Introduction
Trauma is the leading cause of morbidity and mortality in patients under 35-years of age and the sixth leading cause of death worldwide. The majority of serious traumatic injuries are due to blunt trauma from motor vehicle crashes and pedestrian injuries. Falls are also an important cause, particularly in the elderly. Direct blows, assaults, and sporting injuries are also common. Non-accidental trauma is an important cause and should be suspected with certain presentations and injury patterns. Blunt impact to the body may result in a variety of injuries. Severity is related to both the mechanism of injury as well as the underlying comorbidities of the patient. Blunt impact injuries generally can be classified into four categories: contusion, abrasion, laceration, and fracture. [1][2][3]Blunt impact injuries are commonly seen in forensic autopsy practice, and appropriate interpretation of wounds is essential for accurate medicolegal testimony.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Blunt impact injuries result from direct contact of a blunt object with a body. A contusion results from the blunt impact of significant force to rupture capillaries underneath the skin surface while leaving the skin surface intact, while an abrasion results from scraping off of the superficial epidermis. Contusions and abrasions may show distinct patterns which can be used to match a specific wound to a potential weapon or implement; for example, a contusion over the forehead with multiple parallel, zig-zag lines may be matched to the sole of a shoe collected at the crime scene. A laceration results from the blunt impact of significant force to tear the skin, leaving strands of subcutaneous tissues bridging the wound. [4]Contusions and lacerations may also be present on internal organs. Blunt impact of significant force to a bone results in a fracture.
Epidemiology
Blunt impact injuries are commonly seen in living and deceased patients. The appearance of wounds depends on multiple factors, including the force, speed, length of time of impact, the surface area of contact, and elasticity of tissues impacted. A large, crushing force applied to a sizable area over several minutes will result in vast tissue damage; for example, failure of the integrity of a retaining wall at a construction site will likely cause significant blunt impact injury if the wall collapses on and traps the legs of an individual. Alternatively, a smaller force applied to a smaller area will result in less tissue damage; for example, the impact of a thrown baseball to the shoulder of an individual will likely cause minor blunt trauma.
Head trauma and exsanguination are the most common early causes of death due to blunt traumatic injury.
Pathophysiology
Blunt trauma may result in internal or external hemorrhage depending on location and mechanism. Recent contusions are typically red/purple and go through a series of color changes as they heal. In general, a red/purple contusion will be more recent than a yellow/green contusion on the same patient. Similarly, recent abrasions and lacerations are typically red/purple and heal through the process of scab formation which imparts a tan/brown, crusted appearance to the wound. Postmortem abrasions will demonstrate a more tan/yellow, parchment-paper-like appearance indicating the absence of blood flow at the time the injury occurred.[5][6] Fractures heal through the process of callus formation and bony remodeling, features which can be examined microscopically to estimate the approximate age of the fracture and time since the injury.
History and Physical
Patients presenting with acute blunt trauma should be carefully assessed to ensure serious injuries are not missed. This entails obtaining a history of mechanism, events, comorbidities, allergies, medications, and last meal. Primary, secondary, and tertiary surveys are important, with appropriate intervention and resuscitation as required.
Blunt impact injuries usually manifest immediately after impact; however, deep contusions may not be visible on the skin surface for several days after the injury occurs. Examination of adjacent or underlying subcutaneous soft tissues may aid in distinguishing between contusion, in which there will be hemorrhage due to rupture of blood vessels, and lividity, a postmortem change in which blood is contained within blood vessels. Characteristics of fractures and associated soft tissue and/or skeletal muscle injuries may aid in establishing directionality of the impact causing the wound; for example, bumper impact to a pedestrian's legs often results in comminuted fractures of the tibia and/or fibula with a triangular bone fragment pointing in the direction the vehicle was moving.
Evaluation
The Advanced Trauma Life Support course was developed by the American College of Surgeons to promote a standardized, methodical approach to the evaluation of trauma patients. [7][8]The course teaches the initial assessment of trauma patients with a focus on preparation, triage, the primary survey, resuscitation, adjuncts to primary survey and resuscitation, consideration of the need for patient transfer, secondary survey, adjuncts to post-resuscitation monitoring, and reevaluation and definitive care.
