Introduction
Cordotomy is the name of a surgical procedure aimed at destroying the pain-conducting tracts of the spinal cord. First performed in 1912 by neurosurgeons William Spiller and Edward Martin, they found the cordotomy to effectively decrease temperature and pain sensations in patients who suffer from painful conditions. It was originally widely used for chronic pain, but now it has been adapted for use in patients with cancer only. The open procedure is rarely performed due to the high risk and complication rates observed previously.
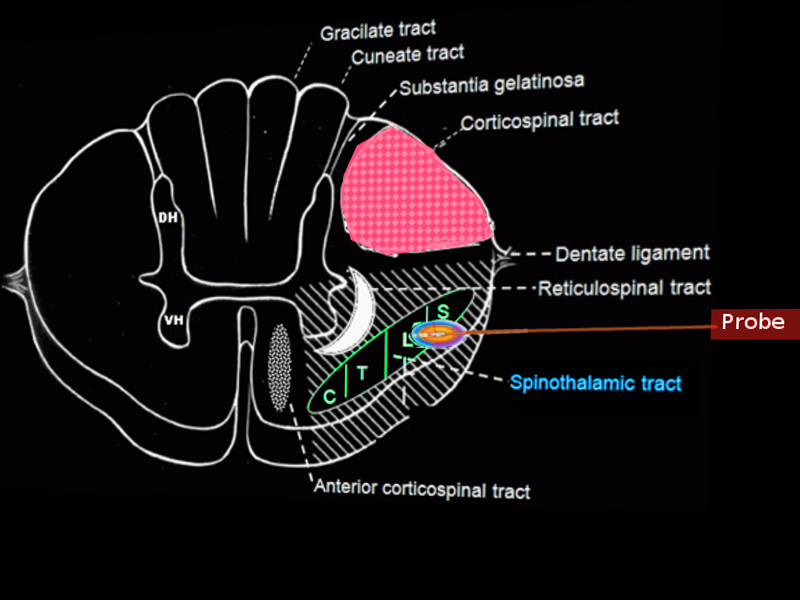
The open method underwent further adaptation to a percutaneous cervical cordotomy in 1963 (see Image. Percutaneous Cordotomy). In the 1990s, with improvements in pain management, the cordotomy again fell out of favor. However, it is still a palliative option for therapy-resistant pain. Given the population which receives this procedure, there is severely limited availability of studies testing its long-term effects. There is a case study of a patient with seminoma who underwent a right-sided percutaneous cervical cordotomy and chemotherapy. The physicians found the patient, five years later, to have continued sensory impact with minimal impact on motor and autonomic function.[1]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Today with the percutaneous cervical cordotomy, the nociceptive pathways in the lateral spinothalamic tract (in the anterolateral column) are destroyed in the cervical spinal cord at the level of C1-C2.[2]
Indications
The original approach focused on pain relief for patients with unilateral malignancies, lower extremity pathologies, failed back syndrome, chronic nociceptive painful conditions, and cancer patients. On the other hand, bilateral cordotomies for visceral or bilateral pain are also an option. In the more recent percutaneous approach, the destruction of the lateral spinothalamic tract at the level of C1-C2 results in a contralateral disruption of painful sensations beyond C4. Today, this latter approach is most commonly used in patients with limited life expectancy and suffering from opioid-resistant cancer pain. Irrespective of the procedure or technique, one uniform indication for this intervention is having severely intractable pain which has not responded to conventional therapies. Cancer-related pain is an indication but not a requirement as it can be done in populations suffering other irreversible painful conditions. The pain severity level is essential when considering appropriate indications. The patient's pain must have advanced to level 3 of the World Health Organization (WHO) pain ladder before considering this invasive procedure.
