Anatomy, Bony Pelvis and Lower Limb, Gluteus Medius Muscle
Anatomy, Bony Pelvis and Lower Limb, Gluteus Medius Muscle
Introduction
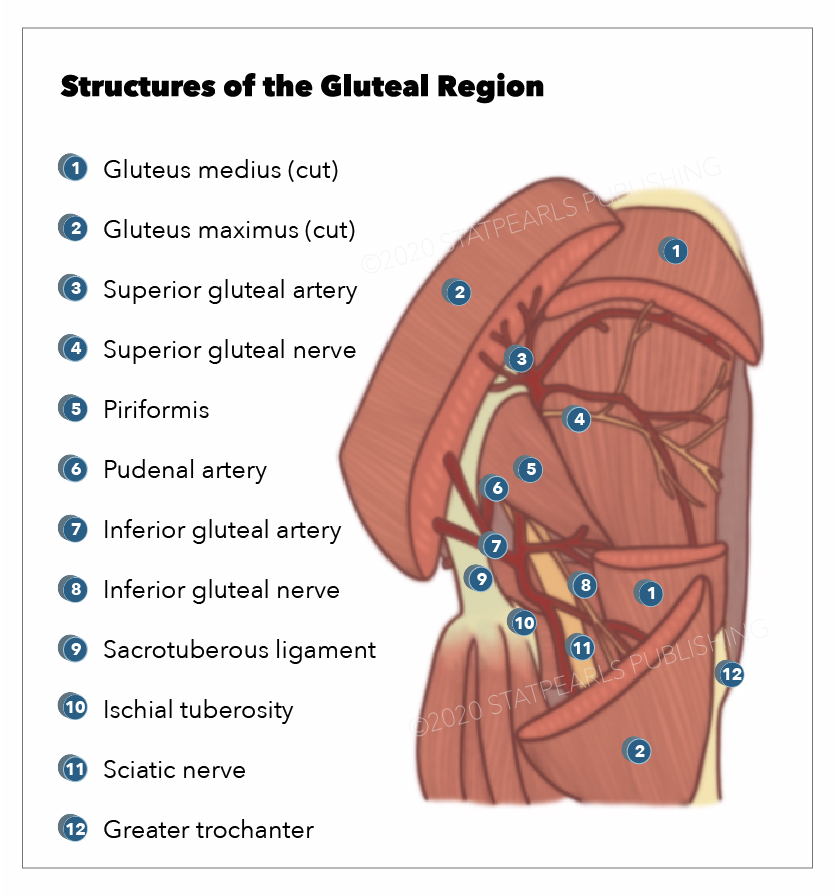
The gluteal region plays a pivotal role in the stability of the lower limb and pelvis and contains various key neurovascular structures (see Image. Structures Surrounding the Right Hip Joint). The musculature is formed principally by the three gluteal muscles: Maximus, medius, and minimus. The Gluteus medius and minimus work together as hip abductors and are vital to normal locomotion (see Image. Gluteal Region).[1] Gluteal muscle tears are common injuries, and the gluteus medius tendon is often affected. Such injuries can cause acute and chronic hip pain and may require surgical repair if refractory to medical treatment.[2]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The gluteal region, colloquially known as the buttock, lies posterior to the bony pelvis and is defined superiorly by the iliac crest and inferiorly ends at the gluteal fold. The muscles of the region consist of the gluteus maximus, medius, and minimus, as well as the piriformis, obturator internus, superior and inferior gemellus, and quadratus femoris.
