Introduction
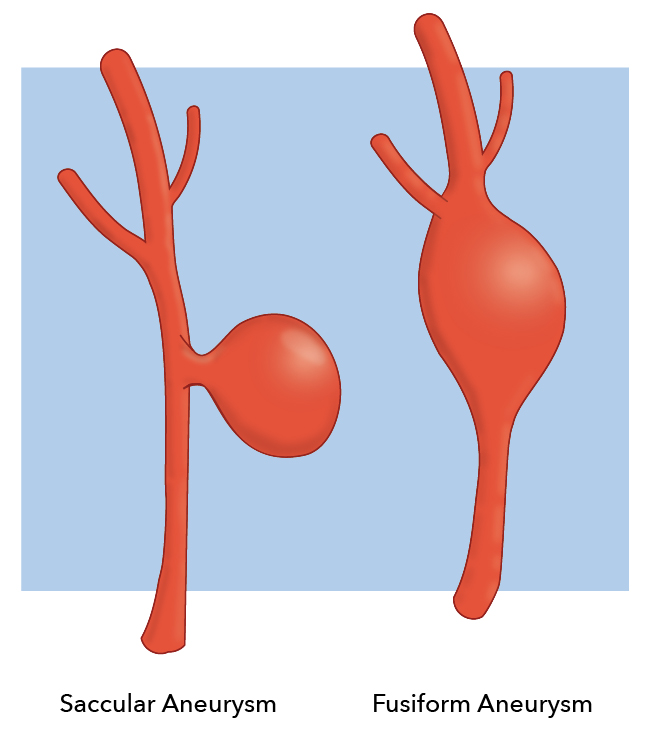
Berry (saccular) aneurysms are the most common type of intracranial aneurysm, representing 90% of cerebral aneurysms. Generally speaking, ballooning arises from a weakened area in the wall of a blood vessel in the brain. Depending on the size of the aneurysm, their symptomatology ranges from asymptomatic to intracerebral hemorrhage (subarachnoid) in the most extreme cases. Berry aneurysm is an older terminology that has mostly been replaced by saccular aneurysm (see Image. Berry Aneurysm). The new nomenclature goes against the tradition of likening a pathologic process to various fruit products. Aneurysm is from the Greek word aneurysma, meaning dilation.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Genetic Factors
- Connective tissue disorders that weaken artery walls
- Polycystic kidney disease
- Arteriovenous malformations
- History of an aneurysm in 2 or more first degree family members
Other Factors
- Untreated high blood pressure
- Cigarette smoking
- Drug abuse, including cocaine and amphetamines, which, via their toxidrome, increases blood pressure extremely. Intravenous drug abuse can cause infectious mycotic aneurysms.
- Heavy alcohol intake
- Heavy caffeine intake
Less Common
- Head trauma
- Infection in the arterial wall from bacteremia - mycotic aneurysms
Risk Factors for Aneurysm Rupture
- Smoking: Not only can smoking promote the development of cerebral aneurysms, but it can also lead to their growth and rupture.
- High blood pressure: Chronic damage to arteries leads to weakness, forming an aneurysm and making them more likely to rupture.
- Size: Larger aneurysms rupture with greater frequency than small ones.
- Location: Posterior circulation, including posterior communicating artery (PCOM), posterior cerebral artery (PCA), and vertebrobasilar artery, are more common
- Growth: If aneurysms grow during a surveillance period despite being small, they are at an increased risk of rupture.
- Family history: If there is a family history, there is a higher risk of rupture.
- Irregular shape, multilobed, daughter sac, blebs
Those with previous ruptures or intracranial bleeds are at the highest risk of cerebral artery aneurysm rupture.[1]
Epidemiology
- Cerebral aneurysms occur in 3 to 5 percent of the general population.
- The prevalence is 3.2 percent by radiographic and autopsy series.[2]
- 0.7 to 1.9 percent rupture, causing subarachnoid hemorrhage (SAH)[3]
- The mean age is 50 years.