Diagnosis of various blunt impact injuries and estimation of time since the injury occurred are made by gross and microscopic examination of wounds. Recent blunt impact injuries are typically characterized by acute hemorrhage microscopically without evidence of organization or hemosiderin deposition, while older blunt impact injuries show evidence of red and white blood cell degeneration, fibroblast proliferation, and hemosiderin deposition.
Treatment / Management
Victims of blunt trauma who meet certain triage criteria have been demonstrated to have improved outcomes when managed in a trauma center. Patients with a Glasgow coma scale score greater than 13, respiratory rates less than 10/min. or greater than 29/min, or patients who need ventilatory support warrant triage to a trauma center. [9][10][11]Patients with two or more long bone fractures, crushed or pulseless extremities, amputations proximal to the ankle or wrist, pelvic fractures, paralysis, or depressed skull fractures warrant trauma center triage based on injuries. The mechanism is also important as victims of high-risk auto crashes, falls from heights, motorcycle crashes, and pedestrian accidents with significant impact should be managed in a trauma center. Elderly patients, pregnant patients, anticoagulated patients, and young children should be managed in trauma centers capable of providing specialized care.
Mortality from trauma is declining for those who survive to reach trauma centers, representing improvements in resuscitation and management. A methodical approach that adheres to evidence-based guidelines for resuscitation and treatment is critical. Many traumatic injuries will heal with supportive care alone, while some may require surgery or interventional radiology for hemorrhage control. [12][13](B2)
Differential Diagnosis
- Domestic violence
- Hemorrhagic stroke
- Hypovolemic shock
- Lower genitourinary trauma
- Penetrating abdominal trauma in emergency medicine
- Pregnancy trauma
- Upper genitourinary trauma
Pearls and Other Issues
Proper interpretation of blunt impact injuries at autopsy is essential for accurate medicolegal testimony. Patterned blunt impact injuries may aid in determining the specific type of weapon or implement used to create the wound.
Injury prevention is critical to decreasing morbidity and mortality due to traumatic injury. Campaigns promoting the use of seat-belts and motorcycle and bike helmets have proven to be effective in decreasing blunt traumatic injury.
Enhancing Healthcare Team Outcomes
The management of blunt force trauma patients is with an interprofessional team that includes a trauma surgeon, emergency department physician, nurse practitioner, anesthesiologist, internist, and specialty-trained emergency and trauma nurses. After the secondary survey is done by the team, other specialists can be consulted as appropriate. All over the U.S., hospitals now have protocols to manage blunt force trauma. The outcomes of these patients depend on their age, type of injury, other comorbidities, time to treatment and number of organs involved. While mortality rates have dropped over the past 3 decades, a significant number of trauma patients still die either at the scene or upon arrival to the trauma center.
- The clinicians should focus on completing the first and secondary survey and performing procedures.
- The emergency and trauma nurses should provide patient monitoring, assist with procedures, and providing medications and blood products.
- The pharmacist should double-check dosing and assist in evaluating any medications that may cause deterioration or drug-drug interactions.
- A clinician or nurse should coordinate with the team to provide family education during and after the recitation.