The gluteus medius lies between the gluteus maximus and gluteus minimus. Its posterior third is covered by the gluteus maximus, while the anterior two-thirds is superficial, covered only by a strong layer of deep fascia.[3] Gluteus medius lies on top of the gluteus minimus, covering the minimus muscle. It is a broad muscle covering the exterior surface of the ilium between the anterior and posterior gluteal lines. The posterior fibers of the gluteus medius converge to form a flat tendon slanting downward and forward towards the superoposterior facet of the greater trochanter of the femur. The anterolateral part runs posteriorly toward the lateral facet of the greater trochanter of the femur. Both parts insert into the lateral surface of the greater trochanter of the femur via fibrocartilage.[4] The muscle tendon varies its thickness; the anterior and lateral portion merges laterally to the greater trochanter and has a lesser thickness than the posterior portion, which merges on the super-posterior area of the greater trochanter.
The gluteus medius is a primary hip abductor, assisted by the gluteus minimus and the tensor fascia lata. Both gluteus medius and minimus act from the pelvis to abduct the thigh and rotate it internally. The anterior fibers help with the internal rotation of the thigh, while the posterior fibers help with lateral rotation when the knee is in extension. Gluteus medius acts from the femur to stabilize the pelvis and maintain the trunk upright when standing on one leg, running, and walking when one leg is off the ground. With one foot being off the ground, the body weight tends to make the pelvis sag downwards on the unsupported side. The gluteus medius and minimus of the supported side counteract this force by powerful traction on the hip bone. The pelvis is prevented from sagging downwards and may even be raised a little on the unsupported side. The force produced by hip abductor muscles to maintain stability during single-limb support accounts for most of the compressive force generated between the acetabulum and femoral head.[5]
Embryology
The lower limb bud forms at around four weeks, corresponding to embryonic stage 14. By stage 17, the lower limb has a flattened footplate with an identifiable hip joint but no true knee. During stages 20 to 23, the digits separate, and the toes are clearly defined by stage 23, corresponding to the end of week eight. Like other skeletal muscles, the gluteus medius is formed by cells derived from somites present at the level of the lower limb bud. These cells demyelinate from the hypaxial edge of the dermomyotome. They subsequently migrate into the limb bud and proliferate there. With the expression of myogenic determination factors, they eventually differentiate into the gluteus medius muscle.[6]
Blood Supply and Lymphatics
The superior gluteal artery supplies the gluteus medius muscle. It is the largest branch of the internal iliac artery (see Image. Arteries of the Pelvis, Male Abdomen). The artery travels posteriorly between the first sacral ramus and the lumbosacral trunk.[7] It exits the pelvis via the greater sciatic foramen superior to the piriformis and further divides into deep and superficial branches. The deep branch passes between the gluteus medius and the surface of the bone and divides into inferior and superior branches; the superior branch inserts into the gluteus medius via 4 to 7 perforators and 0 to 2 perforators to the gluteus minimus. It anastomoses with an ascending branch of the lateral circumflex femoral artery and the deep circumflex iliac artery. The inferior branch runs obliquely through the gluteus medius and supplies it via 3 to 8 perforators and the gluteus minimus via 1 to 3 perforators.[8] It anastomoses with the lateral circumflex femoral artery. The superior gluteal artery exits the pelvis at an acute angle, which increases its vulnerability to shearing forces. The sharp fascia of the piriformis may compromise the artery during displaced fractures. Surgical procedures such as acetabular fracture surgery place the superior gluteal vessels and nerves at risk of injury.[9]
The superior gluteal artery rarely arises from the internal pudendal artery. It occasionally arises with the inferior gluteal artery directly from the internal iliac artery. Internal iliac nodes surround the branches of internal iliac vessels, which receive the lymphatic drainage of the gluteal region. The common iliac nodes receive lymphatic drainage from the internal iliac nodes, which lie around the common iliac artery. The common iliac nodes empty into the lateral aortic nodes.
The superior gluteal vein (SGV) drains blood from the gluteal region through two branches: a superficial branch and a deep branch. The superior gluteal vein runs together with the upper gluteal artery, enters the pelvis through the large ischial foramen in the supra-pyriform canal, and ends in the internal iliac vein. The superior gluteal vein anastomoses with the inferior gluteal vein.[10]
The inferior gluteal vein (IGV) drains the posterosuperior region of the thigh and buttock. It originates from double branches that converge in a single trunk that runs together with the lower gluteal artery. The inferior gluteal vein anastomoses with the medial circumflex veins of the femur and the superior perforating vein, which are tributaries of the deep femoral vein. The inferior gluteal vein enters the pelvis through the lower part of the large ischial foramen and flows into the distal portion of the internal iliac vein.
