Introduction
Chondroblastoma is a benign, chondroid-producing neoplasm composed of chondroblasts. It accounts for less than 1% of all bone tumors and usually arises in the epiphyses or apophysis of skeletally immature patients.[1] Jaffe et al. proposed the term "chondroblastoma," noting the immature chondroid cells and poorly formed matrix.[2] These neoplasms usually occur in the long bones and are important, considering both benign and malignant etiologies in the differential diagnosis. The proximal humerus is the most common site of involvement, followed by the distal femur and proximal femur.[3] Chondroblastomas require surgical treatment. In general, chondroblastoma has a good prognosis, and patients often experience full resolution after surgical treatment.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact etiology to include the genetics and environmental factors that predispose patients to the formation of these neoplasms is not well understood. Although researchers have not yet observed a single chromosomal breaking point, they have described various abnormalities at 2q35, 3q21-23, 8q21, 18q21, p53, chromosome 5, 8, 11, 17 in the literature. [4][5][6][7]
Epidemiology
Chondroblastoma is a rare benign neoplasm, accounting for less than 1% of all primary bone tumors. Most chondroblastomas are diagnosed in the second to third decade of life (mean age, 19 to 23 years) with a male predominance (2 to 1).[1] More than 75% of cases involve the long bones; the most common anatomical sites are the epiphyseal regions of the proximal and distal femur, proximal tibia, and proximal humerus.[8][9] Rarely clinicians will encounter them in flat bones as or the bones of the hands and feet.[10] Chondroblastomas almost invariably involve a single bone.
Pathophysiology
Histogenesis:
The histogenesis of chondroblastomas remains controversial. Possible proposed cells of origin include cartilage germ cells or epiphyseal cartilage cells.[10] A possible multipotent mesenchymal cell or tendon sheath synovial cell origin is another proposed etiological site. [11]
Genetics:
Flow cytometric studies reveal that most chondroblastomas are diploid with low proliferation fractions.[12][13] There are reports of clonal abnormalities in 14 chondroblastomas.[14] Heterogeneous rearrangements of chromosomes 5 and 8, both balanced and unbalanced, appear to be the most common. IDH1 and IDH2 mutations are absent.[5] Recently, research has shown that chondroblastomas have distinctive driver mutations in the genes that encode histone H3.3. Chondroblastomas harbor mutations in the H3F3B gene far more commonly than the H3F3A gene.[15] Research has found an antibody directed against the H3F3 K36M mutation to be specific for chondroblastoma.[16]
Histopathology
Macroscopic findings:
Grossly, chondroblastomas appear as multiple pinkish-tan soft tissue fragments that may exhibit areas of calcification, hemorrhage, or cystic changes.
Histopathological findings:
Histologically, a chondroblastoma characteristically presents with a sheet-like proliferation of small to intermediate-sized round polygonal cells.[1] These cells have well-defined cytoplasmic borders, clear to slightly basophilic cytoplasm, and round to ovoid nucleus (chondroblasts). They often exhibit longitudinal grooves and one or more small or inconspicuous nucleoli. Randomly distributed osteoclast-type giant cells are almost always present. Variably-sized nodules of amorphous to eosinophilic material (chondroid) accompany the chondroblasts. Mature hyaline cartilage is relatively uncommon. A fine network of pericellular ''chicken wire'' calcifications is characteristic. Recurrent chondroblastomas may show cytological atypia, which the clinician should not interpret as a sign of malignant transformation.
