread has resulted in cases of diaphragmatic paresis, and pneumothorax events (although less likely with ultrasound use) have occurred. [6] Finally, a regional block is not advised if preexisting neural deficits exist in the distribution of the block.
Equipment
The necessary equipment includes the following:
- Chlorhexidine gluconate or povidone iodine
- High-frequency ultrasound probe with sterile probe cover and gel
- Nerve stimulator (optional)
- Local anesthetic, typically 1% lidocaine, for superficial layer local anesthesia
- Regional block local anesthetic solution (0.5% bupivacaine or 0.5% ropivacaine for postoperative analgesia, and 2% lidocaine or 1.5% mepivacaine when shorter onset times are a necessity)
- 10 to 20 mL syringe with extension tubing
- Short bevel block needle (10 cm, 18 gauge for a continuous catheter or 22 gauge for single-injection)
Personnel
An anesthesiologist with training in ultrasound-guided regional anesthesia is preferable. Additional healthcare team members such as nursing staff with training in sedation anesthesia may assist.
Preparation
The provider must perform an informed consent process. A pre-procedure pause is done, and the patient is placed in the supine position with arms by the sides. The head is turned towards the contralateral side of the block. Consider elevating the head of the bed about 30 degrees. A towel roll may be needed under the ipsilateral shoulder to improve access to supraclavicular space. Mild sedation may be provided (typically 1 to 2 mg of midazolam and 50 to 100 mcg of fentanyl are provided through an IV), though some patients may not require sedation. Aseptic technique is employed. Chlorhexidine gluconate 2% or povidone-iodine solution is applied to the skin. Sterile conduction gel is applied to the ultrasound probe, and the use of a sterile probe cover is recommended.
Technique or Treatment
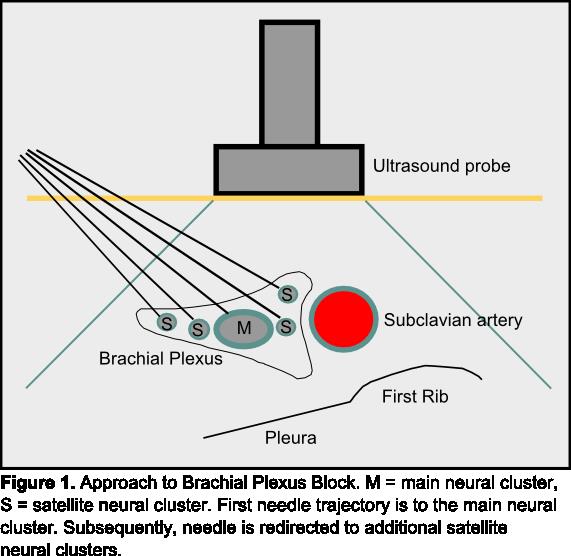
The ultrasound probe is placed in the supraclavicular fossa in the transverse orientation parallel to the clavicle and aimed inferior toward the ipsilateral thorax. The brachial plexus and the subclavian artery are visualized. The first rib appears as a hyperechoic line with the lung pleura deeper to this bony border. Utilizing the in-plane approach, the needle is advanced from lateral to medial, aimed for near the main neural cluster of the brachial plexus. After negative aspiration, local anesthetic (about 10 mL) is injected. Subsequently, smaller aliquots of local anesthetic are deposited near the surrounding satellite neural clusters. [7] Injection should be stopped if the patient experiences paresthesia or pain.
Another approach is "the corner pocket technique," first described by Soares and colleagues in 2007. [8] This involves a needle trajectory aimed towards the deeper portion of the brachial plexus with the goal of local anesthetic solution raising the brachial plexus off of the first rib. Then, the needle is retracted and advanced at a shallower angle, aiming toward the superficial brachial plexus. After negative aspiration, a local anesthetic is injected (about 10 mL). [9] This technique may have higher potential for pleural puncture.
Nerve stimulation may be utilized as an adjunct to ultrasound. [10] If this approach is utilized, the nerve stimulator must be connected before local anesthetic injection. With contraction of the arm, forearm, or wrist occurs below 0.4 mA, intraneural needle position may be likely, and the needle should be withdrawn and redirected. Neural pressure monitoring during proximal brachial plexus blocks has also been recommended as a high opening injection pressure (greater than or equal to 15 psi) is associated with more needle-to-nerve contacts and intraneural injection. [11]
Complications
General complications to peripheral nerve blockade apply to supraclavicular blocks including risk for infection, bleeding, and neuropathy. With the advent of ultrasonography, constant visualization of the needle tip, first rib, and pleura can decrease the risk for pneumothorax. Common, self-limited, side effects associated with other proximal brachial plexus blockade include hoarseness due to an ipsilateral laryngeal nerve block, Horner syndrome from stellate ganglion block, and hemidiaphragmatic paresis from a phrenic nerve blockade. [12] Local anesthetic systemic toxicity is also possible. The transverse cervical and dorsal scapular arteries lie anatomically close to the brachial plexus, and thus the use of color Doppler is recommended.