Nerves
The gluteus medius receives nerve supply from the superior gluteal nerve. The superior gluteal nerve originates from the dorsal branches of the L4, L5, and S1 nerve roots of the sacral plexus [11]. The nerve exits the pelvis through the greater sciatic foramen above the piriformis muscle and splits into inferior and superior branches. See Image. Sacral and Coccygeal Nerves.
The superior branch accompanies the upper branch of the deep division of the superior gluteal artery to innervate the gluteus minimus and gluteus medius. The inferior branch travels with the lower ramus of the deep division of the superior gluteal artery to innervate the gluteus minimus and medius, terminating in the tensor fascia lata muscle.
Surgical Considerations
The gluteus medius and its supplying artery and nerve suffer damage due to hip fracture, hip dislocation, and hip arthroplasty. In a direct lateral approach during hip arthroplasty, the gluteus medius is surgically divided to gain access to the hip joint; therefore, this approach has the highest chance of nerve damage.[12] During the percutaneous placement of iliosacral screws, which is a common technique employed to treat complicated injuries of the pelvis, the deep superior branch of the superior gluteal nerve and vessels are at significant risk even when utilizing soft tissue protecting cannulas, and the screws are appropriately placed.[13]
Gluteus medius tears can present as chronic trochanteric bursitis resistant to medical treatment, requiring surgical management. Identification of this pathology is in the first instance, typically following clinical examination, but MR imaging is also of value, demonstrating a high-intensity T2 signal secondary to the inflammation of the affected area.[14] Ultrasound assessment of gluteal tendinopathy is another diagnostic modality of value in this setting.[15] If surgery is indicated, this can be achieved endoscopically, using a trans-tendon approach to maximize visualization and repair of the gluteus medius tear, and enabling removal of greater trochanter summit, if appropriate, by motorized burr.[2] Percutaneous ultrasound tenotomy (PUT), a minimally-invasive procedure commonly used for treating elbow, knee, and ankle tendinopathies, has also been proposed to treat gluteus medius tendinopathy. Baker et al. trialed the technique in 29 patients with reported good patient satisfaction and improvement in hip clinical assessment scores.[16]
Clinical Significance
The gluteus medius and minimus can be tested together in a clinical setting by internal rotation of the thigh against resistance, with the hip and knee flexed while in a supine position. However, the presence of gluteus medius tears can be individually identified by performing an internal counter-resistance rotation test.[17] The gluteus medius and minimus, along with the tensor fascia lata, can be tested clinically by the abduction of the thigh against resistance with the knee extended while in a supine position. Both the gluteus medius and minimus act together to support the pelvis. The gluteus medius and minimus should be functioning adequately, and their innervation must be intact; the neck of the femur must be intact with its usual angulation to the shaft, and the constituents of the hip joint must be normal for the supportive effect of the gluteus medius and minimus on the pelvis when raising the contralateral foot. When either of these conditions is affected, the pelvis sinks downwards on the unsupported side when the patient stands on the affected limb, known as the Trendelenburg sign.
