Introduction
A diaphragmatic hernia is a protrusion of abdominal contents into the thoracic cavity due to a defect within the diaphragm. Diaphragmatic hernia is commonly a congenital phenomenon; however, acquired cases have also occurred.[1] The reported incidence of diaphragmatic hernia is approximately 0.8 to 5 out of 10,000 live births. Acquired diaphragmatic hernias typically occur following blunt or penetrating trauma, which results in a rupture of the diaphragm, accompanied by herniation of abdominal content; however, acquired diaphragmatic hernias can also occur spontaneously or due to iatrogenic causes.[2] Acquired diaphragmatic hernia is rare but can be life-threatening, resulting in bowel incarceration and strangulation with an overall mortality rate of up to 31%.[3]
Congenital diaphragmatic hernia is a developmental defect of the diaphragm that will result in the herniation of abdominal viscera into the chest cavity. Neonates with congenital diaphragmatic hernia usually present with respiratory distress early in the first few hours of life. The respiratory distress accompanied by the congenital diaphragmatic hernia may be mild. Occasionally, the accompanied respiratory distress is so severe and can be life-threatening. With antenatal diagnosis and improved neonatal care, survival has been remarkably improved, but a notable risk of morbidity and mortality remains in infants with congenital diaphragmatic hernia.[4]
Diaphragmatic injury is rare, complicating less than 1% of all patients with trauma.[5][6] However, the incidence includes up to 3% of all abdominal injuries.[7] Isolated diaphragmatic injuries are uncommon and are usually reported in the context of complicated abdominal and thoracic injuries. Notwithstanding the probability of an obvious herniated abdominal viscera in the thoracic cavity in the chest radiographs, the subtle cases should not be underestimated. Therefore, a high index of suspicion is strongly recommended to avoid the debilitating morbidity associated with delayed and missed diagnosis.[3][8]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The most common etiology of acquired diaphragmatic hernia is secondary to trauma, which results in diaphragmatic rupture. Acquired diaphragmatic hernia occurs more often from blunt trauma but can also result from penetrating thoracoabdominal trauma.[9] Diaphragmatic rupture from thoracoabdominal trauma occurs in approximately 0.8% to 3.6% of cases, with the incidence of herniation following such an event being relatively low.[9][10] Iatrogenic causes following surgery are the second most common cause of acquired diaphragmatic hernia; however, they are infrequent, primarily consisting of case studies in the literature. The most common surgeries with which diaphragmatic hernia has been associated and reported are following pediatric liver transplants and liver resection.[11][12]
Other documented episodes of acquired diaphragmatic hernia postsurgery within case studies include Nissen fundoplication, left colectomy, adrenalectomy, laparoscopy-assisted total gastrectomy, nephrectomy, and partial resection of the left lung using thoracoscopic surgery.[13][14][15][16][17][18][19] Spontaneous defects have also been noted; in these cases, they may be asymptomatic for years before becoming symptomatic in the later stage, where the defects can be extensive.[2] Other rare causes documented within case studies include following radio-frequency ablation for hepatocellular carcinoma and during pregnancy.[20][21][22] According to a literature review, including more than 53,000 patients with blunt and penetrating abdominal trauma, diaphragm injury was reported in up to 3 % of the cases. Moreover, the reports suggested a 2 to 1 ratio of penetrating versus blunt traumatic diaphragm injury in the studied population. The National Trauma Data Bank reported similar results (1% to 7 % vs 10% to 15 %).[7][23]
Epidemiology
Congenital diaphragmatic hernia is a severe and uncommon congenital defect occurring at a rate of 2.3 per 10,000 live births. Congenital diaphragmatic hernia primarily arises from the incomplete development of the fetal diaphragm during pregnancy, allowing abdominal organs to herniate into the thoracic cavity, leading to abnormal lung development and persistent pulmonary hypertension.[24] Acquired diaphragmatic hernia is also rare. Diaphragmatic rupture from thoracoabdominal trauma occurs in approximately 0.8% to 3.6% of cases, with the incidence of herniation following this being relatively low.[9][10]
The number of patients affected by acquired diaphragmatic hernia from other causes is not documented and is most commonly noted within case studies. Currently, no schema exists based on timing. However, most of the literature identifies an acute phase for the first 24 hours following injury and then describes patients presenting the following 24 hours as delayed. If treatment is delayed, abdominal organs can herniate through the new opening into the thoracic cavity, leading to respiratory distress and ischemia of the affected organs. Traumatic diaphragmatic rupture, when not immediately identified, can present months or even years after the initial trauma. The diagnosis is often challenging due to nonspecific clinical symptoms and radiological signs.[25]
Isolated diaphragmatic injuries are uncommon, typically occurring alongside other pathologies in 80% to 100% of cases. D’Souza et al observed intra-abdominal injuries in 77.9% of 127 cases involving penetrating diaphragmatic ruptures.[26] In one study's results, additional organ injuries were found in 86.7% of cases, with the lung being the most frequently affected extra-abdominal organ and the spleen the most common intra-abdominal organ.[27] The incidence of diaphragmatic hernia varies between blunt and penetrating traumas, with reported rates of 94% and 15.1%, respectively. Overall, diaphragmatic hernia was present in 47.26% of diaphragmatic rupture cases, with the stomach and omentum being the most frequently herniated organs.[28]
Pathophysiology
Acquired Diaphragmatic Rupture
Acquired diaphragmatic hernia due to trauma to the diaphragm is likely to occur at areas of potential weakness along embryological fusion points.[29] This condition is thought to be produced by a sudden increase in the pleuroperitoneal pressure gradient due to the trauma.[29] Multiple factors may result from iatrogenic causes depending on the type of surgery, patient-related factors, and technique used to close the diaphragm.[12] Acquired diaphragmatic hernia and diaphragmatic rupture tend to occur more commonly on the left side of the diaphragm, likely due to the right hemidiaphragm being protected by the size of the liver beneath it.[30] Right-sided ruptures and herniations are very rare and associated with higher mortality and morbidity rates.[29] The abdominal contents that can herniate into the diaphragm vary, but documented cases include herniation of the stomach, small intestine, mesentery, splenic, and pancreas.[3]
Penetrating diaphragmatic trauma
The anatomical landmarks of the diaphragm clarify the association between penetrating traumas and the potential for traumatic diaphragmatic injury. The anatomical differences during the inspiration and expiration phases should also be considered. The diaphragm rises during the expiration up to the fourth and fifth thoracic dermatome on the right and the left hemithorax, respectively. However, the diaphragm descends to as low as the eighth thoracic dermatome during the deep inspiration. The lowest level of the lateral costophrenic angle attachment is the twelfth rib. Therefore, any penetrating object that passes through the torso from T4 through T12 may injure the diaphragm. The higher rate of left traumatic diaphragmatic injury with stab wounds is presumably because of the higher prevalence of right-handed assailants.[31]
Blunt diaphragmatic trauma
Blunt diaphragmatic trauma motor vehicle collisions are responsible for most blunt diaphragmatic ruptures in almost 90% of cases. Falling and crushing injuries imply the remaining causalities of blunt diaphragmatic trauma. A significant increase in intra-abdominal pressure is required for diaphragmatic rupture in the mentioned clinical scenarios.[32] During the inspiration phase and with the diaphragmatic contraction, the diaphragm flattens. The flattened diaphragm increases the thoracic cavity's volume; accordingly, the pleuroperitoneal pressure gradient can increase from +7 to +20 cm H2O in the supine position to +100 cm H2O. The blunt force trauma to the torso can result in pleuroperitoneal gradients of up to 200 cm H2O.