Immunohistochemical findings:
Immunohistochemically, the chondroblasts are positive for vimentin, neuron-specific enolase, and S100 protein.[1] Sox9 is a transcriptional factor that shows positivity in chondroblastomas.[17] DOG1 is a useful marker that helps to distinguish chondroblastoma from other giant cell-containing bone tumors.[18] Observable positivity for keratins, namely 8, 18, and 19 and p63, is frequently in evidence.[19]
History and Physical
Clinical complaints are often nonspecific.[3] Symptoms are typically present for many months before the patient seeks medical attention. They include[9]:
- Insidious onset of bone pain: the most common
- Other nonspecific complaints: local swelling, joint stiffness and/or effusion, and the development of a limp
- In tumors arising from the skull bones: seizures and progressive hearing loss can also occur
Physical examination of patients with chondroblastoma can disclose the following findings[1]:
- Local tenderness
- Joint effusion
- Decreased range of motion in the affected joint
- Muscular atrophy
- Rarely: a palpable mass
Evaluation
Several imaging modalities are available for establishing the diagnosis of chondroblastoma. They include:
- Plain radiographs
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
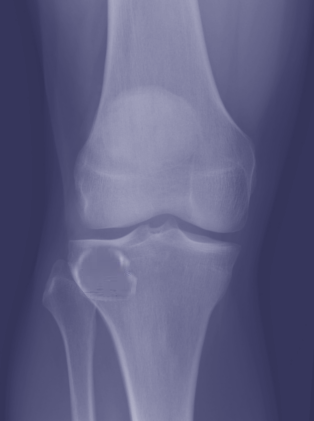
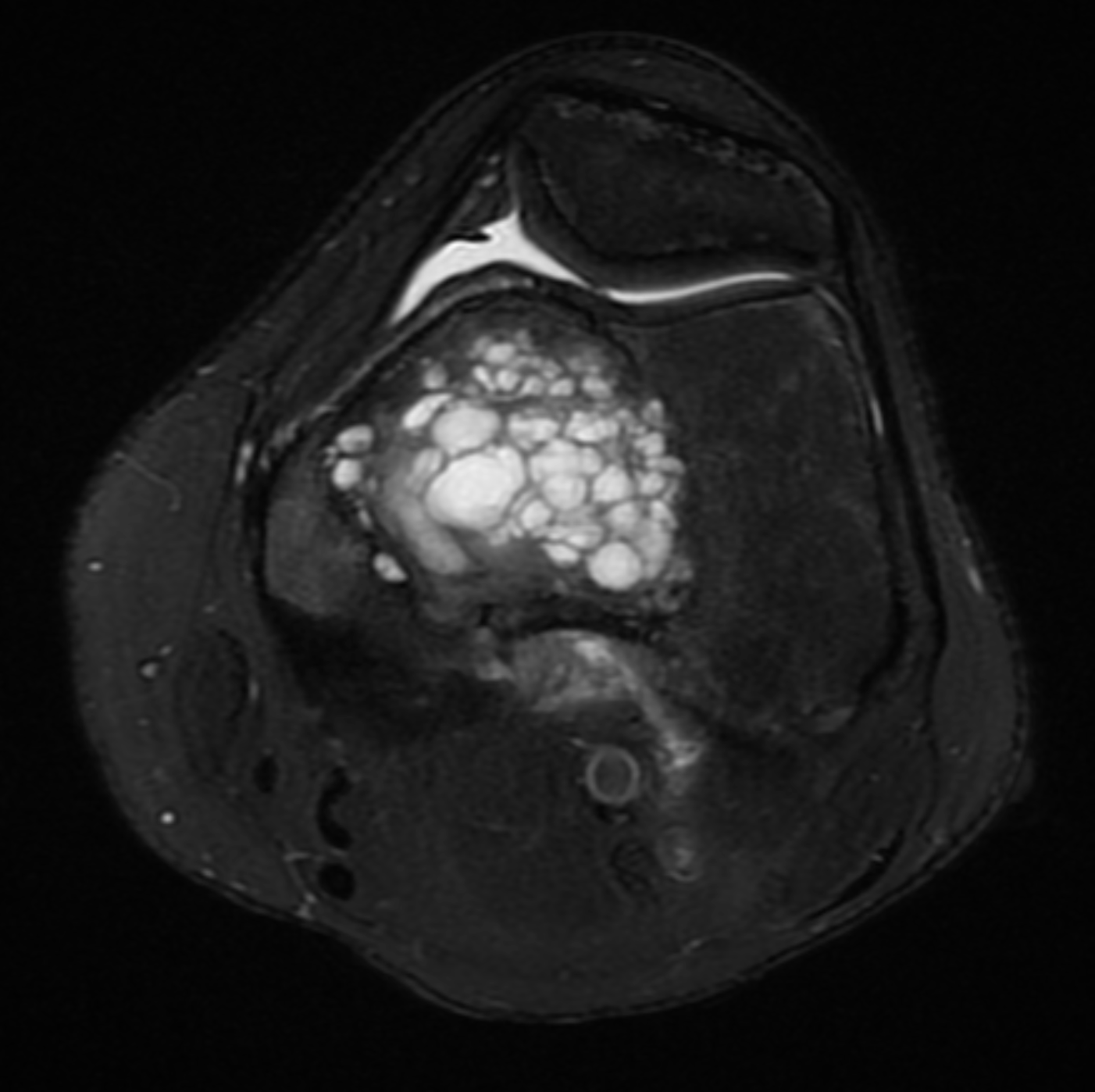
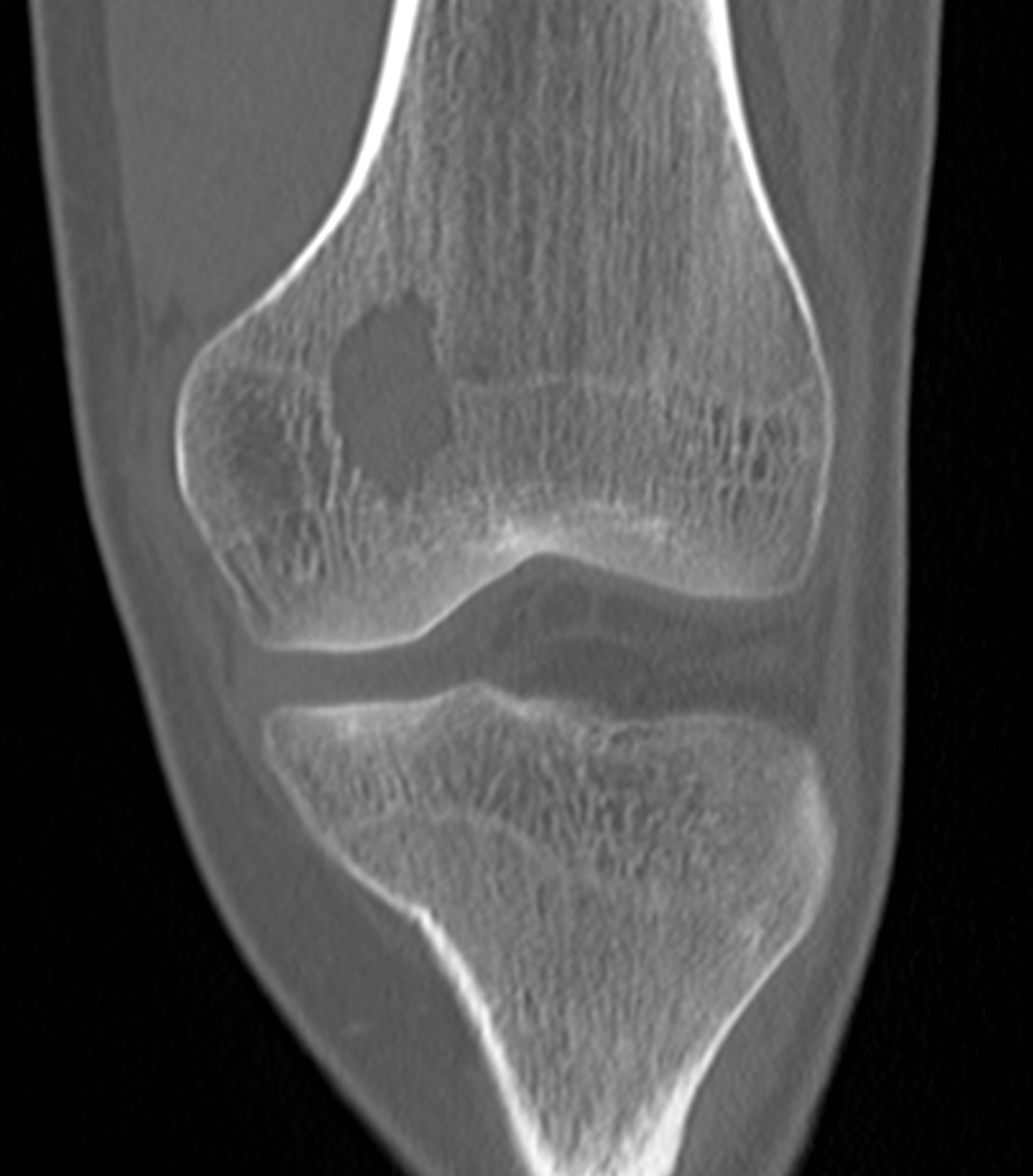
A well-demarcated eccentric and lytic lesion with a thin rim of sclerotic bone is the typical radiologic presentation of chondroblastomas. Chondroblastomas are relatively small (3 to 6 cm) and occupy less than half of the epiphysis. There is generally no expansion of the bone.