The cordotomy has been documented as particularly impactful for pain secondary to mesothelioma, Pancoast syndrome, and lung cancer.[3]
Contraindications
Percutaneous cordotomy is contraindicated in patients with a coagulation disorder, severely reduced ventilator function, and if a patient is unable to cooperate.[4] Several alternative procedures were developed in the 20th century. The commissural myelotomy was developed for bilateral pain arising from the pelvic or abdominal neoplastic disease. Likewise, the punctate or limited midline myelotomy also aimed at pelvic and abdominal visceral pain. Therefore, if patients have pain solely localized to these regions, the cordotomy can be avoided, and these newer procedures adopted. With the introduction of intrathecal pumps and spinal cord stimulators, it is prudent to steer many patients away from cordotomies.[5]
Technique or Treatment
Most cordotomies utilize the percutaneous approach at the level of C1-C2. The surgeon often uses fluoroscopic or CT guidance. Patients are usually awake for the procedure, which is performed under local anesthesia. A laminectomy is required to execute an open cordotomy. It comes with a lengthier recovery and a higher risk of side effects. However, when percutaneous cordotomy is unfeasible, especially in children, the open procedure is preferred.[6]
Complications
Only a few experience serious post-procedure side effects.[7] They include dysesthesia, urinary retention, ataxia, paresis, sympathetic dysfunction (hypotension, Horner syndrome, and bladder dysfunction), sexual sensitivity impaired or lost, and a form of sleep apnea (acquired central hypoventilation syndrome). The bulk of these complications result from the accidental division of the unintended reticulospinal tracts. Another serious complication is spontaneous new pain. New pain may be old (previously extant) pain that was previously unrecognized and now unmasked by removing prior distractions. Likewise, the new pain can be viewed as an unpreventable complication from the interruption of nociceptive pathways.
Overall, the risk of severe complications with unilateral cordotomy is low. Procedure-related mortality is reported in the range of 1%-6%, which is mainly due to respiratory dysfunction.[8] With more accurate ablation techniques, no respiratory dysfunction is rare.[9]
Clinical Significance
Percutaneous cervical cordotomy is recommended for patients with a life expectancy of fewer than six months and also meets the pain severity indications. It is a palliative procedure. Successful, immediate pain relief results in approximately three-quarters of patients.[7] However, the rate of pain relief declines to less than 50% after two years. As was noted earlier, new pain syndromes can also arise, unfortunately, and patients must be aware and be willing to accept that risk. As a depiction of efficacy and clinical significance and side effects, a study showed diminished touch perception on the left side of the body, which points to likely an anterior spinothalamic tract lesion. The nearby anterior spinocerebellar (mediating proprioception), reticulospinal (mediating autonomic outflow), and cerebrospinal (mediating voluntary movement) tracts were deemed unaffected given no signs of ataxia, autonomic issues, or motor dysfunction.[10][11]
Enhancing Healthcare Team Outcomes
The cordotomy is a palliative procedure. It is often performed on patients with a life expectancy under six months and comes with significant risks and with possible significant benefits. Obtaining a thorough history is essential, and the clinician should show empathy to the patient and their condition, whether it be a malignancy or other pathology. This decision is not to be made alone or lightly by the patient, family, or clinician. Patients must not feel rushed when having their options for intractable pain laid out before them. Furthermore, this is a surgical procedure, so interprofessional approaches to conversations must take place. Proper communication should occur between the nurse, palliative physician, the surgeon, the oncologist, and the primary physician. Each specialty should help the patient make an informed decision that the patient feels is best for their own goals of care. As always, especially in palliative care patients with often many co-morbidities, the patient's medical history and background should be clearly defined to members of the patient's healthcare team. Any deviation from thoroughness can create significant challenges and risks for the patients, their family, and their clinicians. Medical errors are to be actively avoided. If any particular nurse or clinician feels that significant palliative procedures, such as the cordotomy, are not the best choice for the patient, they should tactfully bring up their concern to the clinicians involved in that patient's care. This interprofessional approach ensures that they have a full and clear understanding of the procedure, risks, and benefits before approaching the patient with their professional opinion.[12]
Nursing, Allied Health, and Interprofessional Team Interventions
Before cordotomy can be performed, the nurse must make sure that the patient has understood the procedure and has signed a consent. While most cordotomies are done percutaneously, sometimes general anesthesia is required. Irrespective of how the procedure is done, patient monitoring is vital. Resuscitative equipment must be in the room before the procedure is started. Breathing and oxygen need to be continuously monitored. A nurse dedicated to the monitoring of the patient is vital.