The mentioned remarkable increase in pleuroperitoneal gradient surpasses the diaphragmatic tensile strength, resulting in diaphragmatic rupture or avulsion.[33] The diaphragm, a critical skeletal muscle for breathing, has a bi-domed shape with dense collagen fibers arranged diagonally from the lateral to medial direction. The diaphragm's mechanical behavior under tension is comparable to the tensile stress-strain behavior of other skeletal muscles. When at rest, the muscle fibers appear randomly oriented. However, under load, they align parallel to the direction of the tension. Initially, elastin fibers stretch linearly, but as the load increases, collagen fibers reorient to bear more load, occurring in the toe region of the stress-strain curve. With further load, the muscle experiences a transition from low to high stiffness, known as strain stiffening, where overstretched fibers eventually rupture until failure.[34] Diaphragm ruptures occur about 10 times more frequently on the left side in cases of blunt trauma, primarily because the diaphragm's left medial and posterolateral sections are less robust during embryonic development. Additionally, the liver provides a protective barrier on the right side, reducing the incidence of ruptures.[35]
Congenital Diaphragmatic Hernia
The embryologic development of the diaphragm facilitates understanding of congenital diaphragmatic hernia pathophysiology. The diaphragm originates from the following 4 main structures:
- Septum transversum: The development of the septum initiates in the fourth gestational week to separate pericardial and peritoneal cavities. Though initially located next to the cervical vertebrae, the septum transversum grows to the level of the first lumbar vertebrae. Subsequently, dorsal fusion with the esophageal mesentery and pleuroperitoneal membranes occurs.
- Esophageal mesentery: The esophageal mesentery similarly develops in the fourth gestational week and eventually forms the diaphragm's central portion and crura.
- Two paired pleuroperitoneal membranes: These develop later in the fifth week of gestation, parallel to the abdominal wall with the later medial extension. Finally, pleuroperitoneal membranes will fuse with the dorsal borders of the esophageal mesentery and septum transversum.
- Chest wall muscular structures: The complete fusion results in a discrete separation of the thoracic cavity from the abdominal cavity during the eighth gestational week.[36]
Failure of these developmental steps and incomplete fusion with adjacent structures may result in congenital diaphragmatic hernia.[37]
History and Physical
Most acquired diaphragmatic hernia cases follow either blunt or penetrating trauma to the thorax or abdomen. A clear history of trauma should prompt appropriate imaging to determine the extent of the injury, which may then demonstrate the presence of an acquired diaphragmatic hernia. For other causes of acquired diaphragmatic hernia, consideration of the patient's previous surgical history is crucial, as this may cause a diaphragmatic hernia. Patients can present with acquired diaphragmatic hernia in a variety of ways. Respiratory, abdominal, and, in some cases, cardiac symptoms are predicted.[38]
The pressure effect from the abdominal organs in the thorax can result in shortness of breath and chest pain. Abdominal symptoms may also be present, including recurrent abdominal pain, postprandial fullness, vomiting, and obstructive gastrointestinal symptoms.[29] In some spontaneous cases, the diaphragmatic hernia may remain asymptomatic, only revealed incidentally upon imaging studies. Examination of the patient may demonstrate a scaphoid abdomen, the absence of breath sounds over the lower chest on the affected side, and bowel sounds over the lower chest on the affected side.[39]
Congenital diaphragmatic hernia is characterized by a diaphragmatic muscle defect leading to a combination of global embryopathy and mechanical compression, resulting in a pathophysiologic triad of pulmonary hypertension, pulmonary hypoplasia, and cardiac dysfunction. These complex clinical challenges necessitate intensive critical care from the moment of birth. Advances in the management of congenital diaphragmatic hernia, including pressure-limited ventilation, extracorporeal life support, and neonatal critical care expertise, have significantly improved outcomes.
Additionally, a deeper understanding of the underlying pathophysiology and the development of innovative interventions are opening new therapeutic possibilities. While overall survival rates for congenital diaphragmatic hernia patients range from 65% to 80%, influenced by various factors, potential for further improvement may result through evidence-based, protocol-driven management strategies. However, congenital diaphragmatic hernia encompasses a spectrum of disease severity, and the most challenging, high-risk cases still have a survival rate of around 50%.[40] Patients may initially exhibit no symptoms following a diaphragmatic injury; however, over time, the defect can expand, potentially leading to significant herniation of abdominal organs.[41]
Evaluation
Congenital Diaphragmatic Hernia Diagnostic Studies
The diagnostic measures and required evaluations for congenital diaphragmatic hernia are classified as prenatal and postnatal congenital diaphragmatic hernia. Prenatal diagnosis in up to 60% of neonates with congenital diaphragmatic hernia is described by routine antenatal ultrasound screening during 18 to 22 weeks gestation. Nonspecific sonographic findings, including polyhydramnios or hydrops, are predicted in antenatal ultrasonography. However, the presence of abdominal organs in the fetal chest would characterize the diagnosis of congenital diaphragmatic hernia. Large diaphragmatic defects will optimize the diagnostic potential of the sonography.[42][43]
Prenatal congenital diaphragmatic hernia
Left-sided congenital diaphragmatic hernia is characterized by a heterogeneous prenatal lesion in the left hemithorax and right mediastinal shift. The heterogeneous mass implies the herniated intestines. The fluid within the mentioned mass and, more importantly, peristalsis assist in differentiating congenital diaphragmatic hernia from other prenatal intrathoracic lesions. The different diagnostic marker of congenital left-sided congenital diaphragmatic hernia is the absence of the stomach in the abdominal cavity. The displaced stomach is usually identified close to the left pericardial border or posterior cardiac space. A homogeneous hypoechoic mass in the chest close to the heart implies that Doppler sonography can further characterize the herniated liver and the intrahepatic vascular anatomy.[44]
Right-sided congenital diaphragmatic hernia is typically suggested by a homogeneous mass in the right chest on imaging studies. The herniated liver may or may not cause the left mediastinal shift. The sonographic appearance of the liver is quite similar to the lungs and, therefore, may not serve as a reliable diagnostic marker.[45] The presence of pleural fluid and intestines are other potential characteristics of the right-sided congenital diaphragmatic hernia. The cardiac left shift is a reliable marker for differentiating the right-sided congenital diaphragmatic hernia.