Plain radiographs:
Plain radiographs show a fuzzy, round-to-oval, well-delineated lesion with a sclerotic rim.[20]
Computed tomography:
Computed tomography can demonstrate calcifications that are not detectable on plain radiographs. It can depict cortical erosion, matrix mineralization, and soft tissue extension.[21]
Magnetic resonance imaging:
In chondroblastomas, MRI demonstrates extensive edema surrounding the lesion. The signal intensity on T1- and T2-weighted MRI images depends on the levels of various components within the lesion. Most cases show variable intensity on T2-weighted images.[22]
Treatment / Management
The treatment of choice of chondroblastoma is surgical. It consists of complete surgical curettage with or without bone grafting, en bloc resection, or rarely, amputation. Surgical resection alleviates pain, avoids propagation into the joint and adjacent soft tissues, diminishes the likelihood of recurrence, and accurately establishes the diagnosis of chondroblastomas. Surgical management depends on[23][24]:(B3)
- The extent of bone and/or joint involvement
- Anatomic location of the lesion
- Staging
Stage 1 (latent) or stage 2 (active) may be an indication for intralesional excision.
Stage 3 (aggressive) is an indication of marginal or wide resection.[24](B3)
Adjunctive therapy includes chemical cauterization with phenol or cryosurgery. Bone grafting and cryotherapy after surgical curettage decrease the risk of recurrence.[1] Some authors suggest that radiofrequency should be an option as an alternative treatment method in managing chondroblastomas.[10] There is no definite role for adjuvant chemotherapy or radiotherapy. For recurrent tumors, resection remains the treatment of choice.[1](B3)
Differential Diagnosis
The differential diagnosis for chondroblastomas chiefly includes other epiphyseal lesions. These include:
- Giant cell tumor of bone
- Geode or intraosseous ganglion
- Clear cell chondrosarcoma
- Osteomyelitis
Other differentials that are possible include:
- Osteosarcoma
- Osteoblastoma
- Brown tumor
- Osteoid osteoma
- Aneurysmal bone cyst
Toxicity and Adverse Effect Management
The complications of surgical treatment include[10]:
- Damage of the articular cartilage or even an open growth plate
- Recurrence in surgically treated patients
- Hematoma
- Infection
- Fracture
- Limb-length discrepancy
Prognosis
If left untreated, chondroblastoma does not undergo spontaneous regression. Recurrence rates of chondroblastomas range from 8.3% to 21.4% and may be explainable by retained tumor material during surgery.[25][26] The risk of recurrence increases in case of inadequate surgery, location in the hip and pelvis, young age, and aneurysmal bone cyst components.[27] Rarely, pulmonary metastases occur from histologically benign chondroblastomas. However, these metastases are clinically nonprogressive and treatable by surgical resection or simple observation.[28] Malignant transformation of a chondroblastoma is extremely rare. There are no reliable histological parameters capable of predicting more aggressive behavior.