- More common in females
- Twenty to thirty percent of patients with aneurysms have multiple aneurysms.
- Eighty-five percent of aneurysms are located in the anterior circulation, mostly in the circle of Willis.
Common Sites in the Anterior Circulation
- Junction of the anterior communicating artery with the anterior cerebral artery
- Junction of the posterior communicating artery with the internal carotid artery
- Bifurcation of the middle cerebral artery
Common Sites in the Posterior Circulation
- Top of the basilar artery, called the basilar apex
- Junction of the basilar artery and the superior or anterior inferior cerebellar arteries
- Junction of the vertebral artery and the posterior inferior cerebellar artery[4]
Pathophysiology
Berry aneurysms are due to outpouchings in the blood vessel wall, which can be hereditary factors or acquired disease. Repetitive trauma and shearing forces against the weak point in the blood vessel’s wall cause aneurysms to enlarge.[5]
Older dogma considers berry aneurysms to be passively enlarging vascular structures. More recent evidence suggests that berry aneurysms, along with other forms of aneurysms, are created and enlarged through continuous inflammation and tissue degradation.
Histopathology
Some traditional classifications pose this as a model for organizing the types of intracranial aneurysms:
- Mycotic: An artery having sustained damage secondary to an infectious process. these aneurysms tend to be located more distally
- Luetic: Also called syphilitic aneurysms, usually in the aorta and known as syphilitic aortitis, seen in the tertiary stage of syphilis
- Arteriosclerotic: These vessel widenings (aneurysms) occur due to arteriosclerosis damaging the vessel wall [6]
- Traumatic: Vessels may be damaged or disrupted in the setting of trauma, both penetrating to the head and blunt injuries - these are commonly pseudoaneurysms
- These types of aneurysms represent less than 1% of cerebral aneurysms. However, they are prone to grow rapidly, leading to increased morbidity and mortality. Vigilance should be implemented to detect and treat these in the trauma setting.
- Congenital: Certain conditions predispose people to be born with aneurysms. One example is ADPKD (autosomal dominant polycystic kidney disease).[7]
History and Physical
The clinical picture of berry aneurysms includes the most severe manifestation of a major aneurysmal rupture, such as a subarachnoid hemorrhage to minor hemorrhage, also known as a sentinel bleed, nonhemorrhagic scenarios, or asymptomatic situations in which the aneurysm is found incidentally.[8]
Many of these patients may be brought in in extremis, so ABCs take priority. Assess the patient's airway and breathing and establish good IV access. In the trauma setting, give priority to your primary survey, and do not forget to do a thorough secondary survey. Do not be distracted by dramatic extremity injuries. Once the patient has been stabilized hemodynamically, give priority to emergent neuroimaging.
Other patients may present less extreme and warrant a thorough history and physical, even outside the setting of trauma.
Your History should include some key elements as described below:
- Headache - WHOML (worst headache of my life), thunderclap headache. The headache need not be the worst of the patient's life. Even a headache that is different from past headaches should raise one's suspicion of subarachnoid hemorrhage.
- Change in level of consciousness: Increased intracranial pressure decreases the perfusion pressures required to oxygenate the brain properly. Patients may appear confused or less alert than expected.
- Seizures present in 25% of aneurysmal subarachnoid hemorrhage. They may be focal or generalized.
- Meningeal signs - Patients may have classic meningeal irritation and complain of neck pain or stiffness.
- Focal neurologic deficits include changes in strength, sensation, ability to speak or express themselves, and memory loss.