Postnatal congenital diaphragmatic hernia
Postnatal congenital diaphragmatic hernia should be excluded in any term infants presenting with symptoms of respiratory distress. Chest radiography indicating herniation of the abdominal organs, usually intestines characterized by air- or fluid-containing structures, into either the right or left hemithorax with minimal visible aerated lung on the affected side suggests the diagnosis of congenital diaphragmatic hernia.[46] Further evidence supporting the diagnosis of congenital diaphragmatic hernia includes the contralateral cardiac displacement, impression and mass effect over the contralateral lung, and reduced abdominal girth. The diagnosis can be confirmed by a chest radiograph demonstrating the placement of a feeding tube within the thoracic cavity or mediastinal left shift in right-sided congenital diaphragmatic hernia. Occasionally, the herniated liver is the only sign suggesting a right-sided congenital diaphragmatic hernia; in this case, a large right thoracic solid mass without the normal abdominal shadow supports the diagnosis of a right-sided congenital diaphragmatic hernia.[47]
Acquired Congenital Diaphragmatic Hernia Diagnostic Studies
Diagnosis of an acquired diaphragmatic hernia relies on imaging studies. Various imaging modalities are used to diagnose or support the diagnosis of a diaphragmatic hernia, including chest radiographs, ultrasonography, and magnetic resonance imaging, with computed tomography (CT) being the modality of choice.[39] Diagnostic confirmation with laparoscopy or thoracoscopy is recommended in patients with equivocal diagnoses. Moreover, open surgical exploration has been introduced to diagnose highly suspicious cases with equivocal imaging results. Air fluid levels in the chest demonstrate pleural effusions, which may be present in patients presenting with delayed presentation of blunt trauma due to bleeding caused by rib fractures or their subsequent injury to the lung or complications from herniated abdominal organs.[48] In the delayed presentation, the pleural effusion may be massive, resulting in a mediastinal shift to the opposite side.
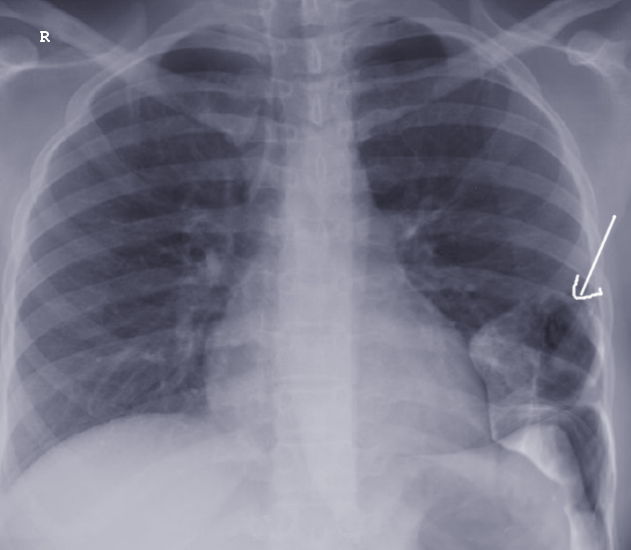
An acquired variant of traumatic diaphragmatic hernia often occurs through a contusive mechanism, resulting in diaphragmatic strains or ruptures. The symptoms of this condition are diverse and depend on factors, including the hernia's location, the size of the defect, the abdominal organs involved, the degree of organ migration, and the presence of volvulus, ischemia, or obstruction. The clinical presentation is frequently mild, and the condition is discovered incidentally, with most digestive symptoms. Severe digestive complications (eg, strangulation, volvulus, and perforation) are rare but can lead to severe shock, typically following several nonspecific digestive symptoms. Diagnosis involves imaging techniques, including plain radiography (see Image. Acquired Diaphragmatic Hernia), contrast studies, CT scans (see Image. Traumatic Diaphragmatic Hernia), and endoscopic evaluations.[49]
Treatment / Management
Treatment of acquired diaphragmatic hernia in the acute setting requires appropriate patient resuscitation followed by surgical correction.[2] Typically, the procedure will use an open abdominal approach, and primary closure will accomplish the repair.[19] In cases where primary closure with nonabsorbable sutures is not possible because of the size of the defect, then mesh repair may be an alternative.[29] If the diagnosis is delayed, a thoracic approach is generally preferred to reduce viscera-pleural adhesions and intra-thoracic visceral perforation.[29] In some delayed cases, a combined thoracic-abdominal approach may be appropriate. A laparoscopic approach may be feasible and an option for repair, depending upon experience.[19](B2)
Acquired Diaphragmatic Hernia
For treatment of acquired diaphragmatic hernias following trauma, preoperative antibiotic therapy with first-generation cephalosporins is recommended. Moreover, in patients with high suspicion of synchronized intestinal trauma, antibiotic therapy is used to cover the anaerobes. Prophylactic antibiotic therapy should be repeated in patients with greater than 1500 mL blood loss and the uncommon circumstances of prolonged surgery for 2 to 3 hours.
Following adequate primary resuscitation, a long-midline laparotomy incision from the xiphoid to the pubis is used. Primary evaluation of the 4 quadrant abdominal cavities and retroperitoneum should be undertaken. Bleeding and gastrointestinal spillage control should be prioritized. According to some literature reviews, in a selected group of patients with documented pure traumatic diaphragmatic injuries without other organ injuries, a primary upper midline incision might be performed. However, extending the incision for an appropriate exposure in equivocal circumstances after laparotomy should be considered.[50]
Next, the bulk of the trimmed diaphragmatic edges is held with Allis clamps. The edges are retracted caudally to allow adequate and versatile exposure and avoid accidental injuries to the intra-thoracic organs. Thorax should be examined entirely to ensure a bloodless, clean field. In case of contamination, copious irrigation is recommended to avoid the risk of later empyema.[51]
A thorough evaluation of the diaphragmatic surface should be included during the primary abdominal evaluation. Accordingly, the falciform ligament should be ligated and divided. Downward hepatic traction will assist in the improvement of the right hemidiaphragm evaluation. Additional exposure with mobilizing the liver from the coronary ligaments has not been described. Gastric and splenic traction should be undertaken to optimize the left hemidiaphragm visualization. The diaphragmatic central tendon and adequate firm attachments to the lumbar vertebrae should be confirmed.