In cases of gluteus medius and minimus paralysis, patients will have a characteristic lurching gait known as Trendelenburg gait. If these two muscles and their innervations are intact, paralysis of other muscles acting on the hip joint will have little impact on walking or running. Greater trochanteric pain syndrome (GTPS) is attributable to tendinopathy of the gluteus medius and/or minimus with or without coexisting bursal pathology.[18] Patients commonly complain of lateral hip pain, localized to the greater trochanter, which increases with side-lying at night and weight-bearing activities.[18] The condition is diagnosed clinically by lateral hip pain with point tenderness at the greater trochanteric region. The pain increases with prolonged repetitive activity involving the gluteus medius, such as walking, running, standing on one leg, or climbing stairs. The superior gluteal nerve can incur damage during an intramuscular injection in the gluteal region. It is advisable to administer injections in the upper lateral quadrant to avoid injuring the superior gluteal and sciatic nerve, the latter of which is usually found in the lower quadrants of the gluteal region.[19]
Other Issues
Owing to the close proximity of the musculature and emerging neurovascular structures in the gluteal region, there have been case reports of compression syndrome occurring following trauma to the gluteus medius muscle, compressing the regional vascular system.[19]
Gluteus medius syndrome (GMS) is a less common cause of lower back pain or leg pain and is similar but not the same as the greater trochanteric pain syndrome. GMS is associated with degeneration of the lumbar vertebrae and osteoarthritis at the level of the hips or the knee; it can correlate with failed back surgery syndrome.[20]
Media
(Click Image to Enlarge)
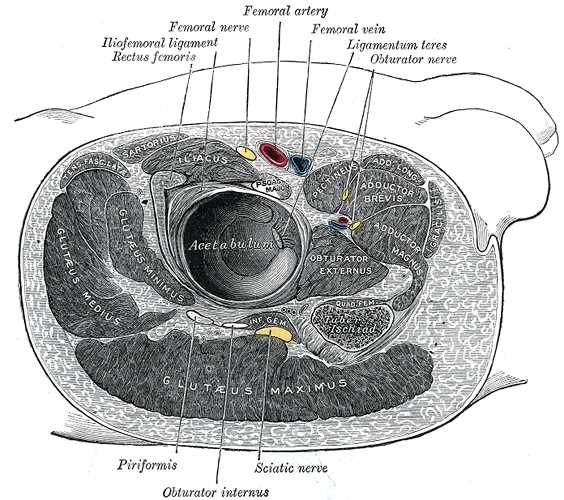
Structures Surrounding the Right Hip Joint. Structures around the right hip joint include the iliofemoral ligament, rectus femoris, femoral nerve, femoral artery, femoral vein, ligamentum teres, obturator nerve, piriformis, obturator internus, sciatic nerve, gluteus maximus, gluteus medius, gluteus minimus, acetabulum, obturator externus, iliacus, pectineus, adductor brevis, and adductor magnus.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
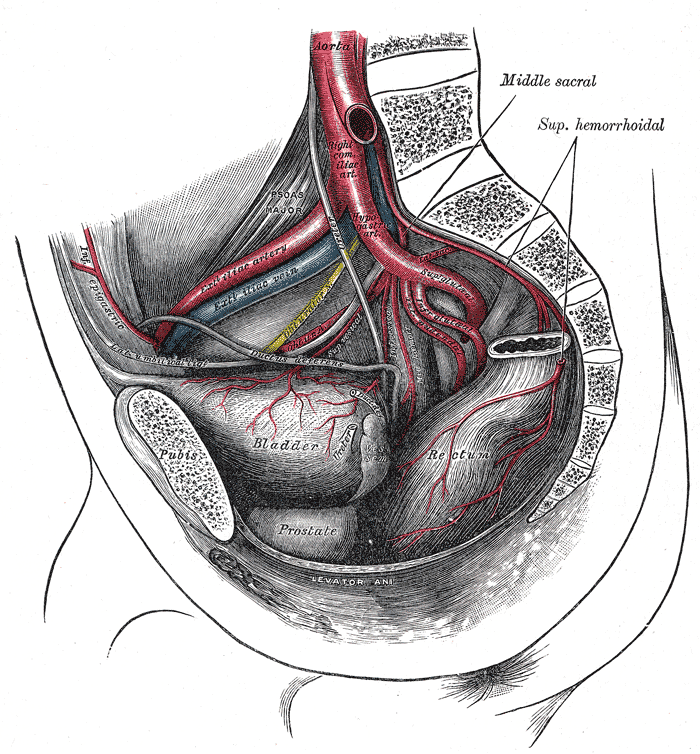
Arteries of the Pelvis, Male Abdomen. The right common iliac artery, hypogastric artery, superior gluteal artery, infra gluteal artery, inferior gluteal artery, external Iliac vein, external iliac artery, bladder, prostate, and rectum are seen in the illustration.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