- Visual symptoms- blurry vision, double vision (diplopia), defects in the patient's visual field
The physical exam should include and not be limited to the following elements:
- A complete neurologic exam:
- Cranial nerve testing
- Strength of upper and lower extremities and face
- Sensations of upper and lower extremities and face
- Assess speech (dysarthric, disorganized, comprehensible)
- Assess for meningismus, Kernig's and Brudzinski's signs
- HEENT
- Examine for signs of trauma to the head
- obvious signs of injury, including lacerations, abrasions, contusions, skull depressions/fractures
- Ears - look for blood behind the tympanic membrane (hemotympanum), assess for CSF otorrhea
- Eyes - ensure PERRLA (pupils equal round and reactive to light and accommodation)
- look for other signs of eye trauma (iritis, conjunctival hemorrhage, globe rupture), which may indicate a severe mechanism of injury
- Nose - assess for nasal fractures, CSF rhinorrhea[9]
- Examine for signs of trauma to the head
Evaluation
Imaging
- NCCT (non-contrast CT) of the head[10]
- With or without CT angiography of the head, especially if NCCT is negative
- MRI/MRA are also options, if available
- Formal cerebral catheter angiogram
Lumbar Puncture
- In cases with negative head CT, a strong family history of aneurysms, or ruptured aneurysms
- Consider after negative NCCT
- may aid in making an alternative diagnosis as the cause of headache (meningitis, idiopathic intracranial hypertension)
- looking for xanthochromia and RBC count
- Xanthochromia - the CSF has a yellowish appearance since blood has been broken down enzymatically and leaking bilirubin into the surrounding fluid[11]
Treatment / Management
Medical management of these patients should begin in the emergency department. In the first 24 hours, there is a very high risk of rebleeding, which can be reduced markedly by controlling blood pressure. Systolic should be kept at less than 140 mmHg.[12]
- Labetalol and nicardipine are good first-line agents.
- Nitroglycerin and nitroprusside should be avoided as they are associated with increased intracranial pressure.
Remember to control the patient's pain. It is not only the right thing to do, but adequate pain control also makes it easier to control blood pressure.
Use antiemetics as needed.
Nimodipine may be added in the first 96 hours to help decrease the degree of vasospasm.[13]
Antiseizure medications should also be initiated.
Differential Diagnosis
On the differential for saccular aneurysms exist many of the disease processes that cause headaches:
- Headache (tension, migraine, cluster)
- Meningitis
- Encephalitis
- SOL (space-occupying lesions such as tumors)
- Pituitary masses (endocrine)
- Metabolic disturbances
- Cerebral venous thrombosis
- Idiopathic intracranial hypertension
- Temporal arteritis
Prognosis
Many aneurysms never cause a patient any discomfort or sequelae.
If an aneurysm does rupture, the prognosis depends on several factors, including:
- Prior neurologic conditions
- Age
- Comorbidities
- Aneurysm location
- Time from rupture to first contact with a doctor
- Bleeding extent or grade of subarachnoid hemorrhage and (rebleeding)
- Aneurysm treatment success
- Vasospasms in the ensuing days
- Development of hydrocephalus and seizures
Twenty-five percent of patients with ruptured aneurysms do not survive the first 24 hours.
Of those who survive initially, 25 percent die from other complications in the next 6 months.[14]
Complications
- Rebleeding
- Hyponatremia
- Vasospasm
- Hydrocephalus
- Seizures
- Cardiac stress
Deterrence and Patient Education
Patients should know how to utilize the emergency medical services (EMS) available to them, such as emergency rooms, via EMS when to seek the expert advice of an emergency physician if a headache develops that is severe or different from baseline headaches.[15]
Enhancing Healthcare Team Outcomes
Currently, research is being done in a variety of fields, including targeting specific genes and improving the diagnostic accuracy of our neuroimaging such that this diagnosis can be made swiftly and accurately, thereby improving patient outcomes and decreasing the morbidity and mortality associated with saccular aneurysms, especially ones that have burst. Outcomes can be enhanced by an interprofessional team, including EMS personnel, emergency department nurses and physicians, radiologists, neurologists, physiatrists, and therapists.