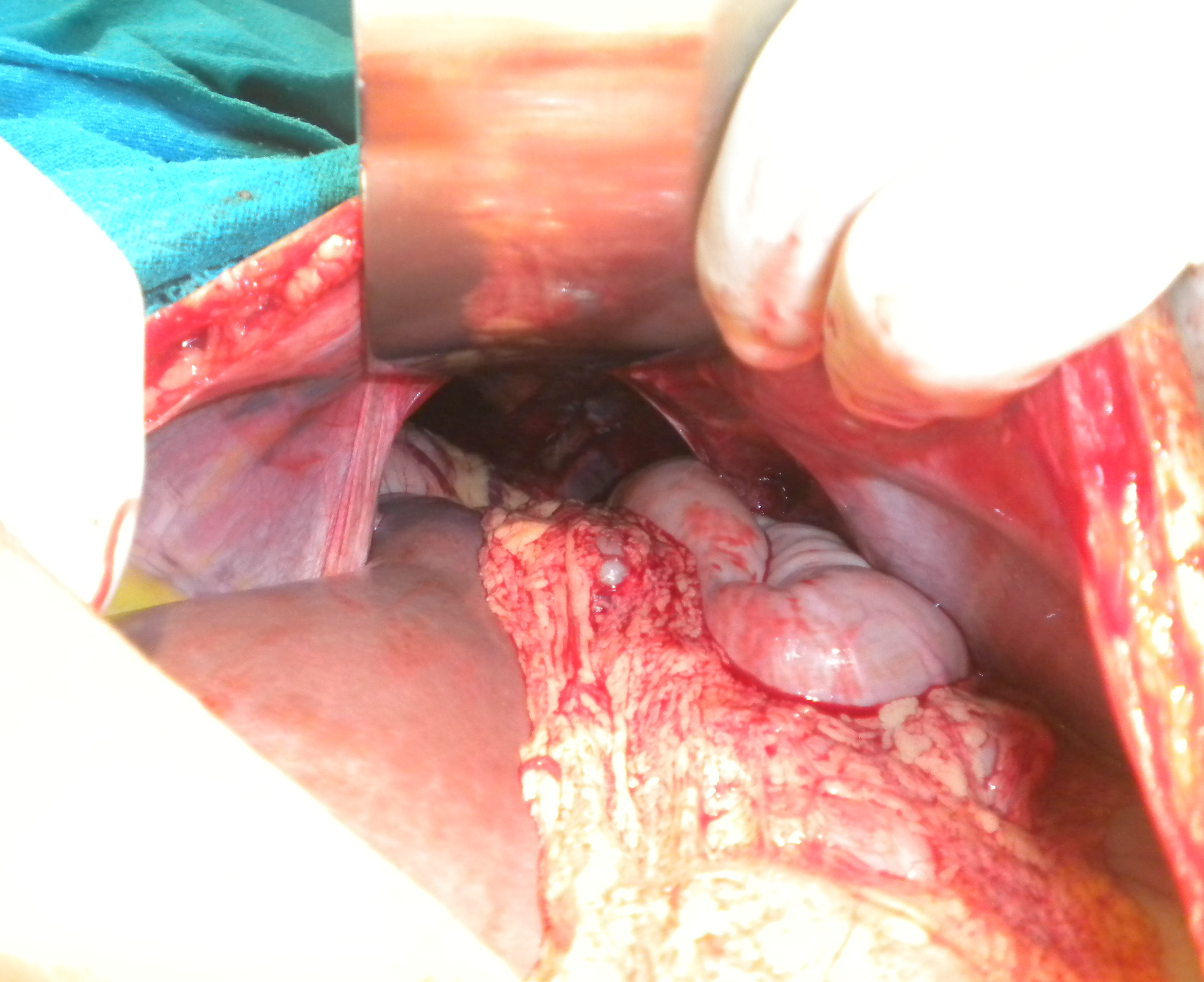
In the presence of abdominal visceral herniation, gentle reduction to the abdominal cavity should be undertaken. In rare circumstances, splenic injury during the reduction could complicate the procedure. In these selected cases, a meticulous extension of the defect is recommended. Chronic herniations differ from acute traumatic cases, where a hernia sac and severe dense adhesions are predicted. The hernia sac should be dissected, followed by the abdominal visceral reduction. Any unintentional injury, including serosal injuries, should be repaired promptly.
A transthoracic approach traditionally addresses a diaphragmatic hernia with delayed presentation (see Image. Delayed Diaphragmatic Hernia). The classic approach via a seventh or eighth intercostal thoracotomy provides excellent visualization and access to the diaphragm. This approach facilitates the identification of diaphragmatic ruptures, the release of herniated abdominal organs from potential adhesions to the lung or chest wall, and their proper reduction back into the abdomen.
Additionally, thoracotomy allows for the treatment of any obstructive complications, such as necrosis or perforation. In more complex procedures, enlarging the diaphragmatic laceration can help reduce the viscera to the abdomen.[52] The diaphragmatic repair is then undertaken with either permanent or absorbable sutures; repairs with running and interrupted fashions have been described in the literature.