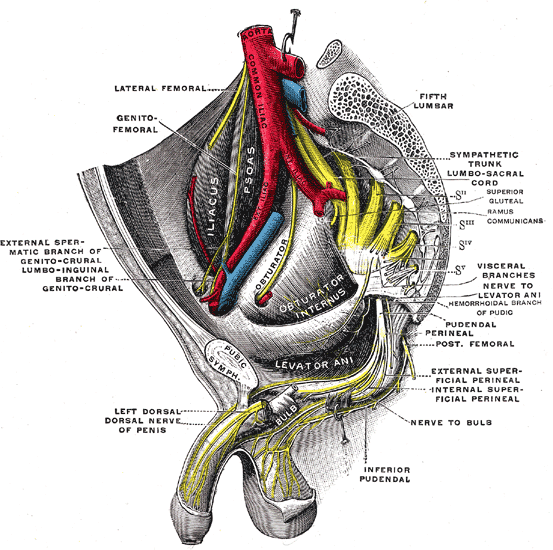
Sacral and Coccygeal Nerves. The illustration depicts the sacral plexus of the right side, pelvic area, coccyx, dorsal nerve of the penis, nerve to bulb, and genitofemoral nerve.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Magrath WJ, Qiu CS, Hanwright PJ, Tuffaha SH, Khavanin N. A Systematic Review of Muscle Synergies during a Walking Gait to Define Optimal Donor-Recipient Pairings for Lower Extremity Functional Reconstruction. Plastic and reconstructive surgery. Global open. 2022 Aug:10(8):e4438. doi: 10.1097/GOX.0000000000004438. Epub 2022 Aug 15 [PubMed PMID: 35983544]
Level 2 (mid-level) evidenceThaunat M, Chatellard R, Noël E, Sonnery-Cottet B, Nové-Josserand L. Endoscopic repair of partial-thickness undersurface tears of the gluteus medius tendon. Orthopaedics & traumatology, surgery & research : OTSR. 2013 Nov:99(7):853-7. doi: 10.1016/j.otsr.2013.06.005. Epub 2013 Sep 25 [PubMed PMID: 24075011]
Level 2 (mid-level) evidenceDa Rocha RP. Surgical anatomy of the gluteal region's subcutaneous screen and its use in plastic surgery. Aesthetic plastic surgery. 2001 Mar-Apr:25(2):140-4 [PubMed PMID: 11349305]
Tsutsumi M,Nimura A,Akita K, The Gluteus Medius Tendon and Its Insertion Sites: An Anatomical Study with Possible Implications for Gluteus Medius Tears. The Journal of bone and joint surgery. American volume. 2019 Jan 16; [PubMed PMID: 30653048]
Neumann DA. Kinesiology of the hip: a focus on muscular actions. The Journal of orthopaedic and sports physical therapy. 2010 Feb:40(2):82-94. doi: 10.2519/jospt.2010.3025. Epub [PubMed PMID: 20118525]
Buckingham M, Bajard L, Chang T, Daubas P, Hadchouel J, Meilhac S, Montarras D, Rocancourt D, Relaix F. The formation of skeletal muscle: from somite to limb. Journal of anatomy. 2003 Jan:202(1):59-68 [PubMed PMID: 12587921]
Level 3 (low-level) evidenceAnetai H, Tokita K, Kojima R, Aizawa Y, Kageyama I, Kumaki K. Variations in the course of the superior gluteal artery in relation to the lumbosacral plexus. Okajimas folia anatomica Japonica. 2017:94(2):45-54. doi: 10.2535/ofaj.94.45. Epub [PubMed PMID: 29249733]
Ahmadzadeh R,Bergeron L,Tang M,Morris SF, The superior and inferior gluteal artery perforator flaps. Plastic and reconstructive surgery. 2007 Nov; [PubMed PMID: 18040187]
Collinge CA, Ziran NM, Coons DA. Relationship Between the Superior Gluteal Vessels and Nerve at the Greater Sciatic Notch. Orthopedics. 2015 Oct:38(10):e929-33. doi: 10.3928/01477447-20151002-62. Epub [PubMed PMID: 26488790]