Nursing, Allied Health, and Interprofessional Team Monitoring
Once cordotomy is completed, the patient's vital signs and neurological status need to be monitored. The patient may develop urinary retention that may require catheterization, apnea, and fecal incontinence. The oxygen saturation must be continually monitored until the patient is stable.
Media
References
Shepherd TM, Hoch MJ, Cohen BA, Bruno MT, Fieremans E, Rosen G, Pacione D, Mogilner AY. Palliative CT-Guided Cordotomy for Medically Intractable Pain in Patients with Cancer. AJNR. American journal of neuroradiology. 2017 Feb:38(2):387-390. doi: 10.3174/ajnr.A4981. Epub 2016 Nov 3 [PubMed PMID: 27811129]
Sharma ML, Marley K, McGlone FP, Gupta M, Marshall AG. Dissociation of Spinothalamic Modalities Following Anterolateral Cordotomy. The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques. 2018 May:45(3):354-356. doi: 10.1017/cjn.2017.290. Epub 2018 Feb 1 [PubMed PMID: 29386077]
Tinkler M, Royston R, Kendall C. Palliative care for patients with mesothelioma. British journal of hospital medicine (London, England : 2005). 2017 Apr 2:78(4):219-225. doi: 10.12968/hmed.2017.78.4.219. Epub [PubMed PMID: 28398901]
Jackson MB, Pounder D, Price C, Matthews AW, Neville E. Percutaneous cervical cordotomy for the control of pain in patients with pleural mesothelioma. Thorax. 1999 Mar:54(3):238-41 [PubMed PMID: 10325900]
Level 2 (mid-level) evidenceFontaine D, Blond S, Mertens P, Lanteri-Minet M. [Neurosurgical treatment of chronic pain]. Neuro-Chirurgie. 2015 Feb:61(1):22-9. doi: 10.1016/j.neuchi.2014.11.008. Epub 2015 Feb 10 [PubMed PMID: 25681114]
Berger A, Tellem R, Arad M, Hochberg U, Gonen T, Strauss I. [NEUROSURGICAL INTERVENTIONS FOR INTRACTABLE ONCOLOGICAL PAIN]. Harefuah. 2018 Feb:157(2):108-111 [PubMed PMID: 29484867]
Sanders M, Zuurmond W. Safety of unilateral and bilateral percutaneous cervical cordotomy in 80 terminally ill cancer patients. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1995 Jun:13(6):1509-12 [PubMed PMID: 7751899]
Blaauw G, Zuijderduijn J, Hilvering C. [Percutaneous chordotomy, a method for the treatment of unbearable pain]. Nederlands tijdschrift voor geneeskunde. 1975 Jan 11:119(2):59-63 [PubMed PMID: 1055861]
Price C, Pounder D, Jackson M, Rogers P, Neville E. Respiratory function after unilateral percutaneous cervical cordotomy. Journal of pain and symptom management. 2003 May:25(5):459-63 [PubMed PMID: 12727044]
Vedantam A, Bruera E, Hess KR, Dougherty PM, Viswanathan A. Somatotopy and Organization of Spinothalamic Tracts in the Human Cervical Spinal Cord. Neurosurgery. 2019 Jun 1:84(6):E311-E317. doi: 10.1093/neuros/nyy330. Epub [PubMed PMID: 30011044]
Stuart G, Cramond T. Role of percutaneous cervical cordotomy for pain of malignant origin. The Medical journal of Australia. 1993 May 17:158(10):667-70 [PubMed PMID: 8487684]
Level 3 (low-level) evidenceHigaki N, Yorozuya T, Nagaro T, Tsubota S, Fujii T, Fukunaga T, Moriyama M, Yoshikawa T. Usefulness of cordotomy in patients with cancer who experience bilateral pain: implications of increased pain and new pain. Neurosurgery. 2015 Mar:76(3):249-56; discussion 256; quiz 256-7. doi: 10.1227/NEU.0000000000000593. Epub [PubMed PMID: 25603110]