For patients with an isolated diaphragmatic injury, a minimally invasive approach using laparoscopic repair should be considered. However, in patients with a positive surgical history and potential for severe dense adhesions, the left upper quadrant 3 cm below the costal margin may be preferable. Using mesh repair should not be considered the standard repair method. However, in uncommon circumstances where the primary repair is not entirely feasible considering a significant tissue loss, using a mesh might be regarded as. Nonabsorbable prosthetic materials, including polytetrafluoroethylene and polyethylene, can be applied to these patients. In gastrointestinal spillage and contamination, adequate abdominal irrigation and autologous flaps are recommended. The latter flaps are provided using either omental or latissimus dorsi flaps.[53]
Congenital Diaphragmatic Hernia
When an infant with congenital diaphragmatic hernia is delivered, a few critical steps are necessary to stabilize the child and confirm the diagnosis. In these high-risk patients with significant morbidity and mortality, following a strict delivery protocol ensures the best possible outcome. This protocol includes early recognition, a risk-stratified approach, lung-protective ventilation, and early consideration of extracorporeal life support if the patient is a suitable candidate. Study results suggest that planned delivery after 39 weeks gestation at a high-volume tertiary center, either via cesarean section or vaginal delivery, offers the best outcomes, with no difference in results based on the delivery method. After birth, initial stabilization involves measuring heart rate and pre- and post-ductal saturations. Immediate intubation is recommended for high-risk infants, though exceptions may be made for those with good predicted lung development and strong postnatal respiratory effort.[40](B3)
Extracorporeal life support is an artificial method of supporting lung or heart function, allowing recovery from reversible respiratory issues; this is used in approximately 30% of infants with congenital diaphragmatic hernia. Infants who require extracorporeal life support are considered "high risk." Factors influencing extracorporeal life support candidacy include karyotype abnormalities, syndromic features, the presence of congenital diaphragmatic hernia, left and right ventricular function and proportions, clinical status and trajectory, liver herniation, observed-to-expected lung-to-head ratio, and percent predicted lung volume.[54]
Understanding the estimated risk for infants with congenital diaphragmatic hernia both before and after birth allows families and the medical team to plan appropriately. This planning includes postnatal interventions like extracorporeal life support and, more recently, exploring antenatal interventions and novel pharmacologic treatments. Fetal lung development occurs in overlapping stages, and any disruption can hinder proper pulmonary vascular development, leading to the significant ventilation/perfusion mismatch seen in congenital diaphragmatic hernia infants. The fetoscopic endoluminal tracheal occlusion procedure involves occluding the trachea to prevent the regression of pulmonary fluid, thereby forcing the pulmonary tissue and vasculature into a hyperplastic state. This promotes the growth and expansion of the alveoli and vasculature.[55]
Differential Diagnosis
A broad range of differential diagnoses for acquired diaphragmatic hernias should be considered due to the wide range of associated clinical features. However, before imaging is performed, a diaphragmatic hernia is unlikely to be high on the differential list for causation of the patient's symptoms, except perhaps in trauma cases. After imaging, an alternative diagnosis that should merit consideration is metastasis, particularly with minor defects.[38] Congenital causes of a diaphragmatic hernia should always be a consideration, particularly when trauma has not occurred previous to the presentation.[56]
Prognosis
If the clinician misses the diagnosis of acquired diaphragmatic hernia, then there is a substantial risk of death; this can be due to lung compression with respiratory failure, vascular compromise with gastric or intestinal infarction, or perforation.[57] A variable risk in surgical mortality has been documented for diaphragmatic repair depending on concomitant injuries between 5% and 50%.[2] Generally, the outcomes following correction are good, with low recurrence levels.[2]
Research results indicate that the survival rates for isolated congenital diaphragmatic hernia (CDH) cases are higher than those accompanied by additional anomalies. Key factors influencing outcomes in CDH include (i) the presence of associated anomalies, particularly cardiac issues, (ii) the degree of lung underdevelopment, and (iii) the liver's position. Generally, the prognosis for isolated CDH is more favorable than CDH with multiple anomalies, as evidenced by population-based studies.[1]
Pulmonary hypertension is a critical factor in the pathophysiology of congenital diaphragmatic hernia, characterized by sustained, abnormally high pulmonary arterial pressures. This condition leads to dysfunction within the pulmonary circulation, impaired gas exchange, and exacerbated cardiac dysfunction. In congenital diaphragmatic hernia, pulmonary hypertension is caused by abnormal prenatal development of the pulmonary vasculature, marked by hypertrophic smooth muscle cells, vessel thickening, and reduced angiogenesis. These changes result in elevated right heart pressures, circulatory shunting, poor ventilation, and decreased oxygenation after birth.
Pulmonary hypertension is a critical element in congenital diaphragmatic hernia's pathophysiology and significantly influences disease outcomes, especially among high-risk patients. Study results have shown that 70% of infants born with congenital diaphragmatic hernia will develop pulmonary hypertension, and of these, 38% will ultimately require extracorporeal life support. This highlights the importance of pulmonary hypertension as a high-risk feature and its critical role in the management and outcomes of congenital diaphragmatic hernia.[58]
Complications
Many potential complications can result from an acquired diaphragmatic hernia. Complications reported include diaphragmatic rupture, acute obstructive symptoms, respiratory failure incarceration, strangulation, and cardiac tamponade.[57][59] Delayed diagnosis would result in irreversible complications related to prolonged herniation. Accordingly, strangulation of abdominal viscera and life-threatening intestinal obstruction, perforation, and necrosis are predictable.
Deterrence and Patient Education
Most cases of acquired diaphragmatic hernia occur in emergencies following trauma; in these situations, surgery is life-saving. If possible, consent for surgery should be obtained with an explanation of the potential complications. These should be balanced with the complications, including death if the surgery is not performed.
Enhancing Healthcare Team Outcomes
Acquired diaphragmatic hernia is a critical condition requiring urgent surgical intervention, and patient-centered care and optimal outcomes in its management depend heavily on an interprofessional approach. Given the importance of timely and accurate diagnosis, imaging expertise is vital, though it often proves challenging, particularly in patients with concurrent trauma. Effective communication and collaboration between radiologists and surgeons are essential in overcoming diagnostic hurdles, enabling surgeons to make well-informed decisions regarding the surgical approach. General surgeons typically manage these cases, but delayed diagnosis can require cardiothoracic surgical expertise, making interprofessional communication essential. Due to the rarity of acquired diaphragmatic hernias, case studies and shared surgical experiences play a crucial role in guiding complex management decisions.