Media
References
Alg VS, Sofat R, Houlden H, Werring DJ. Genetic risk factors for intracranial aneurysms: a meta-analysis in more than 116,000 individuals. Neurology. 2013 Jun 4:80(23):2154-65. doi: 10.1212/WNL.0b013e318295d751. Epub [PubMed PMID: 23733552]
Level 1 (high-level) evidenceVlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. The Lancet. Neurology. 2011 Jul:10(7):626-36. doi: 10.1016/S1474-4422(11)70109-0. Epub [PubMed PMID: 21641282]
Level 1 (high-level) evidenceEtminan N, Rinkel GJ. Unruptured intracranial aneurysms: development, rupture and preventive management. Nature reviews. Neurology. 2017 Feb 1:13(2):126. doi: 10.1038/nrneurol.2017.14. Epub [PubMed PMID: 28145447]
Chalouhi N,Hoh BL,Hasan D, Review of cerebral aneurysm formation, growth, and rupture. Stroke. 2013 Dec [PubMed PMID: 24130141]
Samuel N, Radovanovic I. Genetic basis of intracranial aneurysm formation and rupture: clinical implications in the postgenomic era. Neurosurgical focus. 2019 Jul 1:47(1):E10. doi: 10.3171/2019.4.FOCUS19204. Epub [PubMed PMID: 31261114]
Texakalidis P, Sweid A, Mouchtouris N, Peterson EC, Sioka C, Rangel-Castilla L, Reavey-Cantwell J, Jabbour P. Aneurysm Formation, Growth, and Rupture: The Biology and Physics of Cerebral Aneurysms. World neurosurgery. 2019 Oct:130():277-284. doi: 10.1016/j.wneu.2019.07.093. Epub 2019 Jul 16 [PubMed PMID: 31323409]
Yong-Zhong G, van Alphen HA. Pathogenesis and histopathology of saccular aneurysms: review of the literature. Neurological research. 1990 Dec:12(4):249-55 [PubMed PMID: 1982169]
Level 3 (low-level) evidenceAktham A, AbdulAzeez MM, Hoz SS. Surgical Intervention of Intracerebral Hematoma Caused by Ruptured Middle Cerebral Artery Aneurysm in Neurosurgery Teaching Hospital, Baghdad, Iraq. Neurology India. 2020 Jan-Feb:68(1):124-131. doi: 10.4103/0028-3886.279677. Epub [PubMed PMID: 32129261]
CROMPTON MR. Intracerebral haematoma complicating ruptured cerebral berry aneurysm. Journal of neurology, neurosurgery, and psychiatry. 1962 Nov:25(4):378-86 [PubMed PMID: 14023947]
Wu X, Chen X, Zhu J, Chen Q, Li Z, Lin A. Imaging detection of cerebral artery fenestrations and their clinical correlation with cerebrovascular diseases. Clinical imaging. 2020 Jun:62():57-62. doi: 10.1016/j.clinimag.2020.01.012. Epub 2020 Jan 15 [PubMed PMID: 32066034]
Fisher CM, Roberson GH, Ojemann RG. Cerebral vasospasm with ruptured saccular aneurysm--the clinical manifestations. Neurosurgery. 1977 Nov-Dec:1(3):245-8 [PubMed PMID: 615969]
Wang JW, Li CH, Tian YY, Li XY, Liu JF, Li H, Gao BL. Safety and efficacy of endovascular treatment of ruptured tiny cerebral aneurysms compared with ruptured larger aneurysms. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences. 2020 Jun:26(3):283-290. doi: 10.1177/1591019919897446. Epub 2020 Jan 13 [PubMed PMID: 31930939]
Nornes H, Magnaes B. Intracranial pressure in patients with ruptured saccular aneurysm. Journal of neurosurgery. 1972 May:36(5):537-47 [PubMed PMID: 5026540]
Wiebers DO, Whisnant JP, O'Fallon WM. The natural history of unruptured intracranial aneurysms. The New England journal of medicine. 1981 Mar 19:304(12):696-8 [PubMed PMID: 7464862]
Wiebers DO, Whisnant JP, Sundt TM Jr, O'Fallon WM. The significance of unruptured intracranial saccular aneurysms. Journal of neurosurgery. 1987 Jan:66(1):23-9 [PubMed PMID: 3783255]