Complications
The most common complication associated with chondroblastoma is local recurrence after surgery. Patients require long term monitoring post-surgery for any recurrence of the tumor.[29][26] Pathological fractures can also occur. Rarely, a malignant transformation may take place, as documented in a few case reports.[30][31]
Consultations
- Orthopedics: treatment for chondroblastoma almost always involves surgery with intralesional curettage and packing.
Deterrence and Patient Education
Chondroblastoma is mostly a benign bone tumor, and patients and their families need education on how to recognize the early signs and symptoms of bone tumors. Patients with signs of bone pain, swelling of bones or joints, any palpable mass found on the bones, fractures not associated with trauma should seek early intervention. Treatment for chondroblastoma is predominantly surgical. Prognosis is usually good once treated. Local recurrence can occur after surgery, and rarely malignant transformation has been reported. Long term follow-up is necessary to monitor these patients closely. The interdisciplinary team includes orthopedics, oncologists, and specialty care nurses. Prompt diagnosis by primary providers with a referral for treatment is paramount. Specialty trained nurses in orthopedics assist in coordinating care, monitoring patients, arrange for follow up, and report problems to the team.
Enhancing Healthcare Team Outcomes
Chondroblastoma is ideally managed by an interprofessional team that consists of orthopedists, radiologists, and pathologists. Correlation between gross, radiographic, and microscopic features of the lesion is crucial to establish the definitive diagnosis of chondroblastoma. Postoperatively, patients require long term follow-up due to the possibility of tumor recurrence.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Chen W, DiFrancesco LM. Chondroblastoma: An Update. Archives of pathology & laboratory medicine. 2017 Jun:141(6):867-871. doi: 10.5858/arpa.2016-0281-RS. Epub [PubMed PMID: 28557595]
Jaffe HL, Lichtenstein L. Benign Chondroblastoma of Bone: A Reinterpretation of the So-Called Calcifying or Chondromatous Giant Cell Tumor. The American journal of pathology. 1942 Nov:18(6):969-91 [PubMed PMID: 19970672]
Dahlin DC, Ivins JC. Benign chondroblastoma. A study of 125 cases. Cancer. 1972 Aug:30(2):401-13 [PubMed PMID: 5051664]
Level 3 (low-level) evidenceDe Mattos CB, Angsanuntsukh C, Arkader A, Dormans JP. Chondroblastoma and chondromyxoid fibroma. The Journal of the American Academy of Orthopaedic Surgeons. 2013 Apr:21(4):225-33. doi: 10.5435/JAAOS-21-04-225. Epub [PubMed PMID: 23545728]
Sjögren H, Orndal C, Tingby O, Meis-Kindblom JM, Kindblom LG, Stenman G. Cytogenetic and spectral karyotype analyses of benign and malignant cartilage tumours. International journal of oncology. 2004 Jun:24(6):1385-91 [PubMed PMID: 15138578]
Swarts SJ, Neff JR, Johansson SL, Nelson M, Bridge JA. Significance of abnormalities of chromosomes 5 and 8 in chondroblastoma. Clinical orthopaedics and related research. 1998 Apr:(349):189-93 [PubMed PMID: 9584382]