In cases involving neonates with high-risk congenital diaphragmatic hernias, interprofessional teams must engage in comprehensive prenatal imaging and risk stratification to provide families with clear and informed counseling. These neonates often face unpredictable clinical courses and elevated morbidity, necessitating coordinated care goals that adapt as the patient's needs evolve. To meet these demands, clinicians, nurses, pharmacists, and other healthcare professionals collaborate continuously, working together to ensure safety and patient-centered care. Such coordinated, team-based management is critical for optimizing outcomes, maintaining patient safety, and improving overall team performance in acquired and congenital diaphragmatic hernia cases.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Chandrasekharan PK, Rawat M, Madappa R, Rothstein DH, Lakshminrusimha S. Congenital Diaphragmatic hernia - a review. Maternal health, neonatology and perinatology. 2017:3():6. doi: 10.1186/s40748-017-0045-1. Epub 2017 Mar 11 [PubMed PMID: 28331629]
Katukuri GR, Madireddi J, Agarwal S, Kareem H, Devasia T. Delayed Diagnosis of Left-Sided Diaphragmatic Hernia in an Elderly Adult with no History of Trauma. Journal of clinical and diagnostic research : JCDR. 2016 Apr:10(4):PD04-5. doi: 10.7860/JCDR/2016/17506.7544. Epub 2016 Apr 1 [PubMed PMID: 27190882]
Lu J, Wang B, Che X, Li X, Qiu G, He S, Fan L. Delayed traumatic diaphragmatic hernia: A case-series report and literature review. Medicine. 2016 Aug:95(32):e4362. doi: 10.1097/MD.0000000000004362. Epub [PubMed PMID: 27512848]
Level 2 (mid-level) evidenceDíaz Candelas DA, de la Plaza Llamas R, Arteaga Peralta V, Ramia JM. Complicated diaphragmatic hernia. Cirugia espanola. 2020 Apr:98(4):238. doi: 10.1016/j.ciresp.2019.04.016. Epub 2019 Jun 1 [PubMed PMID: 31164215]
Simon LV, Lopez RA, Burns B. Diaphragm Rupture. StatPearls. 2025 Jan:(): [PubMed PMID: 29262087]
Bocchini G, Guida F, Sica G, Codella U, Scaglione M. Diaphragmatic injuries after blunt trauma: are they still a challenge? Reviewing CT findings and integrated imaging. Emergency radiology. 2012 Jun:19(3):225-35. doi: 10.1007/s10140-012-1025-4. Epub 2012 Feb 24 [PubMed PMID: 22362421]
Petrone P, Asensio JA, Marini CP. Diaphragmatic injuries and post-traumatic diaphragmatic hernias. Current problems in surgery. 2017 Jan:54(1):11-32. doi: 10.1067/j.cpsurg.2016.11.001. Epub 2016 Nov 29 [PubMed PMID: 28212818]
Giuffrida M, Perrone G, Abu-Zidan F, Agnoletti V, Ansaloni L, Baiocchi GL, Bendinelli C, Biffl WL, Bonavina L, Bravi F, Carcoforo P, Ceresoli M, Chichom-Mefire A, Coccolini F, Coimbra R, de'Angelis N, de Moya M, De Simone B, Di Saverio S, Fraga GP, Galante J, Ivatury R, Kashuk J, Kelly MD, Kirkpatrick AW, Kluger Y, Koike K, Leppaniemi A, Maier RV, Moore EE, Peitzmann A, Sakakushev B, Sartelli M, Sugrue M, Tian BWCA, Broek RT, Vallicelli C, Wani I, Weber DG, Docimo G, Catena F. Management of complicated diaphragmatic hernia in the acute setting: a WSES position paper. World journal of emergency surgery : WJES. 2023 Jul 26:18(1):43. doi: 10.1186/s13017-023-00510-x. Epub 2023 Jul 26 [PubMed PMID: 37496073]
Pancholi CK, Hombalkar NN, Dalvi SB, Gurav PD. Left Sided Hydro-pneumothorax in a Operated Case of Left Diaphragmatic Hernia Repair: A Diagnostic Dilemma. Journal of clinical and diagnostic research : JCDR. 2015 Apr:9(4):PD03-4. doi: 10.7860/JCDR/2015/11879.5759. Epub 2015 Apr 1 [PubMed PMID: 26023591]
Level 3 (low-level) evidenceKozak O, Mentes O, Harlak A, Yigit T, Kilbas Z, Aslan I, Akin M, Bozlar U. Late presentation of blunt right diaphragmatic rupture (hepatic hernia). The American journal of emergency medicine. 2008 Jun:26(5):638.e3-5. doi: 10.1016/j.ajem.2007.10.032. Epub [PubMed PMID: 18534320]
Level 3 (low-level) evidenceEsposito F, Lim C, Salloum C, Osseis M, Lahat E, Compagnon P, Azoulay D. Diaphragmatic hernia following liver resection: case series and review of the literature. Annals of hepato-biliary-pancreatic surgery. 2017 Aug:21(3):114-121. doi: 10.14701/ahbps.2017.21.3.114. Epub 2017 Aug 31 [PubMed PMID: 28989997]
Level 2 (mid-level) evidenceCortes M, Tapuria N, Khorsandi SE, Ibars EP, Vilca-Melendez H, Rela M, Heaton ND. Diaphragmatic hernia after liver transplantation in children: case series and review of the literature. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2014 Dec:20(12):1429-35. doi: 10.1002/lt.23977. Epub 2014 Nov 5 [PubMed PMID: 25124299]
Level 3 (low-level) evidenceSommese K, Kelley K, Tan B, Fontana M, Brooks J. Iatrogenic Incarcerated Diaphragmatic Hernia after Nissen Fundoplication. The American surgeon. 2018 Jul 1:84(7):1195-1196 [PubMed PMID: 30064587]
Blount AL, Craft RO, Harold KL, Roberts CC. Laparoscopic Repair of a Chronic Iatrogenic Diaphragmatic Hernia. Radiology case reports. 2009:4(3):304. doi: 10.2484/rcr.v4i3.304. Epub 2015 Dec 7 [PubMed PMID: 27307823]
Level 3 (low-level) evidenceDell'Abate P, Bertocchi E, Dalla Valle R, Viani L, Del Rio P, Sianesi M. Iatrogenic diaphragmatic hernia following laparoscopic left colectomy for splenic flexure cancer An unusual complication. Annali italiani di chirurgia. 2016 Nov 3:87():. pii: S2239253X16025937. Epub 2016 Nov 3 [PubMed PMID: 28232645]
Vilallonga R, Caubet E, González O, Neff KJ, Fort JM, Mazarro A, Armengol M. Laparoscopic repair of a postadrenalectomy left-sided diaphragmatic hernia complicated by chronic colon obstruction. Surgical endoscopy. 2013 May:27(5):1826-8. doi: 10.1007/s00464-012-2641-5. Epub 2012 Dec 12 [PubMed PMID: 23233014]