Clinical Significance
The ultrasound-guided supraclavicular block is performed typically at the distal trunk or proximal divisions level of the brachial plexus. While no confirmatory data exists, this location’s compactness may explain the supraclavicular block’s reputation for producing short latency and dense sensory and motor anesthesia. It can also be utilized for shoulder surgery but requires supplementation of the more proximal cervical nerves including supraclavicular nerve (C3 to C4) and suprascapular nerve (C5 to C6) for coverage of the cape of the shoulder.
The improved safety afforded by the use of ultrasound allowing visualization of the pleura has likely been the turning point in the increased use of supraclavicular blockade. [13] Gamo et al. demonstrated that ultrasound-guided supraclavicular block had a rapid procedure time (4 minutes), provided optimal intraoperative conditions with a mean surgery time of 75.2 minutes (range 6 to 232 minutes), and a mean of 437 minutes of postoperative analgesia. [14] Additionally, studies have demonstrated decreased pneumothorax and inadvertent vascular injury, and increased block success.
If ultrasound guidance is used, concomitant peripheral nerve stimulation may be redundant and has not been shown to increase the success rate of the block. Furthermore, there is a high false-negative rate, suggesting these ultrasound-guided blocks are typically effective even without a motor response. [15]
Which approach to brachial plexus blockade (e.g., supraclavicular, infraclavicular, interscalene, and axillary) you decide on ultimately depends on several patient, provider, and system-related factors including location of desired anesthetic coverage, operator experience, variation in anatomy, coagulopathy (compressible site preferred), infection over the intended site, and ability to appropriately position the patient. Also, it will depend upon the desired goal for primary anesthesia or postoperative analgesia. A prospective randomized study by Stav et al. comparing the efficacy of supraclavicular, infraclavicular, and axillary blocks in 101 patients demonstrated that all three approaches produced similar quality for surgical anesthesia for operations below the shoulder. [16] A meta-analysis by Guo et al. comparing supraclavicular blocks and interscalene blocks for shoulder surgery revealed no difference in procedural time, need for rescue analgesia, and dyspnea rates. However, the incidence of hoarseness and Horner syndrome was statistically lower in those receiving a supraclavicular block compared to those receiving an interscalene block. [17]
Enhancing Healthcare Team Outcomes
A supraclavicular block is usually performed by an anesthesiologist or anesthesia nurse with the help of a nurse. During the procedure, the nurse assists with sterile technique and making sure the medications and equipment are ready. Once the procedure is over, the patient is usually monitored by nurses in the recovery room. The nurses must be prepared and familer with expected complications and quickly report to back to the operative team.
All of these professionals need to know the adverse effects of anesthetics used for regional blocks. The majority of patients have no complications but a few patients may develop temporary paralysis of the brachial plexus. Due to the rarity of complications, it is easy to become lax. As such, re-education and continued interprofessional training is crucial. The best outcomes will be achieved by an interprofessional team approach where each member communicates with the team as challenges arise. [Level V]
Media
References
Kulenkampff D. BRACHIAL PLEXUS ANAESTHESIA: ITS INDICATIONS, TECHNIQUE, AND DANGERS. Annals of surgery. 1928 Jun:87(6):883-91 [PubMed PMID: 17865904]
la Grange P, Foster PA, Pretorius LK. Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block. British journal of anaesthesia. 1978 Sep:50(9):965-7 [PubMed PMID: 708565]
Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesthesia and analgesia. 1994 Mar:78(3):507-13 [PubMed PMID: 8109769]