Level 3 (low-level) evidenceOstrowski ML, Johnson ME, Truong LD, Hicks MJ, Smith FE, Spjut HJ. Malignant chondroblastoma presenting as a recurrent pelvic tumor with DNA aneuploidy and p53 mutation as supportive evidence of malignancy. Skeletal radiology. 1999 Nov:28(11):644-50 [PubMed PMID: 10591928]
Level 3 (low-level) evidenceBloem JL, Mulder JD. Chondroblastoma: a clinical and radiological study of 104 cases. Skeletal radiology. 1985:14(1):1-9 [PubMed PMID: 4023729]
Level 3 (low-level) evidenceTurcotte RE, Kurt AM, Sim FH, Unni KK, McLeod RA. Chondroblastoma. Human pathology. 1993 Sep:24(9):944-9 [PubMed PMID: 8253461]
Petsas T, Megas P, Papathanassiou Z. Radiofrequency ablation of two femoral head chondroblastomas. European journal of radiology. 2007 Jul:63(1):63-7 [PubMed PMID: 17482405]
Level 3 (low-level) evidenceBrien EW, Mirra JM, Ippolito V. Chondroblastoma arising from a nonepiphyseal site. Skeletal radiology. 1995 Apr:24(3):220-2 [PubMed PMID: 7610417]
Level 3 (low-level) evidenceel-Naggar AK, Hurr K, Tu ZN, Teague K, Raymond KA, Ayala AG, Murray J. DNA and RNA content analysis by flow cytometry in the pathobiologic assessment of bone tumors. Cytometry. 1995 Mar 1:19(3):256-62 [PubMed PMID: 7736870]
Tarkkanen M, Nordling S, Böhling T, Kivioja A, Karaharju E Szymanska J, Elomaa I, Knuutila S. Comparison of cytogenetics, interphase cytogenetics, and DNA flow cytometry in bone tumors. Cytometry. 1996 Sep 15:26(3):185-91 [PubMed PMID: 8889389]
Mark J, Wedell B, Dahlenfors R, Grepp C, Burian P. Human benign chondroblastoma with a pseudodiploid stemline characterized by a complex and balanced translocation. Cancer genetics and cytogenetics. 1992 Jan:58(1):14-7 [PubMed PMID: 1728944]
Level 3 (low-level) evidenceBehjati S, Tarpey PS, Presneau N, Scheipl S, Pillay N, Van Loo P, Wedge DC, Cooke SL, Gundem G, Davies H, Nik-Zainal S, Martin S, McLaren S, Goodie V, Robinson B, Butler A, Teague JW, Halai D, Khatri B, Myklebost O, Baumhoer D, Jundt G, Hamoudi R, Tirabosco R, Amary MF, Futreal PA, Stratton MR, Campbell PJ, Flanagan AM. Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nature genetics. 2013 Dec:45(12):1479-82. doi: 10.1038/ng.2814. Epub 2013 Oct 27 [PubMed PMID: 24162739]
Level 2 (mid-level) evidenceAmary MF, Berisha F, Mozela R, Gibbons R, Guttridge A, O'Donnell P, Baumhoer D, Tirabosco R, Flanagan AM. The H3F3 K36M mutant antibody is a sensitive and specific marker for the diagnosis of chondroblastoma. Histopathology. 2016 Jul:69(1):121-7. doi: 10.1111/his.12945. Epub 2016 Mar 21 [PubMed PMID: 26844533]
Konishi E, Nakashima Y, Iwasa Y, Nakao R, Yanagisawa A. Immunohistochemical analysis for Sox9 reveals the cartilaginous character of chondroblastoma and chondromyxoid fibroma of the bone. Human pathology. 2010 Feb:41(2):208-13. doi: 10.1016/j.humpath.2009.07.014. Epub 2009 Oct 3 [PubMed PMID: 19801163]
Akpalo H, Lange C, Zustin J. Discovered on gastrointestinal stromal tumour 1 (DOG1): a useful immunohistochemical marker for diagnosing chondroblastoma. Histopathology. 2012 Jun:60(7):1099-106. doi: 10.1111/j.1365-2559.2011.04152.x. Epub 2012 Feb 15 [PubMed PMID: 22335248]