Level 3 (low-level) evidenceSuh Y, Lee JH, Jeon H, Kim D, Kim W. Late onset iatrogenic diaphragmatic hernia after laparoscopy-assisted total gastrectomy for gastric cancer. Journal of gastric cancer. 2012 Mar:12(1):49-52. doi: 10.5230/jgc.2012.12.1.49. Epub 2012 Mar 30 [PubMed PMID: 22500265]
Level 3 (low-level) evidenceFukami T, Konoeda C, Kitano K, Sakamoto M, Sano A, Yoshida Y, Mura T, Nakajima J. [Iatrogenic diaphragmatic hernia following partial resection of the lung via video-assisted thoracoscopy]. Kyobu geka. The Japanese journal of thoracic surgery. 2010 Dec:63(13):1151-4 [PubMed PMID: 21174666]
Level 3 (low-level) evidenceMínguez Ruiz G, García Florez LJ, Arias Pacheco RD, García Bear I, Ramos Pérez V, Pire Abaitua G. Post-nephrectomy diaphragmatic hernia. Increase suspicion and decrease morbi-mortality: two cases report. Journal of surgical case reports. 2018 Aug:2018(8):rjy224. doi: 10.1093/jscr/rjy224. Epub 2018 Aug 20 [PubMed PMID: 30151114]
Level 3 (low-level) evidenceSingh M, Singh G, Pandey A, Cha CH, Kulkarni S. Laparoscopic repair of iatrogenic diaphragmatic hernia following radiofrequency ablation for hepatocellular carcinoma. Hepatology research : the official journal of the Japan Society of Hepatology. 2011 Nov:41(11):1132-6. doi: 10.1111/j.1872-034X.2011.00865.x. Epub [PubMed PMID: 22032681]
Sano A, Kato H, Hamatani H, Sakai M, Tanaka N, Inose T, Kimura H, Kuwano H. Diaphragmatic hernia with ischemic bowel obstruction in pregnancy: report of a case. Surgery today. 2008:38(9):836-40. doi: 10.1007/s00595-007-3718-y. Epub 2008 Aug 28 [PubMed PMID: 18751950]
Level 3 (low-level) evidenceJacobs R, Honore PM, Hosseinpour N, Nieboer K, Spapen HD. Sudden cardiac arrest during pregnancy: a rare complication of acquired maternal diaphragmatic hernia. Acta clinica Belgica. 2012 May-Jun:67(3):198-200 [PubMed PMID: 22897068]
Level 3 (low-level) evidenceFair KA, Gordon NT, Barbosa RR, Rowell SE, Watters JM, Schreiber MA. Traumatic diaphragmatic injury in the American College of Surgeons National Trauma Data Bank: a new examination of a rare diagnosis. American journal of surgery. 2015 May:209(5):864-8; discussion 868-9. doi: 10.1016/j.amjsurg.2014.12.023. Epub 2015 Feb 21 [PubMed PMID: 25952278]
Feng Z, Wei Y, Wang Y, Liu C, Qu D, Li J, Ma L, Niu W. Development of a prediction nomogram for 1-month mortality in neonates with congenital diaphragmatic hernia. BMC surgery. 2024 Jun 27:24(1):198. doi: 10.1186/s12893-024-02479-z. Epub 2024 Jun 27 [PubMed PMID: 38937726]
Zhao L, Han Z, Liu H, Zhang Z, Li S. Delayed traumatic diaphragmatic rupture: diagnosis and surgical treatment. Journal of thoracic disease. 2019 Jul:11(7):2774-2777. doi: 10.21037/jtd.2019.07.14. Epub [PubMed PMID: 31463105]
D'Souza N, Clarke D, Laing G. Prevalence, management and outcome of traumatic diaphragm injuries managed by the Pietermaritzburg Metropolitan Trauma Service. Annals of the Royal College of Surgeons of England. 2017 May:99(5):394-401. doi: 10.1308/rcsann.2017.0029. Epub [PubMed PMID: 28462659]
Taş İ, Yiğit E. Analysis of traumatic acute diaphragmatic injuries. Singapore medical journal. 2023 Sep 25:():. doi: 10.4103/singaporemedj.SMJ-2022-076. Epub 2023 Sep 25 [PubMed PMID: 37870035]
Gao JM, Du DY, Li H, Liu CP, Liang SY, Xiao Q, Zhao SH, Yang J, Lin X. Traumatic diaphragmatic rupture with combined thoracoabdominal injuries: Difference between penetrating and blunt injuries. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2015:18(1):21-6 [PubMed PMID: 26169090]
Testini M, Girardi A, Isernia RM, De Palma A, Catalano G, Pezzolla A, Gurrado A. Emergency surgery due to diaphragmatic hernia: case series and review. World journal of emergency surgery : WJES. 2017:12():23. doi: 10.1186/s13017-017-0134-5. Epub 2017 May 18 [PubMed PMID: 28529538]
Level 2 (mid-level) evidenceLodhia JV, Appiah S, Tcherveniakov P, Krysiak P. Diaphragmatic hernia masquerading as a pulmonary metastasis. Annals of the Royal College of Surgeons of England. 2015 Mar:97(2):e27-9. doi: 10.1308/003588414X14055925060758. Epub [PubMed PMID: 25723679]
Level 3 (low-level) evidenceNason LK, Walker CM, McNeeley MF, Burivong W, Fligner CL, Godwin JD. Imaging of the diaphragm: anatomy and function. Radiographics : a review publication of the Radiological Society of North America, Inc. 2012 Mar-Apr:32(2):E51-70. doi: 10.1148/rg.322115127. Epub [PubMed PMID: 22411950]
Beshay M, Mertzlufft F, Kottkamp HW, Reymond M, Schmid RA, Branscheid D, Vordemvenne T. Analysis of risk factors in thoracic trauma patients with a comparison of a modern trauma centre: a mono-centre study. World journal of emergency surgery : WJES. 2020 Jul 31:15(1):45. doi: 10.1186/s13017-020-00324-1. Epub 2020 Jul 31 [PubMed PMID: 32736642]
Sekusky AL, Lopez RA. Diaphragm Trauma. StatPearls. 2024 Jan:(): [PubMed PMID: 32491579]
Gaur P, Chawla A, Verma K, Mukherjee S, Lalvani S, Malhotra R, Mayer C. Characterisation of human diaphragm at high strain rate loading. Journal of the mechanical behavior of biomedical materials. 2016 Jul:60():603-616. doi: 10.1016/j.jmbbm.2016.02.031. Epub 2016 Mar 17 [PubMed PMID: 27062242]
Tokgöz S, Akkoca M, Uçar Y, Yilmaz KB, Sevim Ö, Gündoğan G. Factors affecting mortality in traumatic diaphragm ruptures. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2019 Nov:25(6):567-574. doi: 10.14744/tjtes.2019.58133. Epub [PubMed PMID: 31701506]
Bains KNS, Kashyap S, Lappin SL. Anatomy, Thorax, Diaphragm. StatPearls. 2025 Jan:(): [PubMed PMID: 30137842]
Chatterjee D, Ing RJ, Gien J. Update on Congenital Diaphragmatic Hernia. Anesthesia and analgesia. 2020 Sep:131(3):808-821. doi: 10.1213/ANE.0000000000004324. Epub [PubMed PMID: 31335403]
Tibrewala NS, Pai PM. Congenital malformations in the newborn period. Indian pediatrics. 1974 Jun:11(6):403-7 [PubMed PMID: 4473425]