The importance of coordination and communication between members of the team will improve outcomes. [14][15] (Level V)
Media
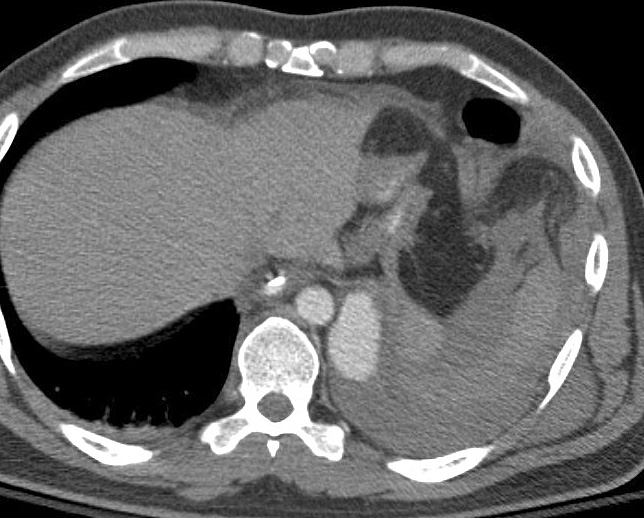
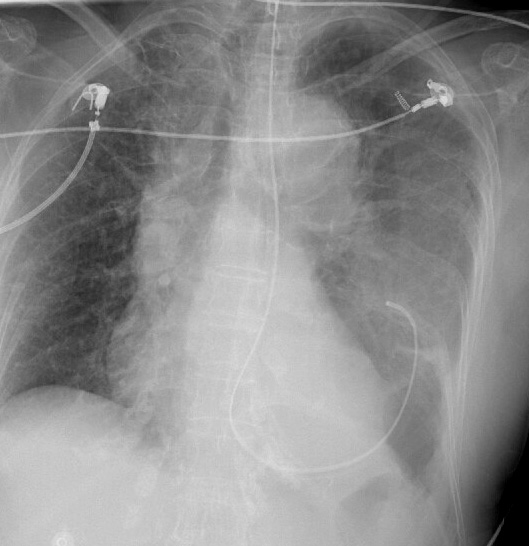
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Vester MEM, Bilo RAC, Loeve AJ, van Rijn RR, van Zandwijk JP. Modeling of inflicted head injury by shaking trauma in children: what can we learn? : Part I: A systematic review of animal models. Forensic science, medicine, and pathology. 2019 Sep:15(3):408-422. doi: 10.1007/s12024-019-0082-3. Epub 2019 Mar 4 [PubMed PMID: 30828765]
Level 3 (low-level) evidenceMorley EJ, English B, Cohen DB, Paolo WF, Nusbaum J, Gupta N. Points & Pearls: Blunt cardiac injury: emergency department diagnosis and management. Emergency medicine practice. 2019 Mar 1:21(Suppl 3):1-2 [PubMed PMID: 30821949]
Morley EJ, English B, Cohen DB, Paolo WF. Blunt cardiac injury: emergency department diagnosis and management. Emergency medicine practice. 2019 Mar:21(3):1-20 [PubMed PMID: 30794369]
Gentile S, Kneubuehl BP, Barrera V, Dobay A, Thali MJ, Bolliger SA. Fracture energy threshold in parry injuries due to sharp and blunt force. International journal of legal medicine. 2019 Sep:133(5):1429-1435. doi: 10.1007/s00414-019-02022-3. Epub 2019 Feb 21 [PubMed PMID: 30788564]
Brooks T, Choi JE, Garnich M, Hammer N, Waddell JN, Duncan W, Jermy M. Finite element models and material data for analysis of infant head impacts. Heliyon. 2018 Dec:4(12):e01010. doi: 10.1016/j.heliyon.2018.e01010. Epub 2018 Dec 8 [PubMed PMID: 30582038]
O'Toole JE, Kaiser MG, Anderson PA, Arnold PM, Chi JH, Dailey AT, Dhall SS, Eichholz KM, Harrop JS, Hoh DJ, Qureshi S, Rabb CH, Raksin PB. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on the Evaluation and Treatment of Patients with Thoracolumbar Spine Trauma: Executive Summary. Neurosurgery. 2019 Jan 1:84(1):2-6. doi: 10.1093/neuros/nyy394. Epub [PubMed PMID: 30202985]
Level 1 (high-level) evidenceSears BW, Luchette FA, Esposito TJ, Dickson EL, Grant M, Santaniello JM, Jodlowski CR, Davis KA, Poulakidas SJ, Gamelli RL. Old fashion clinical judgment in the era of protocols: is mandatory chest X-ray necessary in injured patients? The Journal of trauma. 2005 Aug:59(2):324-30; discussion 330-2 [PubMed PMID: 16294071]
Kanz KG, Sturm JA, Mutschler W. [Algorithm for prehospital blunt trauma management]. Der Unfallchirurg. 2002 Nov:105(11):1007-14 [PubMed PMID: 12402127]
Lee JK, Brady KM, Deutsch N. The Anesthesiologist's Role in Treating Abusive Head Trauma. Anesthesia and analgesia. 2016 Jun:122(6):1971-82. doi: 10.1213/ANE.0000000000001298. Epub [PubMed PMID: 27195639]