Semmelink HJ, Pruszczynski M, Wiersma-van Tilburg A, Smedts F, Ramaekers FC. Cytokeratin expression in chondroblastomas. Histopathology. 1990 Mar:16(3):257-63 [PubMed PMID: 1692005]
Clapper AT, DeYoung BR. Chondroblastoma of the femoral diaphysis: report of a rare phenomenon and review of literature. Human pathology. 2007 May:38(5):803-6 [PubMed PMID: 17306329]
Level 3 (low-level) evidenceYang J, Tian W, Zhu X, Wang J. Chondroblastoma in the long bone diaphysis: a report of two cases with literature review. Chinese journal of cancer. 2012 May:31(5):257-64. doi: 10.5732/cjc.011.10402. Epub 2012 Mar 27 [PubMed PMID: 22464651]
Level 3 (low-level) evidenceOxtoby JW, Davies AM. MRI characteristics of chondroblastoma. Clinical radiology. 1996 Jan:51(1):22-6 [PubMed PMID: 8549042]
Level 2 (mid-level) evidenceÖzer D, Arıkan Y, Gür V, Gök C, Akman YE. Chondroblastoma: An evaluation of the recurrences and functional outcomes following treatment. Acta orthopaedica et traumatologica turcica. 2018 Nov:52(6):415-418. doi: 10.1016/j.aott.2018.07.004. Epub 2018 Sep 22 [PubMed PMID: 30249436]
Angelini A, Arguedas F, Varela A, Ruggieri P. Chondroblastoma of the Foot: 40 Cases From a Single Institution. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2018 Nov-Dec:57(6):1105-1109. doi: 10.1053/j.jfas.2018.05.005. Epub [PubMed PMID: 30368424]
Level 3 (low-level) evidenceLin PP, Thenappan A, Deavers MT, Lewis VO, Yasko AW. Treatment and prognosis of chondroblastoma. Clinical orthopaedics and related research. 2005 Sep:438():103-9 [PubMed PMID: 16131877]
Level 2 (mid-level) evidenceAtalar H, Basarir K, Yildiz Y, Erekul S, Saglik Y. Management of chondroblastoma: retrospective review of 28 patients. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2007 Jul:12(4):334-40 [PubMed PMID: 17657552]
Level 2 (mid-level) evidenceHapa O, Karakaşlı A, Demirkıran ND, Akdeniz O, Havitçioğlu H. Operative treatment of chondroblastoma: a study of 11 cases. Acta orthopaedica Belgica. 2016 Mar:82(1):68-71 [PubMed PMID: 26984656]
Level 3 (low-level) evidenceRiddell RJ, Louis CJ, Bromberger NA. Pulmonary metastases from chondroblastoma of the tibia. Report of a case. The Journal of bone and joint surgery. British volume. 1973 Nov:55(4):848-53 [PubMed PMID: 4766191]
Level 3 (low-level) evidenceSailhan F, Chotel F, Parot R, SOFOP. Chondroblastoma of bone in a pediatric population. The Journal of bone and joint surgery. American volume. 2009 Sep:91(9):2159-68. doi: 10.2106/JBJS.H.00657. Epub [PubMed PMID: 19723993]
Level 2 (mid-level) evidenceDuttaluri R, Sultanpurkar GP, Raorane H, Vikram H. Malignant chondroblastoma of extraskeletal origin. International journal of applied & basic medical research. 2016 Apr-Jun:6(2):146-8. doi: 10.4103/2229-516X.179028. Epub [PubMed PMID: 27127749]
Kyriakos M, Land VJ, Penning HL, Parker SG. Metastatic chondroblastoma. Report of a fatal case with a review of the literature on atypical, aggressive, and malignant chondroblastoma. Cancer. 1985 Apr 15:55(8):1770-89 [PubMed PMID: 3978565]
Level 3 (low-level) evidence