Panda A, Kumar A, Gamanagatti S, Patil A, Kumar S, Gupta A. Traumatic diaphragmatic injury: a review of CT signs and the difference between blunt and penetrating injury. Diagnostic and interventional radiology (Ankara, Turkey). 2014 Mar-Apr:20(2):121-8. doi: 10.5152/dir.2013.13248. Epub [PubMed PMID: 24412818]
Level 2 (mid-level) evidenceHolden KI, Harting MT. Recent advances in the treatment of complex congenital diaphragmatic hernia-a narrative review. Translational pediatrics. 2023 Jul 31:12(7):1403-1415. doi: 10.21037/tp-23-240. Epub 2023 Jul 6 [PubMed PMID: 37575897]
Level 3 (low-level) evidenceKaur R, Prabhakar A, Kochhar S, Dalal U. Blunt traumatic diaphragmatic hernia: Pictorial review of CT signs. The Indian journal of radiology & imaging. 2015 Jul-Sep:25(3):226-32. doi: 10.4103/0971-3026.161433. Epub [PubMed PMID: 26288515]
Zahid A, Nawaz FA, Duvuru R, Alabrach YS, Ahmed A. Congenital Diaphragmatic Hernia With Kidney and Spleen Herniation in the United Arab Emirates: A Case Report. Cureus. 2022 Jul:14(7):e26732. doi: 10.7759/cureus.26732. Epub 2022 Jul 11 [PubMed PMID: 35967164]
Level 3 (low-level) evidenceMbaye PA, Gueye D, Fall M, Zeng FTA, Seye C, Seck NF, Cissé L, Ndoye NA, Sagna A, Ngom G. [Management of congenital diaphragmatic hernia in sub-Saharan Africa: experience in the Albert Royer National Children's Hospital Center, Senegal]. The Pan African medical journal. 2022:41():185. doi: 10.11604/pamj.2022.41.185.30907. Epub 2022 Mar 8 [PubMed PMID: 35655674]
Pelizzo G, Finazzo F, Vitaliti MS, Bellieni CV, Calcaterra V. Left-sided congenital diaphragmatic hernia and liver-up: time to revise simplistic views? The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2021 Dec:34(23):4005-4007. doi: 10.1080/14767058.2019.1702948. Epub 2019 Dec 25 [PubMed PMID: 31875733]
Iqbal CW, Derderian SC, Lusk L, Basta A, Filly RA, Lee H, Hirose S. Outcomes for Prenatally Diagnosed Right Congenital Diaphragmatic Hernia. Fetal diagnosis and therapy. 2020:47(1):1-6. doi: 10.1159/000369385. Epub 2015 Mar 4 [PubMed PMID: 25765922]
Level 2 (mid-level) evidenceAprahamian A, Nouyrigat V, Grévent D, Hervieux E, Chéron G. [Postnatal diagnosis of gastric volvulus revealing congenital diaphragmatic hernia]. Archives de pediatrie : organe officiel de la Societe francaise de pediatrie. 2017 May:24(5):464-467. doi: 10.1016/j.arcped.2017.02.028. Epub 2017 Mar 21 [PubMed PMID: 28336004]
Chang PT, Taylor GA. Umbilical venous catheter malposition and errors in interpretation in newborns with Bochdalek hernia. Pediatric radiology. 2015 Jul:45(7):982-8. doi: 10.1007/s00247-014-3275-7. Epub 2015 Feb 10 [PubMed PMID: 25875634]
Wu YS, Lin YY, Hsu CW, Chu SJ, Tsai SH. Massive ipsilateral pleural effusion caused by transdiaphragmatic intercostal hernia. The American journal of emergency medicine. 2008 Feb:26(2):252.e3-4. doi: 10.1016/j.ajem.2007.04.018. Epub [PubMed PMID: 18272132]
Predescu D, Achim F, Socea B, Ceaușu MC, Constantin A. Rare Diaphragmatic Hernias in Adults-Experience of a Tertiary Center in Esophageal Surgery and Narrative Review of the Literature. Diagnostics (Basel, Switzerland). 2023 Dec 29:14(1):. doi: 10.3390/diagnostics14010085. Epub 2023 Dec 29 [PubMed PMID: 38201394]
Level 3 (low-level) evidenceLynch T, Kilgar J, Al Shibli A. Pediatric Abdominal Trauma. Current pediatric reviews. 2018:14(1):59-63. doi: 10.2174/1573396313666170815100547. Epub [PubMed PMID: 28814248]
Şentürk M, Çakır M, Ali Akbulut M, Yeşildağ K. Approach to Traumatic Diaphragm Injuries: Single Center Experience. Journal of acute medicine. 2021 Mar 1:11(1):18-21. doi: 10.6705/j.jacme.202103_11(1).0003. Epub [PubMed PMID: 33928012]
Filosso PL, Guerrera F, Sandri A, Lausi PO, Lyberis P, Bora G, Roffinella M, Ruffini E. Surgical management of chronic diaphragmatic hernias. Journal of thoracic disease. 2019 Feb:11(Suppl 2):S177-S185. doi: 10.21037/jtd.2019.01.54. Epub [PubMed PMID: 30906583]
Abboud NM, Rimbault M, Abboud S, El Nakadi I, Charara FG. A Surgical Alternative in the Treatment of Recurrent Diaphragmatic Hernia after Total Gastrectomy. Plastic and reconstructive surgery. Global open. 2020 Dec:8(12):e3302. doi: 10.1097/GOX.0000000000003302. Epub 2020 Dec 21 [PubMed PMID: 33425611]
Yu PT, Jen HC, Rice-Townsend S, Guner YS. The role of ECMO in the management of congenital diaphragmatic hernia. Seminars in perinatology. 2020 Feb:44(1):151166. doi: 10.1053/j.semperi.2019.07.005. Epub 2019 Jul 30 [PubMed PMID: 31472951]
Tsao K, Johnson A. Fetal tracheal occlusion for congenital diaphragmatic hernia. Seminars in perinatology. 2020 Feb:44(1):151164. doi: 10.1053/j.semperi.2019.07.003. Epub 2019 Jul 30 [PubMed PMID: 31451196]
Reddy M, Kroushev A, Palmer K. Undiagnosed maternal diaphragmatic hernia - a management dilemma. BMC pregnancy and childbirth. 2018 Jun 15:18(1):237. doi: 10.1186/s12884-018-1864-4. Epub 2018 Jun 15 [PubMed PMID: 29907140]
Thompson M, Wills S, Byard RW. Forensic Features of Lethal Late-Presenting Diaphragmatic Hernias. Journal of forensic sciences. 2016 Sep:61(5):1261-5. doi: 10.1111/1556-4029.13142. Epub 2016 Jun 22 [PubMed PMID: 27329694]
Gupta VS, Harting MT. Congenital diaphragmatic hernia-associated pulmonary hypertension. Seminars in perinatology. 2020 Feb:44(1):151167. doi: 10.1053/j.semperi.2019.07.006. Epub 2019 Jul 30 [PubMed PMID: 31519366]
D'Orio V, Demondion P, Lebreton G, Coutance G, Varnous S, Leprince P. Acquired transdiaphragmatic hernia: an unusual cause of cardiac tamponade. Asian cardiovascular & thoracic annals. 2017 Mar:25(3):233-236. doi: 10.1177/0218492317698326. Epub 2017 Jan 1 [PubMed PMID: 28325075]