Turin SY, Fracol M, Keller E, Markl M, Collins J, Krochmal D, Kim JYS. Gluteal Vein Anatomy: Location, Caliber, Impact of Patient Positioning, and Implications for Fat Grafting. Aesthetic surgery journal. 2020 May 16:40(6):642-649. doi: 10.1093/asj/sjz260. Epub [PubMed PMID: 31574144]
Ray B, D'Souza AS, Saxena A, Nayak D, Sushma RK, Shetty P, Pugazhendi B. Morphology of the superior gluteal nerve: a study in adult human cadavers. Bratislavske lekarske listy. 2013:114(7):409-12 [PubMed PMID: 23822627]
Eksioglu F,Uslu M,Gudemez E,Atik OS,Tekdemir I, Reliability of the safe area for the superior gluteal nerve. Clinical orthopaedics and related research. 2003 Jul; [PubMed PMID: 12838060]
Collinge C, Coons D, Aschenbrenner J. Risks to the superior gluteal neurovascular bundle during percutaneous iliosacral screw insertion: an anatomical cadaver study. Journal of orthopaedic trauma. 2005 Feb:19(2):96-101 [PubMed PMID: 15677925]
Cvitanic O, Henzie G, Skezas N, Lyons J, Minter J. MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus). AJR. American journal of roentgenology. 2004 Jan:182(1):137-43 [PubMed PMID: 14684527]
Level 2 (mid-level) evidenceKong A, Van der Vliet A, Zadow S. MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome. European radiology. 2007 Jul:17(7):1772-83 [PubMed PMID: 17149624]
Baker CL Jr,Mahoney JR, Ultrasound-Guided Percutaneous Tenotomy for Gluteal Tendinopathy. Orthopaedic journal of sports medicine. 2020 Mar [PubMed PMID: 32232066]
Ortiz-Declet V, Chen AW, Maldonado DR, Yuen LC, Mu B, Domb BG. Diagnostic accuracy of a new clinical test (resisted internal rotation) for detection of gluteus medius tears. Journal of hip preservation surgery. 2019 Dec:6(4):398-405. doi: 10.1093/jhps/hnz046. Epub 2019 Nov 14 [PubMed PMID: 32015892]
Speers CJ, Bhogal GS. Greater trochanteric pain syndrome: a review of diagnosis and management in general practice. The British journal of general practice : the journal of the Royal College of General Practitioners. 2017 Oct:67(663):479-480. doi: 10.3399/bjgp17X693041. Epub [PubMed PMID: 28963433]
Thompson AR, Ensrud ER. Superior gluteal nerve injury following landmark-guided corticosteroid injection for greater trochanteric pain: A case report. Clinical case reports. 2020 Dec:8(12):2554-2556. doi: 10.1002/ccr3.3202. Epub 2020 Aug 9 [PubMed PMID: 33363778]
Level 3 (low-level) evidenceKameda M, Tanimae H, Kihara A, Matsumoto F. Does low back pain or leg pain in gluteus medius syndrome contribute to lumbar degenerative disease and hip osteoarthritis and vice versa? A literature review. Journal of physical therapy science. 2020 Feb:32(2):173-191. doi: 10.1589/jpts.32.173. Epub 2020 Feb 14 [PubMed PMID: 32158082]