Level 1 (high-level) evidenceBrown DL, Cahill DR, Bridenbaugh LD. Supraclavicular nerve block: anatomic analysis of a method to prevent pneumothorax. Anesthesia and analgesia. 1993 Mar:76(3):530-4 [PubMed PMID: 8452261]
Neal JM, Gerancher JC, Hebl JR, Ilfeld BM, McCartney CJ, Franco CD, Hogan QH. Upper extremity regional anesthesia: essentials of our current understanding, 2008. Regional anesthesia and pain medicine. 2009 Mar-Apr:34(2):134-70. doi: 10.1097/AAP.0b013e31819624eb. Epub [PubMed PMID: 19282714]
Level 3 (low-level) evidenceAbell DJ, Barrington MJ. Pneumothorax after ultrasound-guided supraclavicular block: presenting features, risk, and related training. Regional anesthesia and pain medicine. 2014 Mar-Apr:39(2):164-7. doi: 10.1097/AAP.0000000000000045. Epub [PubMed PMID: 24496168]
Level 3 (low-level) evidenceTechasuk W, González AP, Bernucci F, Cupido T, Finlayson RJ, Tran DQ. A randomized comparison between double-injection and targeted intracluster-injection ultrasound-guided supraclavicular brachial plexus block. Anesthesia and analgesia. 2014 Jun:118(6):1363-9. doi: 10.1213/ANE.0000000000000224. Epub [PubMed PMID: 24842181]
Level 1 (high-level) evidenceSoares LG, Brull R, Lai J, Chan VW. Eight ball, corner pocket: the optimal needle position for ultrasound-guided supraclavicular block. Regional anesthesia and pain medicine. 2007 Jan-Feb:32(1):94-5 [PubMed PMID: 17196502]
Level 3 (low-level) evidenceDuggan E, El Beheiry H, Perlas A, Lupu M, Nuica A, Chan VW, Brull R. Minimum effective volume of local anesthetic for ultrasound-guided supraclavicular brachial plexus block. Regional anesthesia and pain medicine. 2009 May-Jun:34(3):215-8. doi: 10.1097/AAP.0b013e31819a9542. Epub [PubMed PMID: 19587618]
Gadsden J, Gratenstein K, Hadzic A. Intraneural injection and peripheral nerve injury. International anesthesiology clinics. 2010 Fall:48(4):107-15. doi: 10.1097/AIA.0b013e3181f89b10. Epub [PubMed PMID: 20881530]
Gadsden JC, Choi JJ, Lin E, Robinson A. Opening injection pressure consistently detects needle-nerve contact during ultrasound-guided interscalene brachial plexus block. Anesthesiology. 2014 May:120(5):1246-53. doi: 10.1097/ALN.0000000000000133. Epub [PubMed PMID: 24413417]
Level 2 (mid-level) evidenceNeal JM. Ultrasound-Guided Regional Anesthesia and Patient Safety: Update of an Evidence-Based Analysis. Regional anesthesia and pain medicine. 2016 Mar-Apr:41(2):195-204. doi: 10.1097/AAP.0000000000000295. Epub [PubMed PMID: 26695877]
Honnannavar KA, Mudakanagoudar MS. Comparison between Conventional and Ultrasound-Guided Supraclavicular Brachial Plexus Block in Upper Limb Surgeries. Anesthesia, essays and researches. 2017 Apr-Jun:11(2):467-471. doi: 10.4103/aer.AER_43_17. Epub [PubMed PMID: 28663643]
Gamo K, Kuriyama K, Higuchi H, Uesugi A, Nakase T, Hamada M, Kawai H. Ultrasound-guided supraclavicular brachial plexus block in upper limb surgery: outcomes and patient satisfaction. The bone & joint journal. 2014 Jun:96-B(6):795-9. doi: 10.1302/0301-620X.96B6.31893. Epub [PubMed PMID: 24891581]
Level 2 (mid-level) evidenceBeach ML, Sites BD, Gallagher JD. Use of a nerve stimulator does not improve the efficacy of ultrasound-guided supraclavicular nerve blocks. Journal of clinical anesthesia. 2006 Dec:18(8):580-4 [PubMed PMID: 17175426]
Stav A, Reytman L, Stav MY, Portnoy I, Kantarovsky A, Galili O, Luboshitz S, Sevi R, Sternberg A. Comparison of the Supraclavicular, Infraclavicular and Axillary Approaches for Ultrasound-Guided Brachial Plexus Block for Surgical Anesthesia. Rambam Maimonides medical journal. 2016 Apr 19:7(2):. doi: 10.5041/RMMJ.10240. Epub 2016 Apr 19 [PubMed PMID: 27101216]
Guo CW, Ma JX, Ma XL, Lu B, Wang Y, Tian AX, Sun L, Wang Y, Dong BC, Teng YB. Supraclavicular block versus interscalene brachial plexus block for shoulder surgery: A meta-analysis of clinical control trials. International journal of surgery (London, England). 2017 Sep:45():85-91. doi: 10.1016/j.ijsu.2017.07.098. Epub 2017 Jul 26 [PubMed PMID: 28755885]
Level 1 (high-level) evidence