Stassen NA, Bhullar I, Cheng JD, Crandall M, Friese R, Guillamondegui O, Jawa R, Maung A, Rohs TJ Jr, Sangosanya A, Schuster K, Seamon M, Tchorz KM, Zarzuar BL, Kerwin A, Eastern Association for the Surgery of Trauma. Nonoperative management of blunt hepatic injury: an Eastern Association for the Surgery of Trauma practice management guideline. The journal of trauma and acute care surgery. 2012 Nov:73(5 Suppl 4):S288-93. doi: 10.1097/TA.0b013e318270160d. Epub [PubMed PMID: 23114483]
Schoenfeld AJ, Lehman RA Jr, Hsu JR. Evaluation and management of combat-related spinal injuries: a review based on recent experiences. The spine journal : official journal of the North American Spine Society. 2012 Sep:12(9):817-23. doi: 10.1016/j.spinee.2011.04.028. Epub 2011 Jun 2 [PubMed PMID: 21640658]
Fakhry SM, Trask AL, Waller MA, Watts DD, IRTC Neurotrauma Task Force. Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. The Journal of trauma. 2004 Mar:56(3):492-9; discussion 499-500 [PubMed PMID: 15128118]
Level 2 (mid-level) evidenceYeung LL, McDonald AA, Como JJ, Robinson B, Knight J, Person MA, Lee JK, Dahm P. Management of blunt force bladder injuries: A practice management guideline from the Eastern Association for the Surgery of Trauma. The journal of trauma and acute care surgery. 2019 Feb:86(2):326-336. doi: 10.1097/TA.0000000000002132. Epub [PubMed PMID: 30489505]
Keane M. Triad of death: the importance of temperature monitoring in trauma patients. Emergency nurse : the journal of the RCN Accident and Emergency Nursing Association. 2016 Sep:24(5):19-23. doi: 10.7748/en.2016.e1569. Epub [PubMed PMID: 27615346]
Alhelali I, Stewart TC, Foster J, Alharfi IM, Ranger A, Daoud H, Fraser DD. Basal skull fractures are associated with mortality in pediatric severe traumatic brain injury. The journal of trauma and acute care surgery. 2015 Jun:78(6):1155-61. doi: 10.1097/TA.0000000000000662. Epub [PubMed PMID: 26151517]
Demetriades D, Hadjizacharia P, Constantinou C, Brown C, Inaba K, Rhee P, Salim A. Selective nonoperative management of penetrating abdominal solid organ injuries. Annals of surgery. 2006 Oct:244(4):620-8 [PubMed PMID: 16998371]
PATCH-Trauma Investigators and the ANZICS Clinical Trials Group, Gruen RL, Mitra B, Bernard SA, McArthur CJ, Burns B, Gantner DC, Maegele M, Cameron PA, Dicker B, Forbes AB, Hurford S, Martin CA, Mazur SM, Medcalf RL, Murray LJ, Myles PS, Ng SJ, Pitt V, Rashford S, Reade MC, Swain AH, Trapani T, Young PJ. Prehospital Tranexamic Acid for Severe Trauma. The New England journal of medicine. 2023 Jul 13:389(2):127-136. doi: 10.1056/NEJMoa2215457. Epub 2023 Jun 14 [PubMed PMID: 37314244]
Subramanian M, Kaplan LJ, Cannon JW. Thromboelastography-Guided Resuscitation of the Trauma Patient. JAMA surgery. 2019 Dec 1:154(12):1152-1153. doi: 10.1001/jamasurg.2019.3136. Epub [PubMed PMID: 31596452]